Spatial Competition between Health Care Providers: Effects of Standardization ()
1. Introduction
The perspective of industrial economics has been rarely applied to the health care sector (see, for example, Dranove and Satterthwaite [1] ; Gaynor and Vogt [2] ). Many publications focus on empirical analysis; only very few try to elaborate explicit microeconomic model (cf. Gal-Or [3] ). Regarding theoretical approaches, many authors employ the idea to discuss horizontal competition (cf. Dranove and Satterthwaite [1] ; Gaynor and Haas-Wilson [4] ; Pauly [5] ). Limited attention has been paid to standardization effects and horizontal competition within a regional health care market. Nevertheless, in many health care systems there is a tendency to enforce standardization in inpatient as well as outpatient care. As this has direct impacts on the competition environment within a regional health care market, these effects are modeled in this paper. We want to outline competition between two health care providers which face regulated prices and can only differentiate by means of quality competition. Moreover, as cost payers require quality improvements in health care supply, all health care providers have to optimize their way of organizing health. One strategy for them is to standardize production procedures, especially regarding surgery but the magnitude of the relationship seems not really clear (cf. Weitz et al. [6] ). Hence, our paper captures the idea of quality differences by focusing on quality competition in regional health care environments (cf. Brekke, Nuscheler and Straume [7] ). In consequence, we develop an expanded Hotelling model in two steps: we analyze quality choice using an expanded Hotelling framework. There are several methods for analyzing markets for differentiated products. Following Shy [8] , we can find non-address approaches as well as models that employ location ideas (pp. 143 ff.). We employ a Hotelling framework for describing the regional health care market, because hospital competition combines product heterogeneity and different patient preferences. We allow the providers to choose their location, their scope of treatments and the quality of treatments being offered. The hospital supply faces a line of consumers who have different preferences for one health care provider. But there are also some patients at the fringe that could be attracted by the means of quality competition. In the following we use the term horizontal quality when we focus on the choice of location and scope of treatments.1 This is the first stage of our model. On the second stage, the hospital chooses vertical quality. Vertical quality describes the way how one given treatment is produced. This means vertical quality depends for instance on minimum further education standards for physicians or minimum levels for medical devices and pharmaceuticals etc. By means of backward induction, vertical quality can be explained endogenously by the level of horizontal quality that the health care provider chooses first. We introduce standardization, e.g., a standard of vertical quality for treatments in the regional health care market. The standard could be the result of a benchmark process initiated by the regulator or a cost payer (insurance company). This means, we assume that a third party is able to observe the vertical qualities and to prescribe the higher quality as a standard. The regulator sets a level of vertical quality for both health care providers, which is binding for both. For analytical reasons we assume that level of vertical quality set by the regulator corresponds to the first-best level set by provider 1. In this case provider optimizes his profit function. Hence, health care provider 1 can better cope with the standard whereas health care provider 2 has to converge to quality level of his competitor. In consequence, we can show the interaction between the two possibilities of quality setting contingent on a quality leadership in the market. On one hand there are areas for substitution; on the other hand, comparing the own-cost and the cross-cost effects, the standard follower has to consider limitations on the substitution incentive. The paper is organized as follows: Section 2 describes the typical characteristics of a regional health care market. Section 3 introduces the basic model of spatial competition. The model is expanded in Section 3.2 to include a standardization process in the regional health care market. Section 4 summarizes our findings and outlines their implications for further research.
2. Quality Competition in Spatial Health Care Markets
For the discussion it is necessary to define the conditions and restrictions outpatient (physicians) and inpatient (hospitals) health care providers face within the typical health care markets. In a typical patient-physician-situa- tion, patient’s primary demand is directed to a physician who diagnoses the patient and makes the first treatment decisions. For more severe illnesses the patient will be transferred to a higher equipped health care provider for appropriate care. This can be an outpatient specialist or a hospital. For the sake of simplicity we assume that the patient is free to choose between health care providers, i.e., we do not differentiate between inpatient and outpatient care. But patients are typically heterogeneous when considering the scope and the location of health care supply. Hence, a regional health care market simultaneously encompasses heterogeneity in demand as well as in supply. Moreover, in contrast to other markets, prices in health care markets are regularly set by a regulator or the third payer (insurance).2 This strengthens the relevance of competition in quality. In the tradition of industrial economics, we distinguish between vertical quality and horizontal quality. Patients’ preferences for vertical quality are uniformly ranked, i.e., all patients prefer a higher vertical quality when all prices are fixed. Consequently, all patients are better off when the level of medical quality which health care provider 1 offers rises.3 Horizontal quality refers to characteristics where the optimal choice depends on the characteristics of the consumer. Health care provider location or the range of treatments offered can be represented through the horizontal quality variable. Patients who are closer to health care provider 1 have less opportunity costs when choosing provider 1 than those located closer to provider 2. In contrast to a rise in vertical quality a rise in horizontal quality does not necessarily constitute a Pareto improvement. Consumers, whose optimal horizontal quality was close to the offered horizontal quality before the change, may face a decline in utility as the deviation between their desired quality and the quality offered increases (cf. Shy [8] ). For the purpose of this paper we regard that the chosen horizontal quality is necessarily fixed for the time being. Therefore, the only remaining choice concerns vertical quality.
