Evaluation of X-Ray Doses on Children, from Paediatric Hospitals in Sudan ()
1. Introduction
Quality Assurance Programmes in diagnostic radiology have been developed in several countries in the past 16 years, mainly in Europe [1,2]. However, the need for special QAP for paediatric patients was first realised early in the 1980s [3,4]. The main goals were to improve the diagnostic information and to reduce the patient dose to a minimum ALARA principle [5]. The efforts towards QA in paediatric radiology were at first dominated by the principle of justification and also by the concepts of “efficacy/efficiency” [6,7]. The WHO Report 757 compiled such principles for a number of common diseases in paediatrics and emphasised the term “rational use of diagnostic imaging” [8]. The second important principle of “optimisation” [9] is contemplated by the document “Quality Criteria for Diagnostic Radiographic Images in Paediatrics” [10] and an earlier developed document for adults, “Quality Criteria for Diagnostic Radiographic Images” [11].
One of the main aspects on the implementation of QA programs is the calibration and maintenance of X-ray equipment and well-trained technicians. QAP [12] also intends to reduce rejection rates, improve image quality, reduce doses imparted to patients and consequently, reduce costs of radiology departments.
Quality assurance in paediatric radiology is still more important, since it is known that children are more sensitive to radiation than adults [13]. Therefore, in this case, closer attention should be paid to improve the diagnostic information, reducing the child dose as much as possible [14] as well as choosing the most convenient type of projection.
2. Materials and Methods
This study was carried out in three paediatric hospitals in Sudan: Hospital A (university Hospital), Hospital B and Hospital C (general hospital). The age intervals considered were 0 - 1 year, 1 - 5 years, 5 - 10 years and 10 - 15 years and the weight intervals from 1 - 10 kg, 10 - 20 kg, 20 - 30 kg, and 30 - 40 kg. In this work, two examination techniques were used, PA and AP projections.
The evaluation of the performance of the X-ray equipment in all three hospitals was performed by the Sudanese Atomic Energy Agency, however. Equipment maintenance is only corrective, not preventive.
The three hospitals are of medium size (around 140 beds each), however they have a very heavy workload, with approximately 8400 patients per month, each.
The examinations are performed by the technician and supervised by resident physicians. The main types of examinations are chest, skull and pelvis.
For each hospital and each projection, age, sex, weight and technical exposure parameters (tube voltage, current, time product, SSD) were recorded.
The X-ray machines used were FB-GT 22 (Hospital A), Siemens (Hospital B) and GE Beaver R201 (Hospital C). In this work, the number of patients was 31, 54 and 44 for A, B and C hospitals, respectively. The technical parameters used according to the type of examination and the patient age, varied from 36 to 78 kV for AP projection and from 36 to 70 kV for PA projection. With respect to the transportable charge, the values ranged from 1.8 to 20 mAs for AP projection and from 3 to 16 mAs for the PA projection.
A software package specially constructed for the evaluation of effective dose and body organ doses. Using this software, it possible to estimate patient doses knowing the X-ray tube output that must be measured using a calibrated ionization chamber at 80 Kv, FSD equal to 100 cm and a transportable charge of 10 mAs. For the calculation of the Entrance Surface Dose, and the effective dose with the use of relation (1) and (2) below, it is necessary as well, the knowledge of the back scatter factor (BSF), field size and tube filtration.
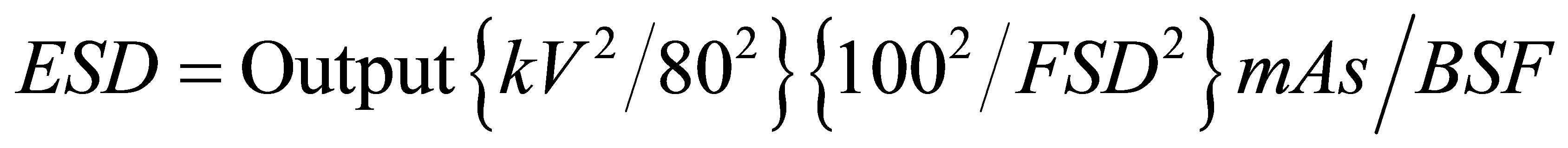 (1)
(1)
 (2)
(2)
where:
The standard output factor in  for the particular radiographic equipment used, measured under minimal scatter conditions at 1m from the tube focus at nominal 80 kV; mAs is the product of tube current and exposure time. And Cf(ED) is NRPB factor used to convert the ESD to ED.
for the particular radiographic equipment used, measured under minimal scatter conditions at 1m from the tube focus at nominal 80 kV; mAs is the product of tube current and exposure time. And Cf(ED) is NRPB factor used to convert the ESD to ED.
