2. MATERIALS AND METHODS
This is a single-center open-label prospective clinical study. The clinical study part was carried out at Overton Brooks VA Medical Center at Shreveport, Louisiana after the approval of the protocol and consent form Institutional Review Board at LSUHSC, Shreveport as well as the Research and Development Committee at VAMC. All the subjects have provided informed consent. The samples for this clinical study were collected at Overton Brooks VAMC, Shreveport, LA between 2006 and 2009. Plasma from the venous blood samples drawn for insulin, C-reactive protein (CRP), tumor necrosis factor α (TNF-a), interleukin-6 (IL-6) and adiponectin and urine samples were stored at −80˚C for until further analysis. For the study of aspirin resistance, supplemental analyses of the samples were carried out at Stratton VAMC and Research Pharmacy Institute at Albany. The inclusion criteria included men aged 30 - 55 years of all ethnic groups with Type 2 diabetes and normal kidney function, evaluated by creatinine < 1.4 and eGFR > 70. One hundred and forty two subjects with Type 2 diabetes were included in the study. Clinical parameters include weight, height, waist circumference, duration of diabetes, history of hypertension, and history of premature coronary artery disease. Basic labs collected include fasting lipids, HbA1c, uric acid, serum creatinine and urine micro-albumin in all subjects. Body composition analysis was carried out by DXA.
Laboratory measurements: Levels of total adiponectin, MCP, TNF-a, CRP, IL-6 and insulin were measured in duplicate using commercially available kits (ALPCO diagnostics, USA). The sensitivity of the adiponectin assay is 0.234 ng/mL (range of 0.375 - 12 ng/mL). Interand intra-assay coefficients of variation were 2.8% - 5.5% and 2.97% - 3.84%, respectively. The sensitivity of the CRP assay is 0.124 ng/mL. Interand intra-assay coefficients of variation were 5.5% - 6% and 11% - 13%, respectively. The sensitivity of the TNF-α assay is 4.8 pg/mL. Interand intra-assay coefficients of variation were ±10.8% and 4% - 8.3%, respectively. The sensitivity of the insulin assay is 1 µIU/mL. Interand intra-assay coefficients of variation were 2.6% - 3.6% and 2.8% - 4%, respectively. The insulin resistance index was calculated from fasting glucose and insulin using the formula of homeostatic model assessment (HOMA-R). HOMA-R = (plasma glucose level x plasma insulin level/22.5). Urinary 11-dehydro-thromboxane beta-2 (11DhTx2) concentrations measured using an enzyme immunoassay kit from Cayman chemicals with a specificity of 100% and sensitivity at 120 pg/ml and an intraand inter assay variability of 5% - 7%. Levels of 11DhTx2, a major urinary metabolite of thromboxane at ≥ 1500 pg/mg of creatinine is considered as AR.
Aspirin: Bioassay of aspirin in the serum was carried out by Liquid Chromatography Mass Spectrometry (LC/MS/MS) in MRM mode. LC-MS/MS in MRM mode offers analytical specificity much more superior to that of immunoassay or conventional HPLC for low molecular weight analyses. Aspirin levels are expressed as μg/mL and it is the sum of salicylic acid, which were eluted at different time as various glucoronides possess different retention time.
Statistical analyses: Statistical analyses were carried out using Microsoft Excel 2007. All data are presented as means ± S.D. A p value of <0.05 is considered statistically significant. Difference in the clinical and biochemical parameters between the subjects with elevated 11DhTx2/cre levels and those with normal levels was carried out. Correlation of 11DhTx2 /cre levels with other clinical and biochemical parameters were carried out.
3. RESULTS
Baseline characteristics of the cohort are shown in Table 1. Participants included 142 male patients with Type 2 diabetes. Their average age was 48 years, and most were Caucasian. The levels of insulin, HbAiC, and adipocytokines are shown in Table 2. Approximately 55% of subjects had aspirin resistance (poor response to aspirin) as measured by elevated urinary 11-dehydrothromboxane beta-2 (11DhTx2) concentration. The comparative clinical parameters of the subjects with T2DM with or with aspirin resistance are shown in Table 3.