3. Model of Quality Competition
3.1. Basic Model
A simple model of a regional health care market can be derived from the papers of Glazer and McGuire [9] , Montefiori [10] or Brekke et al. [11] . Considering the results of Gravelle [12] and Calem and Rizzo [13] we use the approach of the spatial competition literature to model the effects of standardization. This should provide a good intuition for the probable consequences of the implementation of a new form of standardized care. Brekke, Nuscheler and Straume [7] develop a specific model that combines ideas of spatial competition in the tradition of Hotelling [14] with quality competition. This is our point of reference in this paper.4 Like them we employ a two-stage model of health care provision with fixed prices. In the first stage, each health care provider decides on horizontal quality. He selects his range of treatments offered. 5After the decision on horizontal quality at the first stage the health care providers compete by choosing the quality of care they provide in the second stage, i.e., by choosing a level of vertical quality.
3.1.1. Demand for Health Care
As a first step we model patients’ demand for health care. We follow Hotelling’s idea of a linear city6 and assume rational consumers with perfect and complete information about all relevant parameters. The termai denotes the absolute position of the health care provider I on the [0, 1] interval.7 We assume health care provider 1 is located left within the spectrum and health care provider 2 is located right 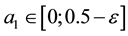 and
and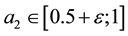 . Hence, we assume there is a perceivable horizontal quality difference so that patient’s location or need for a specific treatment will generally direct them to one of the providers, i.e., the average patient is not indifferent between health care providers but has a decided preference for one. Demand for a (specific) unit of health care hl is assumed to be independently identically distributed on the [0; 1] interval. In the line of a linear model the patients are heterogeneous considering the both health care providers which resembles some baseline preference for proximity of care.8 In addition to horizontal quality we consider vertical quality in the standard of care for any given treatment, which is described by the parameter
. Hence, we assume there is a perceivable horizontal quality difference so that patient’s location or need for a specific treatment will generally direct them to one of the providers, i.e., the average patient is not indifferent between health care providers but has a decided preference for one. Demand for a (specific) unit of health care hl is assumed to be independently identically distributed on the [0; 1] interval. In the line of a linear model the patients are heterogeneous considering the both health care providers which resembles some baseline preference for proximity of care.8 In addition to horizontal quality we consider vertical quality in the standard of care for any given treatment, which is described by the parameter . The variable costs for crossing the distance to a regional provider are borne by the patient. They are assumed to be constant and denoted by t. As we have noted before, within the model
. The variable costs for crossing the distance to a regional provider are borne by the patient. They are assumed to be constant and denoted by t. As we have noted before, within the model , the price for medical treatment, is independent of the scope of medical treatment and the vertical quality offered. Now, we additionally assume
, the price for medical treatment, is independent of the scope of medical treatment and the vertical quality offered. Now, we additionally assume  is regulated and fix for all health care providers.9 Similar to Brekke, Nuscheler and Straume [7] each patient faces the following objective:
is regulated and fix for all health care providers.9 Similar to Brekke, Nuscheler and Straume [7] each patient faces the following objective:
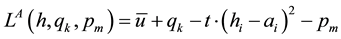 (3.1)
(3.1)
The patient of interest is the indifferent one located at the margin between the both health care providers. He has to decide whether health care provider 1 or health care provider 2 are entitled to treat him.10 We assume, that net utility is always positive, even for the lowest vertical quality possible. The whole market is always covered for the regulated price  which is equal for all patients. Each consumer demands one unit of the good and a second unit does not offer additional utility. The indifferent patient can be described with the following location
which is equal for all patients. Each consumer demands one unit of the good and a second unit does not offer additional utility. The indifferent patient can be described with the following location  which is the solution to:
which is the solution to:
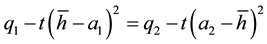 (3.2)
(3.2)
The result allows us to denote the position h in the linear city. Both health care providers face the same indifferent patient. Consequently, health care provider’s demand  is the fraction of the market just up to the marginal consumer
is the fraction of the market just up to the marginal consumer .
.