3. Results and Discussion
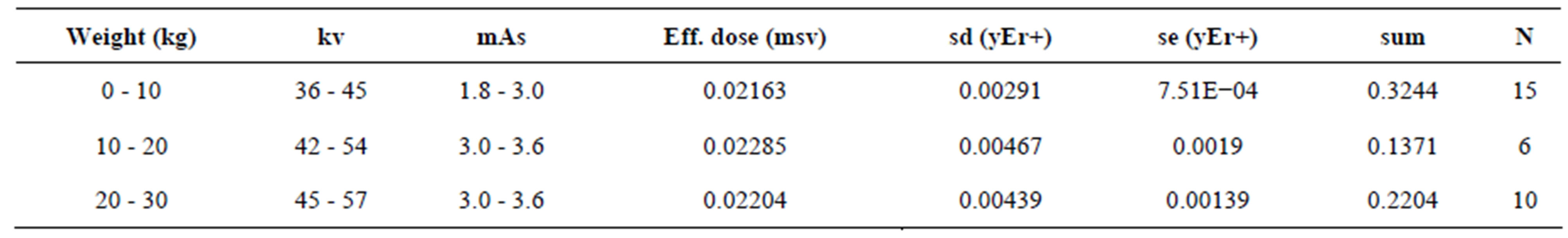
Results for effective doses according to weight are presented in Table 1, for the three hospitals.
The effective dose, which is directly related with the risk, depends on several factors: radiographic technique (kv, mAs, etc.), processing conditions, equipment calibration and performance, film-screen sensibility and the technicians’ expertise, among others.
 (a)
(a)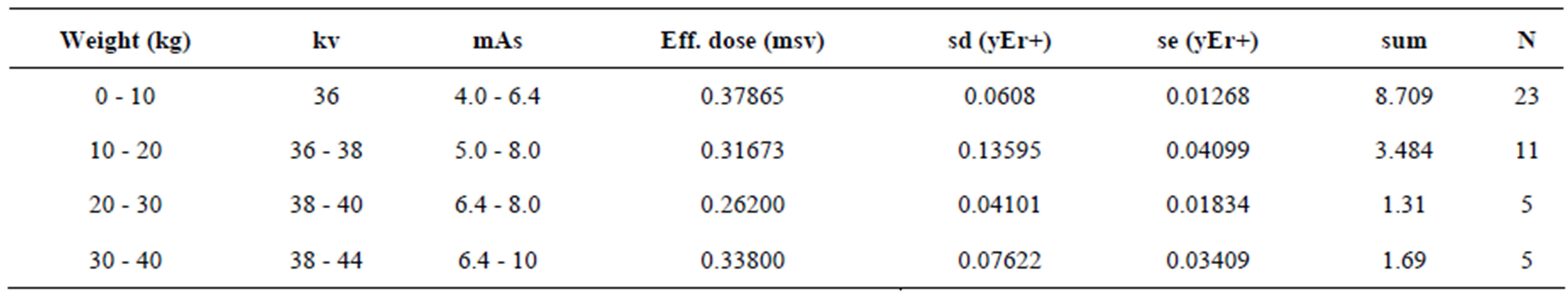 (b)
(b) (c)
(c)
Table 1. Values of effective doses according to weight for the three hospitals.
From the results presented in Table 1, where we take into consideration only the children’s weight, it can be seen that large differences in doses are present from one hospital to the other. The greatest difference registered was for the weight interval from 0 - 10 kg. In hospital B, the mean effective dose was 0.379 msv while in hospital A it was only 0.022 msv. Therefore, a difference of 1700% in the effective dose was detected between the two hospitals. It means that, children of up to 10 kg that take a chest X-ray in hospital B are likely to receive 17 times more radiation than those who take the same radiograph in hospital A.
Still analysing the results from Table 1, it can be seen that the radiographic technique for the three hospitals differs both, in kv and mAs. For the weight interval from 0 - 10 kg, where the largest difference in effective dose was detected, A and B hospitals use the approximately the same kV range. However, the mAs, ranges from 1.8 - 3.0 (mean value of 2.4) in hospital A, while in hospital B it ranges from 4.0 to 6.4 (mean value of 5.2). The mean mAs value in hospital B is at least doubled as compared to hospital A. This could be one of the causes of the higher effective doses.
On the other hand, analysing the radiographic technique of hospital C, for the same weight interval, it is seen that the kV ranges from 6 - 10 (mean value of 8), being consequently even higher than hospitalB. However, the effective dose for this Hospital is not the highest. In this case, the relatively low effective dose could be accounted for better equipment (more modern and/or with appropriate maintenance), more adequate processing conditions, and/or technicians better trained.
Table 2 presents the results of effective dose in terms of age intervals.
Analysing effective doses for the three hospitals, it is found that the worst situation is also for the smallest babies, from 0 - 1 year, and Large discrepancies were encountered between A and B hospitals.