Compared to the subjects with 11DhTx2/cre levels < 1500, there are no significant differences in the clinical parameters such as age, history of hypertension or BMI, waist to hip ratio.
Compared to the subjects with 11DhTx2/cre levels < 1500, there are no significant differences in the biochemical parameters such as creatinine, thyroid function tests, HbA1C and lipid parameters. Levels of 11DhTx2/ cre correlated with % abdominal fat (r = 0.19; p < 0.01), and IL-6 levels (r = 0.18; p < 0.01). Elevated 1DhTx2/ cre levels not associated with the other adipocytokines, duration of diabetes, use of insulin or micro-albumin.
4. DISCUSSION
Individuals with diabetes are at twoto fourfold increased risk of cardiovascular events compared with ageand sex-matched individuals without diabetes. In diabetic

Table 1. Clinical characteristics of subjects with premature coronary artery disease.
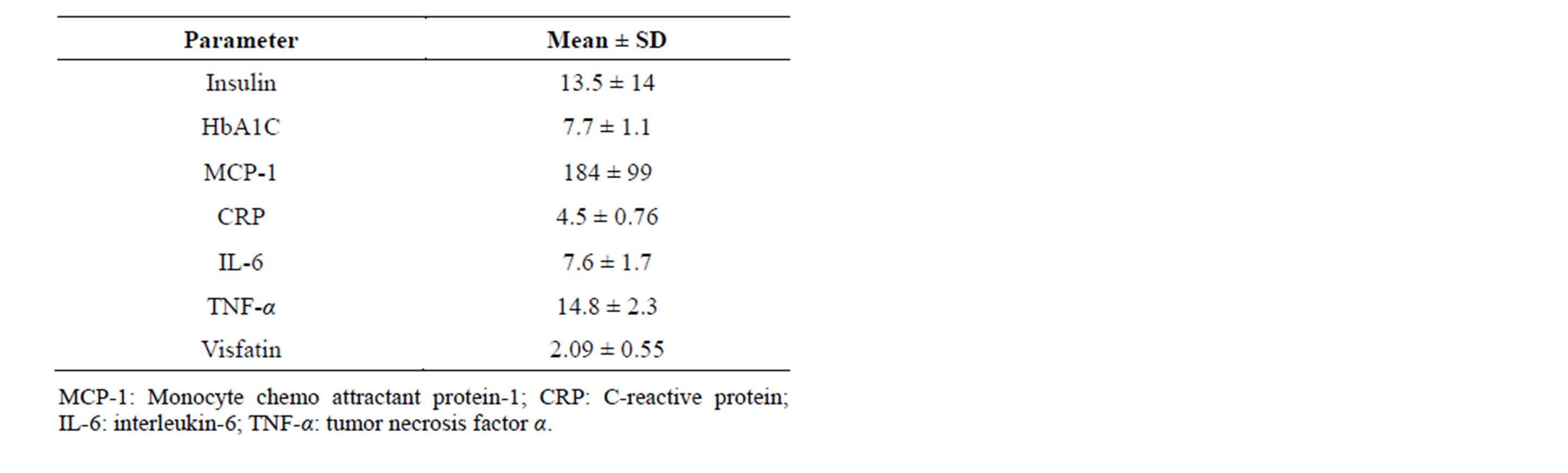
Table 2. Biochemical and adipokine parameters in subjects with Type 2 diabetes.

Table 3. Comparison of clinical parameters in subjects with Type 2 DM with or without aspirin resistance.
patients over the age of 65 years, 68% of deaths are from coronary heart disease (CHD) and 16% are from stroke. A position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation recommends enteric-coated aspirin at a dosage of 81 - 325 mg to be used as a preventive strategy in high-risk diabetic individuals. [2] Despite the proven benefits of aspirin therapy in the prevention of cardiovascular complications in the diabetic patient, the diabetic patient has a greater risk for thrombotic complications than non diabetic patients.