 (3.3)
(3.3)
For the other health care provider  holds. For the non-spatial case there is an intuitive interpretation of this variable. If
holds. For the non-spatial case there is an intuitive interpretation of this variable. If  is high, a substantial part of patients choose health care providers offering a wide range of treatments. If
is high, a substantial part of patients choose health care providers offering a wide range of treatments. If  is low, the majority prefers treatment by providers with a lower degree of horizontal quality
is low, the majority prefers treatment by providers with a lower degree of horizontal quality , i.e., by providers who specialize in a small number of treatments. We split expression (3.3) into three parts:11
, i.e., by providers who specialize in a small number of treatments. We split expression (3.3) into three parts:11
![]() (3.4)
(3.4)
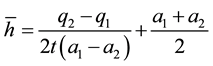
The position of![]() , the marginal consumer, depends on vertical quality difference, the degree of competition and average horizontal quality. We are particularly interested in the degree of competition. From the second term over braces we infer that the degree of competition rises when t is low and/or the gap between
, the marginal consumer, depends on vertical quality difference, the degree of competition and average horizontal quality. We are particularly interested in the degree of competition. From the second term over braces we infer that the degree of competition rises when t is low and/or the gap between ![]() and
and ![]() is small, i.e. there is little differentiation in horizontal quality.
is small, i.e. there is little differentiation in horizontal quality.
3.1.2. Supply of Health Care
Taking health care provider 1 as our representative producer in a world with two health care providers, we get the following profit function:
![]() (3.5)
(3.5)
![]()
10The model is limited to selective medical treatments a patient can anticipate and plan.
11Cf. Pfähler and Wiese [17] : 244.
12The case where this condition is not met presents us with an argument against insufficiently high reimbursements, as these could lead to low levels of quality and a sub-optimally narrow range of treatments. Interested readers are referred to Newhouse [18] and Pope [19] .
13![]() . See Brekke, Nuscheler and Straume [7] : 212.
. See Brekke, Nuscheler and Straume [7] : 212.
We set ![]() for the regulated price all health care suppliers face. We suppose that reimbursements cover costs, i.e. that
for the regulated price all health care suppliers face. We suppose that reimbursements cover costs, i.e. that ![]() is valid. If reimbursements do not cover costs there will be no voluntary supply, consequently, this case is irrelevant in a market economy.12
is valid. If reimbursements do not cover costs there will be no voluntary supply, consequently, this case is irrelevant in a market economy.12
The parameter ![]() signifies the variable cost of a treatment while
signifies the variable cost of a treatment while ![]() denotes fixed cost. The variable costs occur if the minimum level of quality
denotes fixed cost. The variable costs occur if the minimum level of quality ![]() is provided. The costs
is provided. The costs ![]() for producing higher vertical quality
for producing higher vertical quality ![]() are supposed to be convex.13 Costs for a given level of vertical quality are therefore a combination of the variable costs for the provision of basic quality and a higher vertical quality cost increment.
are supposed to be convex.13 Costs for a given level of vertical quality are therefore a combination of the variable costs for the provision of basic quality and a higher vertical quality cost increment.
There are already a few very straightforward results to be derived from this profit function. Profit can only be positive, if reimbursements exceed variable costs ![]() and rises with the difference between these two variables. Variable cost for vertical quality
and rises with the difference between these two variables. Variable cost for vertical quality ![]() and fixed costs
and fixed costs ![]() have a negative impact on profits. These results are general and do not depend on the specifications of the model. Substituting the results derived in (3.3) into the profit function we get:
have a negative impact on profits. These results are general and do not depend on the specifications of the model. Substituting the results derived in (3.3) into the profit function we get:
![]() (3.6)
(3.6)
Now we analyze the effects of decisions on vertical and horizontal quality. We know, that provider 1 has a smaller ![]() than provider 2, therefore the first term within the brackets can only be positive if
than provider 2, therefore the first term within the brackets can only be positive if![]() . Provider 1, the provider with the smaller range of treatments offered in the non-spatial interpretation, has an incentive to offer higher vertical quality, because this increases his profits. If he offers a lower vertical quality the difference in horizontal quality between providers will lower his profits compared to the case in which both providers offer homogenous goods. For this vertical quality distribution, profits for a provider with the higher vertical quality rise, the smaller the difference in horizontal quality
. Provider 1, the provider with the smaller range of treatments offered in the non-spatial interpretation, has an incentive to offer higher vertical quality, because this increases his profits. If he offers a lower vertical quality the difference in horizontal quality between providers will lower his profits compared to the case in which both providers offer homogenous goods. For this vertical quality distribution, profits for a provider with the higher vertical quality rise, the smaller the difference in horizontal quality ![]() and the smaller transport costs t are. Consequently, there is an incentive to diversify horizontally for this provider.
and the smaller transport costs t are. Consequently, there is an incentive to diversify horizontally for this provider.
3.1.3. Optimal Vertical Quality
In our basic model we assume that both health care providers offer different levels of vertical quality. The first order condition for the profit-maximizing quality ![]() is:
is:
![]() (3.7)
(3.7)
![]()
14The second-order condition is negative![]() .
.
15For the discussion of health care provider 2 cf. Appendix A.1.
As we have assumed that ![]() the above equation only holds if
the above equation only holds if![]() . Otherwise the first order condition for a profit-maximum would not be satisfied, as
. Otherwise the first order condition for a profit-maximum would not be satisfied, as![]() . Profit-maximizing vertical quality14 can be written as:
. Profit-maximizing vertical quality14 can be written as:
![]() (3.8)
(3.8)
Comparative static for optimal quality yield for![]() :15
:15
![]() (3.9)
(3.9)
This equation tells us, that a higher level of horizontal quality (![]() rises) induces the level of competition. Hence, the health care provider is compelled to increase the vertical quality
rises) induces the level of competition. Hence, the health care provider is compelled to increase the vertical quality![]() . The implication of this relationship can be explained looking at the differences in heterogeneity of medical supply.