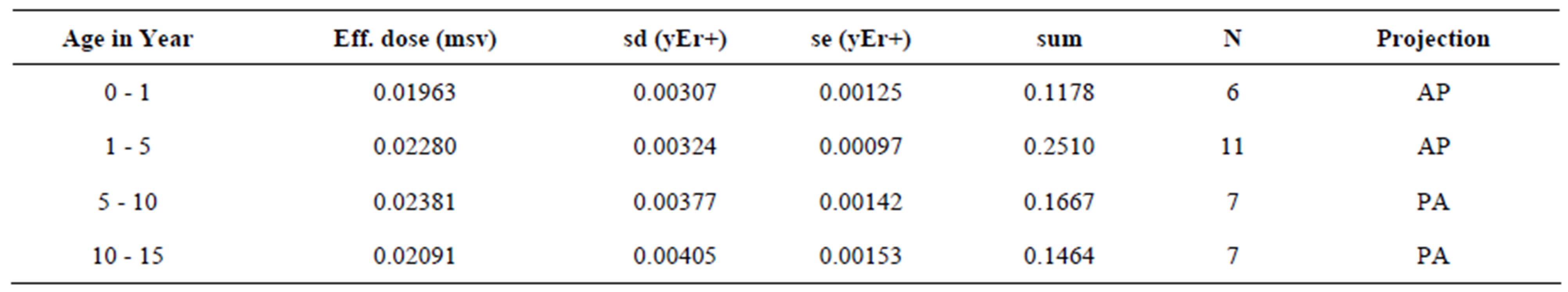
In Table 3, organ doses are shown for the three hospitals, for AP and PA projections.
Concerning organ doses, for AP projection presented in Table 3; once more the highest values were encountered in hospital B. Comparing B and hospitals A, the organs that presented the highest doses, in the two hospitals were: breast (0.272 and 0.015 mSv), thymus (0.224 and 0.013), heart (0.150 and 0.008), thyroid (0.130 and 0.008) and lungs (0.121 and 0.007) respectively. For these organs the increase in doses from hospital A to hospital B is again around 17 to 18 times.
Analysing the results from the three hospitals and now considering PA projection, as compared to AP projection, much higher doses for the PA projection were
 (a)
(a) (b)
(b)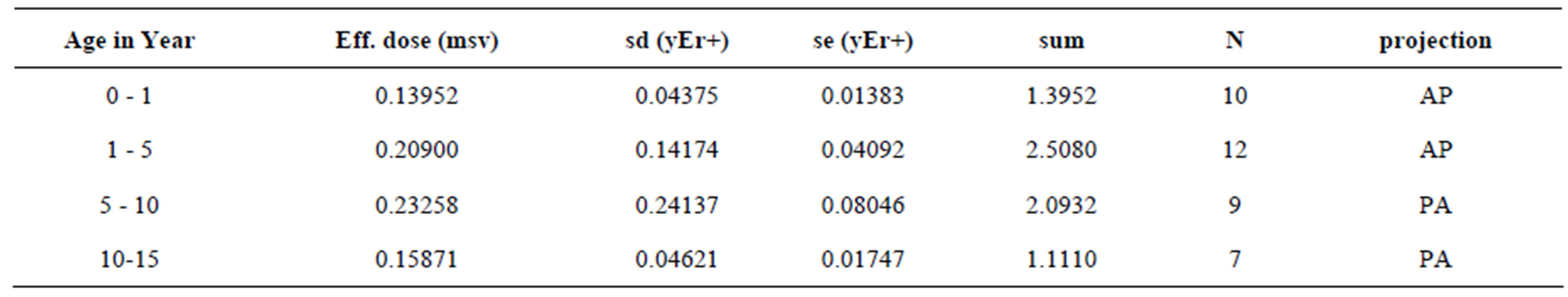 (c)
(c)
Table 2. Effective doses according to age interval for the three hospitals.

Table 3. Organ doses calculated with the use of a dosimetry software for the three hospitals for both, AP and PA projections. Body organ dose in (mSv) for (AP projection)and (PA projection).
found in some body organs due to their location with respect to the direction of the incident beam. This fact is of special concern in paediatric radiology because little babies are more likely to suffer the effects of radiation and have longer life expectation. Therefore, physicians, when deciding for a certain type of projection, they should be aware of these differences to be able to decide which the most adequate technique to be chosen is. Probably, in some situations, not only scattered radiation is measured, but also the direct beam, since new-borns bodies are very small and are almost completely irradiated during examination. In this particular case, proper collimation would certainly reduce doses significantly.
4. Conclusions
In hospital B, the doses are always higher compared to hospital A, so care should be taken in this hospital to avoid the potential health hazards to paediatrics patients due to exposure during X-ray diagnostic. On the other hand, hospital A presents the lowest dose values for all age range. The reason is that Hospital A is paediatrics university hospital with a very well trained staff to work with neonates and children in general, the other two hospitals considered in this work are general hospital not dedicated for paediatrics, their staff have no special training to work with children, their equipments and procedure are normally adapted for adults.
In Table 3, the BOD can be seen for Ap and PA projection respectively, and it has been seen that the AP projection delivers high dose to the Brest and thyroid and should be avoided whenever possible specially for girls.
By the results shown above, we can conclude that a lot can be done to reduce doses in radiology, being of special concern of paediatric departments. The importance of the implementation of Quality Assurance Programs in radiology departments should be stressed because most of the non-conformal working conditions that are here reflected by the differences in doses could be controlled if a QAP was implemented on a regular basis. X-ray equipment properly calibrated, with a good maintenance schedule, correct processing conditions, adequate screenfilm combination and well-trained technicians are among the most important items to be considered. It is also of great importance to instruct physicians about the basic principals of radioprotection so that they would be aware of the correct methods to reduce radiation risks in infants.