1. Introduction
Calcium hydroxide has been used by dentists in the clinical practice for over a century [1] . In 1920, Herman introduced calcium hydroxide to dentistry as a pulp-capping material but today it is used widely in the field of endodontics [2] [3] .
Calcium hydroxide is a white odourless powder with the chemical formula Ca(OH)2 and a molecular weight of 7.08. Chemically, it is classified as a strong base in contact with aqueous fluids (its pH is about 12.5 - 12.8), and dissociate into calcium and hydroxyl ions [4] . Calcium hydroxide is used and supplied in various forms. It is used like a varnish when supplied as a liquid containing calcium hydroxide suspended in a solvent or when supplied as a paste in which calcium hydroxide is suspended in methylcellulose. Another form of calcium hydroxide is marketed as a base and a catalyst. By using the catalyst, calcium hydroxide reacts faster and forms a hard, amorphous compound within matter of minute in the oral environment. Finally, calcium hydroxide supplied as a paste contains a polymer resin that can be hardened when exposed to illumination from a handheld blue light source [2] .
Nowadays, calcium hydroxide is widely used in the field of endodontics due to its advantages such as:
・ Initially bactericidal effect then bacteriostatic.
・ Promotes healing and repair.
・ High pH stimulates fibroblasts.
・ Stops internal resorption.
・ Neutralizes low pH of acids.
・ Inexpensive and easy to use [5] .
On the other hand, calcium hydroxide has some disadvantages such as:
・ Does not exclusively stimulate dentinogenesis.
・ Does exclusively stimulate reparative dentin.
・ Associated with primary tooth resorption.
・ May dissolve after one year with cavosurface dissolution.
・ Degrades upon tooth flexure.
・ Marginal failure with amalgam condensation.
・ Does not adhere to dentin or resin restoration [5] .
The purpose of this literature review is to focus on the role of calcium hydroxide in the field of endodontics including a brief explanation of its mechanism of action, antimicrobial effects, different applications, cytotoxicity or biocompatibility, and finally removal of calcium hydroxide from the root canals.
2. Materials and Methods
3. Antimicrobial Effect of Calcium Hydroxide
Endodontic infections occur as a result of microbial mixtures containing bacteria represented by Enterococcus faecalis [6] and fungi which are especially represented by Candida Albicans [7] . Anaerobic bacteria with their endotoxins on their cell walls also predominant in this microbial diversity and can be detected especially gram negative [8] . It is well established that the complete removal of bacteria from the root canal system is difficult even with the new endodontic techniques. Combining procedures to eliminate bacterial infection may be accepted. These including mechanical root canal debridement by proper shaping, irrigation by chemical agents such as sodium hypochlorite (NaOCl) or hydrogen peroxide (H2O2) in addition to the intracanal medicament containing antimicrobial agents such as calcium hydroxide [9] [10] .
3.1. Mechanism of Action
The release of hydroxyl ions in an aqueous environment is essential for the activation of calcium hydroxide against microbes. These ions reacted intensively with several biomolecules due to their highly oxidant free radicals. As this reactivity is unspecified, the free radicals most likely gathered at the sites of generation. Hydroxyl ions have fatal effects on bacterial cells. They may damage the cytoplasmic membrane of bacteria, denature their proteins, or damage the DNA. It is difficult to prove which of these three
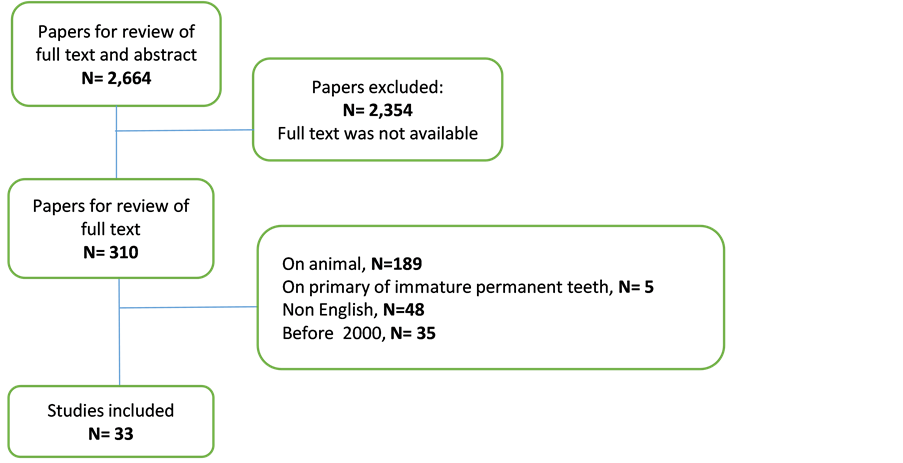
Diagram 1. Article screening process.
mechanisms is mainly involved in the death of bacterial cells after their exposure to a strong base. Since enzymatic sites are located in the cytoplasmic membrane of bacteria, hydroxyl ions from calcium hydroxide exert their mechanism of action there. Extracellular enzymes favor digestion, and through hydrolysis act on nutrients, carbohydrates, proteins, and lipids, whereas intracellular enzymes act on the respiratory activity of the cellular wall structure.