. The implication of this relationship can be explained looking at the differences in heterogeneity of medical supply.
Comparing this result with the impact of ![]() gives:
gives:
![]() (3.10)
(3.10)
An increase in the (horizontal quality) distance between the two health care providers decreases provider 1’s incentive to offer a high level of vertical quality.
![]() (3.11)
(3.11)
The incentive to provide quality is negatively related to t, the parameter denoting transport cost or the cost of quality mismatch for patients. This is plausible, as competition from other health care providers is lower when opportunity costs (the product of the actual distance/quality mismatch and the cost parameter) are high. The health care provider can anticipate that the patient will compare higher transport costs with a potential loss of vertical quality.
![]() (3.12)
(3.12)
As ![]() is true per definition, the impact of an increase in
is true per definition, the impact of an increase in ![]() is to lower the level of vertical quality. Costs directly reduce profit and consequently reduce the incentive to compete via higher quality.
is to lower the level of vertical quality. Costs directly reduce profit and consequently reduce the incentive to compete via higher quality.
![]() (3.13)
(3.13)
The above equation shows that the negative relationship between costs and quality is not only true for the cost of treatment, but also for the costs of quality improvements![]() . Again, a reduction of profits lowers the incentive to compete for them via higher vertical quality.
. Again, a reduction of profits lowers the incentive to compete for them via higher vertical quality.
Result 1
The conclusions for both health care providers are (compare A.1):
・ It exists a partial substitution between horizontal and vertical quality. If one health care provider sets its medical supply more homogeneously in comparison to the other health care provider, he has to increase vertical quality in order to cope with the higher level of competition (3.9).
・ If health care provider 2 changes horizontal quality, e.g., both providers gets more heterogeneous, health care provider 1 has less incentive to increase vertical quality (3.10).
・ Higher opportunity costs reduce the patients’ gain from higher vertical quality. In consequence the provider has to differentiate and expand its vertical quality supply (3.11).
・ Higher costs for producing health care ![]() reduces the possibility for provider 1 to increase his vertical quality (3.12).
reduces the possibility for provider 1 to increase his vertical quality (3.12).
・ Higher costs of vertical quality ![]() will directly reduce the interest of provider 1 to increase the vertical quality (3.13).
will directly reduce the interest of provider 1 to increase the vertical quality (3.13).
3.1.4. Optimal Horizontal Quality
When determining optimal horizontal quality ![]() for each health care provider, we have to keep in mind that
for each health care provider, we have to keep in mind that ![]() is true per definition. In other words, for provider 1 an increase in
is true per definition. In other words, for provider 1 an increase in ![]() would reduce differentiation between providers, whereas an increase in
would reduce differentiation between providers, whereas an increase in ![]() would c.p. induce a greater distance. Backwards induction stipulates both health care providers to choose an optimal level of
would c.p. induce a greater distance. Backwards induction stipulates both health care providers to choose an optimal level of ![]() when determining optimal horizontal quality
when determining optimal horizontal quality![]() . Inserting
. Inserting ![]() into Equation (3.6) gives us the new profit function:
into Equation (3.6) gives us the new profit function:
![]() (3.14)
(3.14)
The implicit optimal value of ![]() considering the first order condition is:
considering the first order condition is:
![]() (3.15)
(3.15)
The optimal value of ![]() and
and ![]() cannot be computed directly. Hence, for both health care provider sexist a kind of reaction function for the optimal values
cannot be computed directly. Hence, for both health care provider sexist a kind of reaction function for the optimal values![]() :16
:16
![]() (3.16)
(3.16)
Considering health care provider 1 we observe that the second derivative of (3.14) over ![]() is also negative which means that there is a local profit optimum at the left side of the range
is also negative which means that there is a local profit optimum at the left side of the range![]() .17
.17
In consequence both reaction functions resemble “strategic complements”. Hence, it is possible that there is a corner solution possible for both health care providers. Using the Equation (A.10) we can differentiate between two relevant cases considering the assumption about the relation between ![]() and
and![]() . Looking at the marginal
. Looking at the marginal
differentiation of both profit functions we have to discuss ![]() and
and![]() .18
.18
・ The sign of ![]() will be negative as long as
will be negative as long as ![]() holds. Hence, for provider 1
holds. Hence, for provider 1 ![]() follows.
follows.
・ But for the reverse cost relation it is also possible that provider 1 would choose![]() .
.
・ Considering ![]() for provider 2, using equation A-13 it is possible that
for provider 2, using equation A-13 it is possible that ![]() is valid.
is valid.