In a sub-analysis of the Japanese Primary Prevention of Atherosclerosis with Aspirin for Diabetes (JPAD) trial to evaluate the effect of low-dose aspirin on preventing atherosclerotic events in groups receiving different diabetes management, the study noted that low-dose aspirin (81 or 100 mg daily) reduced atherosclerotic events predominantly in the diet-alone group but not in the insulin or oral hypoglycemic agent user groups [11]. They also noted that patients treated with insulin had the longest history of diabetes, the worst glycemic control, and the highest prevalence of diabetic micro angiopathies and low dose aspirin did not affect atherosclerotic events (insulin: hazard ratio [HR] 1.19 [95% CI 0.60-2.40].
In our study, we found that AR is significantly high. Platelet aggregation depends upon several factors. Aspirin effect truly on generation of thromboxane. Hence measuring metabolites of thromboxane is appropriate. Most of the studies used platelet aggregometry was used to measure AR, which makes it difficult to compare our results with previous studies.
In an analysis from the aspirin-induced platelet effect (ASPECT) study, diabetic patients treated with 81 mg exhibited higher platelet function measured by VerifyNow, collagenand ADP-induced LTA, and 11-dhTxB(2) levels (p < or = 0.02 for all comparisons). Higher aspirin doses significantly inhibited platelet function and decreased aspirin resistance in diabetic patients (p < 0.05) [12].
5. URINARY 11-dh-TxB2
We noted that subjects with coronary artery disease have higher levels of 11 DhTxB2 levels. Our results are similar to the results in ASPECT study, where they reported that diabetic patients with CAD treated with 81 mg aspirin exhibit a higher prevalence of aspirin resistance and have significantly higher ADPand collageninduced platelet aggregation, 11-dh-TxB(2) levels [12]. They also noted that Both 162 and 325 mg aspirin significantly reduced levels compared with 81 mg aspirin in diabetic patients (p = 0.01 and 0.002, respectively).
On-going studies that will address the problem include: A Study of Cardiovascular Events in Diabetes (ASCEND), is being conducted in the U.K. has recruited 15,000 people with diabetes (either Type 1 or Type 2) who were not known to have vascular disease. ASCEND volunteers are randomly allocated to take either 100 mg aspirin daily or placebo (dummy) and 1 gram capsules containing naturally occurring omega-3 fatty acids (“fish-oils”) or placebo capsules containing olive oil. http://www.ctsu.ox.ac.uk/ascend/. The trial is started during 2004, and is scheduled to continue until 2017. The other study is Aspirin and Simvastatin Combination for Cardiovascular Events Prevention Trial in Diabetes (ACCEPT-D) is an open-label Italian primary prevention trial assessing whether 100 mg/daily of aspirin prevent cardiovascular events in patients without clinically manifest vascular disease and treated with simvastatin (starting dose 20 mg/day) comparing to no aspirin among adults over age 50 years with diabetes [13].
Statins to improve aspirin resistance: There is evidence that statins may be useful in treating aspirin resistance. Tirnaksiz and associates reported in a study of subjects with stable coronary artery disease, 11.2% were found to be aspirin resistant as measured by PFA-100, with a closure time of <186 seconds with collagen/ adrenaline cartridges. [14] After 3 months of statin therapy (atorvastatin 10 mg/day), 65% of the aspirin-resistant patients became aspirin sensitive by PFA-100 measurements (p < 0.0001). [14] Tekten and his colleagues have shown that statins reduced platelet aggregation [15].
Other suggested recommendations include: As saturated fat ingestion increases in vivo thromboxane production despite aspirin therapy, low dietary saturated fat intake and aggressive lipid management in diabetic patients on ASA therapy [16].
6. CONCLUSIONS
Aspirin resistance is high with 81 mg a day of aspirin among subjects with diabetes, who are at high risk for atherothrombotic episodes. Screening for aspirin resistance and alternative methods to improve response in those with AR is suggested.
ACKNOWLEDGMENTS
The residual funds from the Merit Review grant of Dr. Yaturu partly supported the study. Part of the support is by the research Pharmacy institute at Rensselaer, NY. Dr. Yaturu receives salary support from VHA.
The authors appreciate the proof reads by Barbara Youngberg.