The high concentration of hydroxyl ions from calcium hydroxide alters the pH gradient of the cytoplasmic membrane damaging its protein. The integrity of the cytoplasmic membrane is altered by the high alkalinity of calcium hydroxide by acting on the organic components and transporting the nutrients or by a saponification reaction in which the phospholipids or unsaturated fatty acids of the cytoplasmic membrane are destructed during the peroxidation process [11] .
3.2. Antibacterial Effect
The antibacterial activity of calcium hydroxide is a major concern to most of the scientists. Cook et al. evaluated the quality of root canal filling with or without calcium hydroxide application prior to the root canal filling or 2% chlorhexidine on the persistence of bacterial infection on the dentinal tubules, they found that the use of 2% chlor- hexidine followed by root canal filling was more effective in removing the bacterial infection especially E. faecalis than placement of calcium hydroxide or immediate canal filling [12] . Peters et al. claimed that the number of positive gram bacteria increased in root canal system after dressing with calcium hydroxide [13] . Other studies showed that calcium hydroxide could not reliably remove bacteria from the root canal system or change the culture from gram-negative to gram-positive [14] . It has been reported that the 7 days application of calcium hydroxide is effective in bacterial elimination while the 10 minutes application was not effective [11] .
3.3. Antifungal Effect
The presence of Fungi represented by C. albicans was detected in primary root canal infection but is more common in failed endodontic treatments. Their occurrence varies between 1% and 17%.
It was reported that C. albicans cells are more resistant to calcium hydroxide than did E. faecalis. Since C. albicans survives at a wide range of pH values, high pH of calcium hydroxide may not have any effect on C. albicans. Additionally, calcium hydroxide pastes provide Ca2+ ions that are essential for the growth of C. albicans which explained the limited or no effect of calcium hydroxide to fungal infection [11] .
4. Applications of Calcium Hydroxide in Endodontics
4.1. Intracanal Medicaments
Endodontic treatment requires the use of suitable intracanal medicaments that simultaneously eliminate bacteria, prevent their growth, stop their ingress and cut off their nutrient supply [15] . Calcium hydroxide is most commonly used as an intracanal medicament for disinfection of the root canal system [2] . As mentioned above, the application of calcium hydroxide paste at intervals of at least 7 days is able to eliminate and/or reduce the total number of bacteria surviving even after biomechanical preparation [11] . It has a wide range of antimicrobial activity against bacteria, but has limited effect against E. faecalis and C. albicans. It is also an effective anti-endotoxin agent [2] . Calcium hydroxide has a little or no effect on the intensity or severity of postoperative pain following endodontic treatment. In contrast, application of corticosteroid paste in the canal reduces the postoperative pain [16] . The Effect of calcium hydroxide on pro-Inflammatory cytokines was studied and concluded that it leads to denaturation of these pro-inflammatory mediators such as interleukin-1α (IL-1α), tumor necrosis factorα (TNFα) and calcitonin gene-related peptide (CGRP) that is a potential mechanism by which calcium hydroxide contributes to the resolution of periradicular periodontitis [17] . Different techniques can be used for the placement of calcium hydroxide in the canals. Tan et al. compared the use of syringe and #25 finger spreader (group 1), syringe and #4 rotary lentulo spiral (group 2), specially designed paste carrier (group 3), they found that, the specially designed paste carrier was more effective than other tested techniques in the intracanal placement of calcium hydroxide [18] .
4.2. Root Canal Sealer
The main objective of root canal obturation is to achieve a tight seal of the root canal system which in turn enhance the healing process of periapical and apical regions after endodontic therapy [19] .
It is well clear that some forms of cement are required when filling the root canals to fill the minor spaces between the core material and the dentinal walls of the canal to prevent leakage. The outcome of endodontic treatment may influenced by sealer selection [2] . The properties of an ideal root canal sealer were outlined by Grossman (Table 1) [20] . The dissociation of calcium hydroxide into Ca++ and OH− is necessary for its therapeutic effect. Therefore, dissolving an endodontic sealer based on calcium hydroxide resulted in the loss of its solid content and consequently obturation voids are formed [2] . The antibacterial activity of some calcium hydroxide based sealers such as RealSeal, Sealapex, Apexit, and Apexit Plus is related to the release of hydroxyl ions. These sealers may also help in the formation of root-end hard tissue. Despite their advantages, calcium hydroxide-based sealers exhibit some disadvantages such as limited antibacterial activity, poor cohesive strength, greater solubility, and marginal leakage [1] [21] .