・ In consequence, assuming ![]() it may be possible that for both providers a kind of a “Nash-equilibrium”
it may be possible that for both providers a kind of a “Nash-equilibrium”
exists that induces ![]() and
and![]() .
.
For the sake of simplification we set ![]() henceforward and we only discuss the partly marginal effects for the reaction function of health care provider 1.
henceforward and we only discuss the partly marginal effects for the reaction function of health care provider 1.
As we cannot directly infer the marginal effects for the first stage, we use the optimal level of ![]() and the marginal effects (stage two).19 Following the first-order condition for vertical quality, we compare the results for both health care providers at the second stage:
and the marginal effects (stage two).19 Following the first-order condition for vertical quality, we compare the results for both health care providers at the second stage:
![]() for health care provider 1 (3.17)
for health care provider 1 (3.17)
![]() for health care provider 2
for health care provider 2
For ![]() and assuming
and assuming ![]() holds the following must be true:
holds the following must be true:
![]() (3.18)
(3.18)
・ If ![]()
・ and ![]()
Under the described circumstances competition will always result in a higher vertical quality for the health care provider 1 with the lower![]() . This sheds light on the conditions that could be relevant for different qualities
. This sheds light on the conditions that could be relevant for different qualities ![]() if horizontal quality is set. Therefore, the decision for the horizontal quality at stage one is taken in view of the capabilities for producing vertical quality.
if horizontal quality is set. Therefore, the decision for the horizontal quality at stage one is taken in view of the capabilities for producing vertical quality.
The influence of the variable costs ![]() can be described as follows:
can be described as follows:
![]() (3.19)
(3.19)
The sign of the fraction is not directly clear. Hence, we use the following assumption to get an idea of the re-
lationship between horizontal and vertical quality. The denominator will be positive ![]()
・ If: ![]()
・ or: ![]()
In this case a high level of a reimbursement ![]() makes the second, fourth and sixth term of the numerator
makes the second, fourth and sixth term of the numerator
negative. Nevertheless, the whole numerator is positive as long as![]() . In consequence
. In consequence ![]() could
could
be assumed.
For a change in quality costs ϕ1 the following holds:
![]() (3.20)
(3.20)
The sign of the denominator is still assumed to be positive, as we have outlined above. Hence, following the
basic assumption ![]() the whole fraction gets negative and
the whole fraction gets negative and ![]() holds.
holds.
When we look at the parameter t we get:
![]() (3.21)
(3.21)
For the denominator the impact of the assumption concerning quality cost will be helpful, too. The numerator
will be negative for the range ![]() Hence, the result could be
Hence, the result could be![]() . The more
. The more ![]() converges to
converges to
![]() the more probable the expected result
the more probable the expected result ![]() gets.
gets.
Result 2
We could summarize our findings:
・ An increase of the costs ![]() will induce health care provider 1 to reduce his horizontal quality. Additionally, both health care providers will be incited to reduce their vertical quality (3.19).
will induce health care provider 1 to reduce his horizontal quality. Additionally, both health care providers will be incited to reduce their vertical quality (3.19).
・ Higher costs ![]() will incite health care provider 1 to expand his horizontal quality. Only when health care provider 1 has a large cost advantage in
will incite health care provider 1 to expand his horizontal quality. Only when health care provider 1 has a large cost advantage in ![]() he would accept to converge to the other health care provider. Referring to the optimal value of
he would accept to converge to the other health care provider. Referring to the optimal value of ![]() higher costs
higher costs ![]() will directly reduce the health care providers’ incentive to increase vertical quality (3.20).
will directly reduce the health care providers’ incentive to increase vertical quality (3.20).
・ An increase in opportunity costs t will incite health care provider 1 to reduce his horizontal quality, i.e., to decrease the differentiation. Only if health care provider 1 has an advantage ![]() it could be optimal to expand horizontal quality a1 and reduce differentiation (3.21).
it could be optimal to expand horizontal quality a1 and reduce differentiation (3.21).
3.2. Standardization and the Impact on Competition
3.2.1. Preliminaries
![]()
20We do not analyze the welfare maximizing level of![]() .
.
21This result may directly be followed by the assumption![]() .
.
Up to now we have discussed the case where both health care providers could differentiate between horizontal and vertical quality. Now we introduce the idea of a standard for vertical quality. We assume that both health care providers are not able to anticipate this step by the regulator. They are not able to form expectations about the timing, process or nature of the actual regulation and are therefore not able to choose their competition parameters strategically. This is not entirely implausible as things can change quickly in health care systems. For the purpose of this model we assume that the regulator chooses the highest observable level of vertical quality as standard. In the following we continue to set that ![]() holds and therefore assuming all other things equal health care provider 1 has an advantage in vertical quality
holds and therefore assuming all other things equal health care provider 1 has an advantage in vertical quality![]() .20
.20
Now, our assumption is that the regulator may set a vertical quality ![]() that would perfectly match the optimal quality
that would perfectly match the optimal quality![]() .21 However, for the health care provider this choice is at random. As the United Kingdom, Germany and Switzerland require their independent health care providers to document their quality levels, the assumption of an informed regulator is plausible. As a consequence, both health care providers have to accept this standardized level of vertical quality but health care provider 1 could cope better than health care provider 2.
