Case report on the treatment of atrial fibrillation in a pregnant woman of 33 weeks’ gestation ()
KEYWORDS
Atrial Fibrillation; Pregnancy; Cardioversion
1. INTRODUCTION
This case involved the treatment of atrial fibrillation in a woman of 33 weeks’ gestation. There was no prior cardiac history. The only potential cause identified was infection given that she was being treated for a urinary tract infection.
Atrial fibrillation is the most common cardiac arrhythmia. It may cause no symptoms but is often associated with palpitations, chest pain or congestive cardiac failure. Patients are at risk of a thromboemoblic event. It can be managed by either controlling rate or rhythm with no difference in stroke risk between the treatments [1].
Rate control is often commenced at the time of diagnosis. This is done to decrease the heart rate but does not normalize the heart rhythm [2].
Physiologic changes of pregnancy can predispose women to cardiac arrhythmias however atrial fibrillation is still rare and usually occurs in women with underlying cardiac arrhythmias. Diagnosis requires exclusion of all possible aetiologies. Electical cardioversion as opposed to chemical cardioversion is the treatment of choice and pregnant women also require fetal growth surveillance and antenatal testing in persistent atrial fibrillation [3].
2. CASE PRESENTATION
AMcM was a 37-year-old female in her third pregnancy.
She presented to the Emergency Room of a general hospital complaining of flu like symptoms. At the time of presentation, she was 32 weeks pregnant with dichorionicdiamniotic twins.
She was diagnosed with a urinary tract infection, commenced on po cefuroxime, rehydrated in the ER and discharged.
She represented three days later complaining of sudden onset palpitations. There was no associated chest pain or dyspnoea. Electrocardiogram confirmed new onset fast atrial fibrillation.
She was admitted to the Coronary Care Unit. Medications were commenced including Metoprolol 50 mg od and Enoxaparin 1 mg/kg.
Echocardiogram was performed the following day. This showed mild mitral regurgitation with no other significant findings. In particular, there was no evidence of an atrial septal defect and there was no thrombus visualized in the left atrium.
The next day, she was transferred to our tertiary referral unit for further assessment and management. She was admitted to the High Dependency Unit for monitoring. Since commencing beta blockers, she experienced no further palpitations. ECG still confirmed the presence of Atrial Fibrillation (Figure 1). CTG monitoring and ultrasound scan confirmed normal biophysical profiles and Doppler flow in both twins.
She underwent cardioversion by the cardiology team. A consultant obstetrician was also present to intervene if there were unforeseen obstetric complications. Synchonised electrical cardioversion was used and the current delivered during the R wave of the QRS complex. Sinus rhythm was obtained MrsMcM remained well in the unit over the following four days. Twice daily ECGs confirmed sinus rhythm on each occasion (Figure 2). There were no further episodes of palpitations. MrsMcM was discharged and attended for outpatient cardiology care in her local hospital. She had an induction of labour with vaginal delivery at 38 weeks gestation
3. DISCUSSION
MrsMcM was correctly diagnosed with atrial fibrillation and treated appropriately. The risk of systemic embolisation in atrial fibrillation during pregnancy is probably due to circulatory statis in the atrium and left atrial appendage, and the hyperviscosity and hypercoagulable state of pregnancy with subsequent thrombus formation. The management of atrial fibrillation in haemodynamically stable pregnant women initially involves control of the

Figure 1. ECG on admission to the Rotunda Hospital.