4.3. In Weeping Canal
Weeping canal is a canal from which constant clear or reddish exudation is appeared. This exudate is associated with a large apical radiolucency. The tooth is difficult to treat as when opened, exudate stops but it again reappears in next appointment. Signs and symptoms are varies from symptomless to tenderness to percussion and palpation. Obturation of canals with exudates is contraindicated.
![]()
Table 1. Requirements and characteristics for root canal sealer―Grossman (1982).
For such teeth, application of calcium hydroxide in the canal after drying with sterile absorbent paper points is helpful. This is because of its high alkalinity, which changes the acidic pH of periapical tissues to a more basic environment [2] [5] . Two other mechanisms have also been proposed: 1) build up bone in the lesion due to the calcifying potential of calcium hydroxide and 2) the residual chronically inflamed tissue is cauterized by the caustic action of calcium hydroxide [4] .
4.4. Perforation Management
One of procedural errors that can happen during root canal treatment is root or furcation perforation. This error can cause failure of the treatment and subsequent tooth loss. Calcium hydroxide was one of the most preferred materials that have been used to seal and manage perforations. It has many advantages in this treatment modality such as stimulation of hard tissue formation, easy preparation, rapid resorption when extruded into the periodontium and healing enhancement of damaged periodontal tissues [4] . In case of crestal and furcation perforations, calcium hydroxide is not the suitable material for the seal as a pocket is formed due initial inflammatory response to these materials and subsequent breakdown of the supporting tissues. Although calcium hydroxide possesses disadvantages-as mentioned previously, calcium hydroxide has been recommended as a traditional agent to manage perforations, and its usage still indicated to control infection, stop bleeding and as a temporary solution when inadequate time is available to perform a permanent repair. However, mineral trioxide aggregate (MTA) now is the material of choice for the permanent repair of perforations from both a conventional and surgical approach [4] [21] .
4.5. Role in Root Resorption
Root resorption can be classified into internal, external or root-ended resorption based on the site of origin, and can affect the cementum and/or dentine of the root. Since calcium hydroxide has alkaline pH, it actively influences the local environment around a resorptive area by reducing osteoclast activity and stimulating repair. The alkaline calcium hydroxide neutralizes the acidic environment which exists in the region of resorption, reversing the reaction and thus stimulating hard tissue formation. The diffusion of hydroxyl ions released by calcium hydroxide through the dentinal tubules that directly communicate with periodontal space would increase the pH of periodontal space from 6.0 to 7.4 - 9.6 [21] . To treat an internal resorption, the canal and resorption lacuna are filled with calcium hydroxide paste. In this way calcium hydroxide will induce the necrotization process of the remaining tissue in the lacuna, and then by irrigation with sodium hypochlorite the necrotic residuals are removed [4] . In case of lateral resorption, pulp extirpation, debridement of root canal and application of calcium hydroxide are the preferred therapy. The resorptive defect should be filled with calcium hydroxide at 3-month intervals until it reveals hard tissue formation, confirmed by both direct examination through the access cavity and radiograph [4] [11] . After establishment of physical barrier, the defect can be compacted with Gutta-percha [3] . Recently, MTA is an alternative for calcium hydroxide in the management of internal root resorption. It has been reported that MTA used successfully in surgical and non-surgical treatment of internal resorption [4] .
5. Cytotoxicity and Biocompatibility of Calcium Hydroxide
The primary function of the pulp is dentin formation which started when the peripheral mesenchymal cells differentiated into odontoblasts and the collagen matrix begins to deposit, in a sequence of deposition/mineralization that will lead to complete tooth formation. Dentin is produced by the pulp continuously due to the tooth aging, even after the initial formation. Physical and/or chemical injuries may also produce reparative dentin [22] . Dentin-pulp complex can be protected by applying one or more layers of some specific materials between the restorative material and dental tissues. Protection of the dentin-pulp complex leads also to pulp vitality recovery. Calcium hydroxide based products are the materials that can be used for this purpose [23] . Cytotoxicity and biocompatibility of these materials have been widely studied in different cell cultures [22] .