.21 However, for the health care provider this choice is at random. As the United Kingdom, Germany and Switzerland require their independent health care providers to document their quality levels, the assumption of an informed regulator is plausible. As a consequence, both health care providers have to accept this standardized level of vertical quality but health care provider 1 could cope better than health care provider 2.
Following the regulation rule, health care provider 2 has to accept the level ![]() and provide a sub- optimal level of quality from his point of view. The position of the indifferent patient changes to hStandard:
and provide a sub- optimal level of quality from his point of view. The position of the indifferent patient changes to hStandard:
![]() (3.22)
(3.22)
Both health care providers choose the levels of ![]() and
and ![]() within the model. Moreover, as the vertical quality is not a relevant parameter for competition anymore, health care provider 1 would benefit from the given standard. Hence, he will be the standard profiteer because his horizontal quality fits the standard vertical quality. The new profit function for health care provider 1 can be written as:
within the model. Moreover, as the vertical quality is not a relevant parameter for competition anymore, health care provider 1 would benefit from the given standard. Hence, he will be the standard profiteer because his horizontal quality fits the standard vertical quality. The new profit function for health care provider 1 can be written as:
![]() (3.23)
(3.23)
Considering the first order condition the following holds:
![]() (3.24)
(3.24)
As we assume that the standard follows ![]() the health care provider 1 will optimize
the health care provider 1 will optimize ![]() contingent on his expectations about the optimal level
contingent on his expectations about the optimal level![]() .
.
3.2.2. Impact of Regulation on Health Care Provider 1
After the description of the standard we want to elaborate the impact of standardization upon competition in horizontal quality. For the optimal horizontal quality of the standard profiteer ![]() we apply the total differentiation of the first order condition and insert the marginal effects from the second stage. With other words, we assume the optimal level of vertical quality for the standard profiteer and then look at standardization. As there is no possibility to substitute a difference in horizontal quality with vertical quality, we have to discuss the optimal in a one stage model. Hence, both health care providers have only to consider the distance between each other as a level of competition. As we cannot derive a mutual best answer for each health care provider we concentrate on discussing the marginal effects for both health care providers: For the impact of
we apply the total differentiation of the first order condition and insert the marginal effects from the second stage. With other words, we assume the optimal level of vertical quality for the standard profiteer and then look at standardization. As there is no possibility to substitute a difference in horizontal quality with vertical quality, we have to discuss the optimal in a one stage model. Hence, both health care providers have only to consider the distance between each other as a level of competition. As we cannot derive a mutual best answer for each health care provider we concentrate on discussing the marginal effects for both health care providers: For the impact of ![]() on
on ![]() the following holds:
the following holds:
![]() (3.25)
(3.25)
and
![]() (3.26)
(3.26)
Considering Equation (3.25) the own-cost effect may be ambiguous. As the denominator is always positive the overall sign depends on the numerator. The second term will be positive as long as the second addend in the brackets exceeds the first addend, i.e., for high levels of![]() . With low levels of
. With low levels of ![]() the second term of (3.25) is negative and therefore the standard profiteer has a direct incentive to increase horizontal quality. Consequently, a relatively small remuneration reduces the standard profiteer’s incentive to attract more patients through an increase in horizontal quality. From (3.26) we can directly conclude that there is no relevant impact on the costs of the competitor. Considering the parameter
the second term of (3.25) is negative and therefore the standard profiteer has a direct incentive to increase horizontal quality. Consequently, a relatively small remuneration reduces the standard profiteer’s incentive to attract more patients through an increase in horizontal quality. From (3.26) we can directly conclude that there is no relevant impact on the costs of the competitor. Considering the parameter ![]() we get:
we get:
![]() (3.27)
(3.27)
and
![]() (3.28)
(3.28)
![]()
22The following only holds as long as![]() .
.
The expression will always be positive if the basic assumption ![]() is still valid. Higher costs for the provision of vertical quality increases the incentive to diminish horizontal differentiation.22 For the parameter t we get:
is still valid. Higher costs for the provision of vertical quality increases the incentive to diminish horizontal differentiation.22 For the parameter t we get:
![]() (3.29)
(3.29)
The expression will be always positive, if the basic assumptions are still valid. Higher travelling or quality mismatch costs reduce the standard profiteer’s incentive to differentiate horizontally.
Result 3
As the health care provider could directly benefit from the vertical standard his decision on horizontal quality could be characterized as follows:
・ Higher costs of c1 will incentivize the standard profiteer to increase horizontal quality differentiation (a1↓). But this effect could be outweighed by higher reimbursement ![]() (3.25). The standard profiteer has not to consider the costs of the other health care provider (3.26).
(3.25). The standard profiteer has not to consider the costs of the other health care provider (3.26).