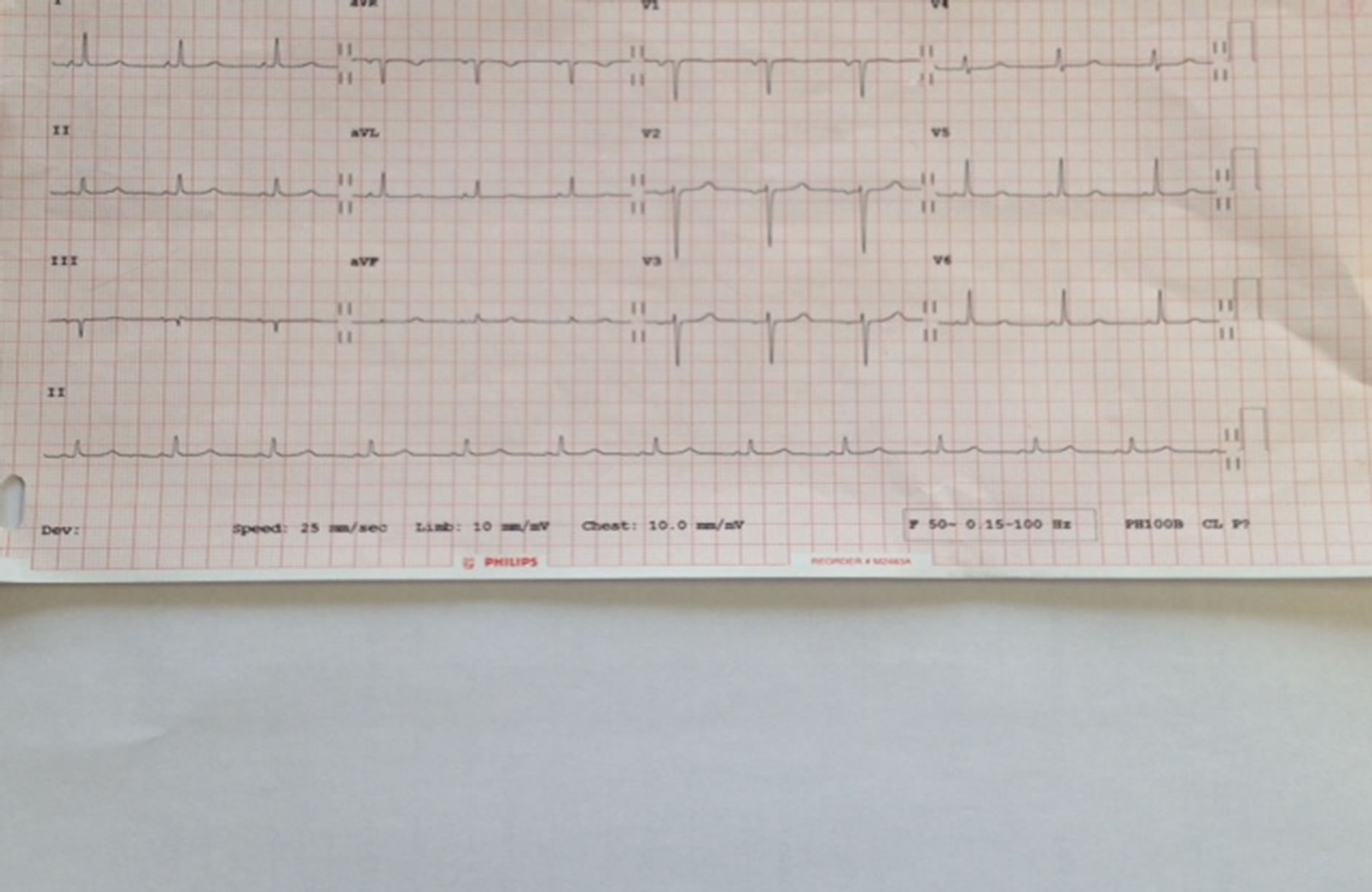
Figure 2. ECG in Rotunda Hospital post electrical cardioversion.
ventricular rate by digoxin, a beta blocker or a calcium channel blocker or a combination of these. In elective situations, rate should be controlled initially and this can later be followed by rhythm control using DC cardioversion [4].
It is rare for new onset atrial fibrillation to occur in pregnancy with no aetiology for same. Cases in the literature highlighted that most of these cases involve women with known pre-existing cardiac disease or where investigations confirm cardiac disease. In our case, echocardiogram was essentially normal. The only potential cause found is infection given that she was being treated for a urinary tract infection. We have found no cases such as ours in the Irish literature.
NOTES