5.1. Effect of Calcium Hydroxide on Pulp Vitality
Pulp tissue is affected by environmental impacts such as heat, mechanical trauma as well as microbial toxins. After multiple injuries, the pulp cells have the capacity to repair and differentiate into odontoblasts and produce dentin matrix proteins during wound healing process. Therefore, not all the inflammatory reaction leads to permanent damage [22] . Due to its direct and indirect effect in pulp repair, calcium hydroxide considers as the most important dental material which is used as the gold standard in biocompatibility tests. Since calcium hydroxide is biologically and therapeutically potential, it is the material of choice for all pulp conservation treatment [23] . Many studies reported that pulp repair and formation of hard tissue barrier can be induced when the pulp tissue directly capped with the different form of calcium hydroxide (Figure 1 and Figure 2) [22] . Clinically, the formation of hard tissue barrier after pulp capping is precious as it provides natural protection from bacterial ingress and chemical products [22] . The mechanism of using calcium hydroxide as pulp capping agent is unclear. However, it has been reported that some proteins and growth factors are released from dentine because of the dissolved high alkaline pH of calcium hydroxide solution. These mechanisms may stimulate pulp repair and formation of hard tissue barrier. Additionally, a layer of coagulation necrosis is induced when the high pH of calcium hydroxide in direct contact with pulp tissue [22] .
![]()
Figure 1. Pulp exposure capped with calcium hydroxide, (arrow). Observe that 30 days after the pulp, therapy, a partial hard tissue barrier was formed, adjacent to the capping agent. HE, ×32 [22] .
![]()
Figure 2. Sixty days after applying calcium hydroxide, on the pulp tissue, a complete hard tissue barrier, (HB) is formed. HE. ×125 [22] .
5.2. Effect of Calcium Hydroxide on Periapical Area
When using calcium hydroxide past in root canal treatment as intracanal medicament, it might be accidentally extruded through the root apex. In case of large chronic periapical lesions, intentional pressing of calcium hydroxide beyond the root canal and into the periradicular tissue has been supported by some researchers. They claimed that calcium hydroxide enhances the healing and osseous repair by direct effect on inflamed tissues. However, this hypothesis was rejected by other researchers and not widely used as extrusion of calcium hydroxide beyond the apex can lead to damaging effects [24] .
In Endodontics, barium sulfate (BaSO4) is added to calcium hydroxide paste as a radiopaque agent. Extrusion of calcium hydroxide paste containing barium sulfate beyond root canal can obscure the apex, and is not easily resorbed over time (Figure 3 and Figure 4) [21] , also barium sulfate enhances the release of inflammatory mediators responding to polymethylmethacrylate (PMMA) particles. Therefore, the healing process might be delayed when using calcium hydroxide paste including barium sulfate, or in this condition the radiographic interpretation of osseous healing might be difficult. Furthermore, the effect of extruded calcium hydroxide paste including a barium sulfate and/or another radiopaque agent and the healing of periapical lesions is not completely clear. Consequently, pure calcium hydroxide is preferred by most clinicians as they believe that the commercial ingredients may delay the healing process they want [24] [25] .
![]()
Figure 3. Radiograph after placement of an intracanal, calcium hydroxide paste dressing with, unintentional periapical overextension [24] [25] .
![]()
Figure 4. The 36-month control radiograph showing healing of, the apical lesion and the presence of a white radiopaque, spot at the place where calcium hydroxide remnants, were originally present [24] [25] .
6. Removal of Calcium Hydroxide from the Canals
Calcium hydroxide is the most commonly used intracanal medicament [26] . However, incomplete removal of the material from the canal may adversely affect sealer performance and subsequent long-term prognosis [27] [28] . Thorough cleaning of root canal system can be achieved by delivering effective irrigation, solution activation as well as direct contact with all canal walls especially in the apical third. Several methods have been described to remove calcium hydroxide from the canal. The most commonly used method is using a master apical file to the working length in conjunction with EDTA and sodium hypochlorite [29] . Using rotary files, sonic and ultra-sonic activated tips with irrigation have also been recommended. However, all of the mentioned methods are not able to remove calcium hydroxide from the canals especially in the apical third [30] [31] [32] . It has been reported that continuous irrigations with vibrating motion may have positive effects on cleaning process, particularly in the apical third of the canal which is the most difficult part to clean [33] .
7. Conclusion
Calcium hydroxide has been used for different purpose in endodontics and available in different forms. Despite its wide range of antimicrobial activity, calcium hydroxide is less effective against some species. Its cytotoxicity appears to be milder than other groups of sealers. The biocompatibility of calcium hydroxide based sealers is controversial and because of their solubility, they do not fulfill all the criteria of an ideal sealer. It is difficult to remove calcium hydroxide completely from the root canals. Further studies are recommended to evaluate the effectiveness of calcium hydroxide and its applications in the field of endodontics.
Appendix
![]()
![]()
![]()
Table A1. Details of the searched articles (narrative review).