・ If the costs for the standardized vertical quality rise the standard profiteer will reduce the difference in horizontal quality and increase the degree of competition (3.27). The standard profiteer has only to bear the own-cost effects (3.28).
・ If patients have to bear higher opportunity costs for selecting one health care provider the standard profiteer will also reduce the difference in horizontal quality and increases the degree of competition (3.29).
3.2.3. Impact of Regulation on Health Care Provider 2
The next equations show the impact of vertical quality regulation on health care provider 2’s decision for horizontal quality. He has to cope with the vertical standard ![]() and therefore we want to elaborate
and therefore we want to elaborate![]() . Although both providers must accept the standard health care provider 2 is like a “follower” in typical oligopolistic models. Due to regulated vertical quality, competition can only take place through a choice of locations or differences in the scope of treatments. For the standard follower there is c.p. a high incentive to hold the distance in horizontal quality. For the standard profiteer the opposite seems to be true. We can discuss these effects by using the marginal effects for the standard follower: For the production costs
. Although both providers must accept the standard health care provider 2 is like a “follower” in typical oligopolistic models. Due to regulated vertical quality, competition can only take place through a choice of locations or differences in the scope of treatments. For the standard follower there is c.p. a high incentive to hold the distance in horizontal quality. For the standard profiteer the opposite seems to be true. We can discuss these effects by using the marginal effects for the standard follower: For the production costs ![]() we get:
we get:
![]() (3.30)
(3.30)
The sign is definitely negative as long as the basic assumption ![]() holds. The impact of
holds. The impact of ![]() on
on ![]() is unambiguous. As we assumed, the standard follower has to bear higher vertical quality costs
is unambiguous. As we assumed, the standard follower has to bear higher vertical quality costs![]() . If there is a rise in the cost for basic health services
. If there is a rise in the cost for basic health services![]() , the follower has an incentive to reduce the distance to the standard follower.
, the follower has an incentive to reduce the distance to the standard follower.
The standard follower has also to anticipate the cross-cost-effects:
![]() (3.31)
(3.31)
As denominator and numerator are negative by assumption the overall effect is always negative. The standard follower has also to reduce the horizontal quality given the provider’s 1 costs for producing health increase. For a change in ![]() the following is valid:
the following is valid:
![]() (3.32)
(3.32)
The sign of the numerator is positive due to the basic assumption![]() . Higher costs for producing vertical quality additionally diminish health care provider 2’s profits, and therefore his incentive to attract patients. Instead of increasing the level of competition, he chooses a greater horizontal differentiation from the standard profiteer to reach the point where his marginal quality costs equal marginal returns. But he also has to consider the cross-cost effect:
. Higher costs for producing vertical quality additionally diminish health care provider 2’s profits, and therefore his incentive to attract patients. Instead of increasing the level of competition, he chooses a greater horizontal differentiation from the standard profiteer to reach the point where his marginal quality costs equal marginal returns. But he also has to consider the cross-cost effect:
![]() (3.33)
(3.33)
In consequence of our basic assumption the effect will be always negative. Hence, the standard follower is compelled to reduce horizontal differentiation if the exogeneous standard costs which fit better for health care provider 1 increase. When we look at t we get:
![]() (3.34)
(3.34)
The impact seems to be clear. The numerator is definitely negative, whereas the denominator is always positive. A higher cost parameter t also encourages the standard follower to reduce his horizontal quality.
Result 4
The standard follower reduces most of his parameters for competing in spatial competition:
・ The own-cost effect is always positive. The standard follower will try to reduce the degree of competition because of its worse cost situation in comparison to the standard profiteer (3.30). But he has also to anticipate the cross-cost effects, which are opposite to the own-cost effects (3.31).
・ A similar result could be inferred by discussing the costs for the standardized vertical quality![]() . As the own-cost effect is positive which would incite the standard follower to reduce the degree of competition (3.32) the cross-cost effect is negative (3.33).
. As the own-cost effect is positive which would incite the standard follower to reduce the degree of competition (3.32) the cross-cost effect is negative (3.33).
・ For higher opportunity costs the standard follower will react similar to the standard profiteer and reduce the horizontal differentiation (3.34).
4. Conclusions and Outlook
We use an extension of a Hotelling model to analyze the impact of a standardization of vertical quality on horizontal quality in a regional health care market. In the basic model both health care providers compete in horizontal and vertical quality. The basic model tells us that the choice of vertical quality ![]() will be made conditionally on optimal horizontal quality
will be made conditionally on optimal horizontal quality ![]() of the competitor. The success of competing in vertical quality is directly dependent on the comparison of the cost parameters
of the competitor. The success of competing in vertical quality is directly dependent on the comparison of the cost parameters ![]() of both competitors. In the standardization case the standard profiteer gets similar results like in the basic model. But, the standard follower fairly loses control over horizontal quality because he has to cope with the suboptimal vertical standard, which he has to anticipate in his decision for horizontal quality. This leads to a non-optimal level of vertical quality as well as horizontal quality for the standard follower. Considering the impact of own-cost effect and cross-cost effect, some direct implications for regional competition exist:
of both competitors. In the standardization case the standard profiteer gets similar results like in the basic model. But, the standard follower fairly loses control over horizontal quality because he has to cope with the suboptimal vertical standard, which he has to anticipate in his decision for horizontal quality. This leads to a non-optimal level of vertical quality as well as horizontal quality for the standard follower. Considering the impact of own-cost effect and cross-cost effect, some direct implications for regional competition exist:
・ The follower is driven out of the market, because he is not able to offer the standard quality as the costs of doing so are prohibitively high for him;
・ or he has to accept the chosen quality which is (more) beneficial for the standard profiteer and has to accept lower profits in comparison to the non-standard case.
As we can directly infer from the comparison of basic model and standardization model, there is substitution between horizontal and vertical quality, which may be beneficial for health care providers as well as for patients if the standard leader can outweigh vertical quality with horizontal quality. More investigation in this area is necessary especially when discussing the impacts on welfare. We focus on a restricted area of horizontal quality where both health care providers are free to choose. For further research it would be interesting to widen our approach by incorporating a more detailed discussion on the scope and level of standardization. Moreover, it could be beneficial to widen the analysis to another form of standardization where both health providers could anticipate and probably influence the standard setting.
Appendix
A.1. Vertical Quality
The second health care provider has to optimize the following profit function:
![]() (A.1)
(A.1)
The first order condition for the profit maximizing quality ![]() is:
is:
![]() (A.2)
(A.2)
The optimal level of ![]() is:
is:
![]() (A.3)
(A.3)
Using comparative statics we get:
![]() (A.4)
(A.4)
![]() (A.5)
(A.5)
![]() (A.6)
(A.6)
![]() (A.7)
(A.7)
![]() (A.8)
(A.8)
![]() (A.9)
(A.9)
A.2. Horizontal Quality
For the optimal horizontal quality we insert the optimal values ![]() and
and ![]() into the profit function (3.14) und compute in an explicit manner. Because we are looking at a corner solution we get:
into the profit function (3.14) und compute in an explicit manner. Because we are looking at a corner solution we get:
![]() (A.10)
(A.10)
The whole expression will be negative if the second addend cannot compensate the negative impact of the
first addend. If there is no difference in vertical quality the expression simplifies to:![]() .
.
Considering the second derivation, we get:
![]() (A.11)
(A.11)
As the first addend will always be negative and the expression within the brackets encompasses positive as well as negative parts we can assume that the whole formula get negative, as long as the assumption for the first derivative holds. The result for the optimal choice of ![]() given
given ![]() can be computed by inserting the optimal values
can be computed by inserting the optimal values ![]() and
and ![]() into the profit function (3.14) (cf. (A.10)):
into the profit function (3.14) (cf. (A.10)):
![]() (A.12)
(A.12)
As we can see from (A.12) the optimal level of ![]() depends on
depends on![]() , the other provider’s horizontal quality. We are looking at a reaction function
, the other provider’s horizontal quality. We are looking at a reaction function![]() . The corresponding reaction function for health care provider 2 is:
. The corresponding reaction function for health care provider 2 is:
![]() (A.13)
(A.13)
NOTES
*Corresponding author.
![]()
1This means we have two possible interpretations for horizontal quality.
2We will therefore treat prices as fixed in this paper. No additional offerings which can be paid for by the patients are assumed. In comparison to Brekke et al. [11] we only concentrate on quality competition without any differentiations in hospital reimbursement.
![]()
3The same argument applies to health care provider 2.
4In contrast to Brekke, Nuscheler and Straume [7] we do not attempt to find an optimal reimbursement scheme or the reimbursement level that will maximize welfare.
5Interested readers are referred to Robinson and Casalino [15] and Gal-Or [3] for an in-depth discussion of this topic.
6The presentation of the basic model follows Tirole [16] : 96 ff.
7ai stands for the chosen location in the spatial interpretation. In the service differentiation case it denotes the range of treatments offered.
8Differences between hl and ai represent a quality mismatch. Opportunity costs are the costs consumers face because the range of treatments covered by a given medical care provider does not exactly match their preferences (cf. Shy [8] and can be computed by multiplying the actual mismatch with a cost parameter t).
9As we assume all patients are insured, they do not face variable costs of treatment. Effects on insurance are either non-existent or not perceptible for patients. It is important to note that this price for treatment is not identical with hospital remuneration which we will denote later.
![]()
16For the explicit solution cf. Appendix (A.10).
17Cf. Appendix (A.2). Although it might be interesting to consider quality choice by a provider, who is not able to choose his location freely in view of existing regulations. The scope of this paper is limited and we have to refrain from discussing that particular topic.
![]()
18Cf. Appendix (A.10).
19In the following we concentrate on health care provider 1. The results for the other health care provider are to be found in Appendix A.3.