Fast Track Extubation Post Coronary Artery Bypass Graft: A Retrospective Review of Predictors of Clinical Outcomes* ()
Abstract
Introduction: Fast track (FT) cardiac surgery and early extubation (EE) are aimed at safe and effective rapid post-operative progression to discharge, and have been practiced for more than two decades. Their goal is to optimize patient care perioperatively in order to decrease costs without negatively affecting morbidity and mortality. However, the factors that predict successful EE are poorly understood, and patients with significant co-morbidities are frequently excluded from protocols. We hypothesize that independent of disease severity, early extubation leads to shorter hospital stays and can be performed safely without negatively affecting outcomes. Materials and Methods: We performed a retrospective review of 919 patients who underwent coronary artery bypass grafting (CABG) at the Southern Arizona Veteran’s Affairs Health Care System medical center over 7 years. We collected pre-operative data regarding patients’ NYHA classification, presence and severity of cerebral vascular disease, peripheral vascular disease, pulmonary disease, diabetes and hypertension. Intra-operative variables were also recorded including ASA scores, ischemic times, and time to extubation. Finally, post-operative variables such as rates of reintubation and tracheotomy, and both length of ICU and total hospital stay were also compared. Results: Prolonged periods of ischemia were found to predict a delayed extubation (HR = 0.992; CI = 0.988 - 0.997, p = 0.0015) while small body surface area (HR = 1.57; CI = 1.13, 2.17, p = 0.007) and higher pre-operative functional status of the patient, such as independent versus dependent status (HR =1.68; CI = 1.30 - 2.16, p < 0.0001), or partially dependent to fully dependent status (HR = 1.33; CI = 1.03 - 1.70, p = 0.03) were found to be associated with earlier extubation. The early extubation (EE) group (those extubated in less than the median 7.3 hours) had an average hospital stay of 5.1 ± 4.0 days, versus 7.8 ± 8.1 days in the delayed group (>4 hours), p < 0.0001. The EE group also experienced shorter ICU stays by about 1 day (EE, 1.9 ± 4.2 v. conventional, 3.8 ± 17.3, p = 0.02). There were no differences in rates of tracheotomy or re-intubation between groups. Conclusions: In our study population, pre-operative functional class and total body surface area predicted those patients able to tolerate early extubation after cardiac surgery. Prolonged ischemia resulted in delayed extubation. Patients that were extubated in less than 4 hours had shorter ICU and hospitalization stays, while there was no significant difference between the two groups in rate of reintubation or tracheotomy.
1. Introduction
Today, the need for high quality and cost-effective care of surgical patients has lead to an increased focus on methods for decreasing length of ICU and total hospital stays. In regards to cardiac surgery, approximately 500,000 coronary artery bypass graft (CABG) procedures are performed annually in the United States at a substantial cost to the healthcare system [1]. As a result the development of fast track (FT) and early extubation (EE) management protocols have been developed to provide safe, effective and rapid post-operative progression to discharge of post CABG patients [1]. This approach has been practiced for more than two decades beginning back in the 1990’s ,when “fast-track” protocols were developed and since associated with decreased lengths of stay (LOS) without negatively affecting outcomes [2,3] and potentially lowering rates of ventilator associated pneumonia [4].
Despite these benefits, the key factors associated with successful EE and FT post-operative management are poorly understood. Consequently, it is unclear if patients with significant comorbidities should be excluded from EE. The purpose of this paper is to review and evaluate the safety and efficacy of early extubation in patients undergoing coronary artery bypass grafting in terms of their preoperative disease severity.
2. Materials and Methods
Institutional Review Board approval was obtained prior to the study. We performed a retrospective chart review of all patients who underwent an isolated coronary artery bypass grafting (CABG) at the Southern Arizona Veteran’s Affairs Health Care System medical center over 7 years. All patients undergoing additional valve replacement at the time of surgery were excluded from analysis. We collected demographic data including age, gender, height, weight, and body surface area. The patient’s preoperative condition and disease severity was documented based on the following variables: cerebral vascular disease, NYHA classification, presence of pulmonary disease, diabetes, hypertension and degree of peripheral vascular disease.
Data collected regarding the intra-operative course included: ASA scores, ischemic times, number of grafts implanted and time to extubation. Extubation times were noted and calculated from the time patient left the operating room to time of endotracheal tube (ET) removal. Additional data regarding re-intubation rates, requirement of tracheotomy, and length of ICU and total hospital stay were also recorded.
Additionally, a Charlson co-morbidity index, a previously validated scoring system aimed at predicting the ten-year mortality of patients with chronic illnesses and co-morbid conditions including heart disease [5,6] was calculated for each patient.
Patient demographics were calculated using means and standard errors. Statistically significant changes in length of intubation over time were detected via a one-way ANOVA. A Cox proportional hazards model which is a statistical technique for exploring the relationship between the survival of a patient and several explanatory variables was used to identify variables that predicted longer intubation times [7]. Finally, comparison between early extubation groups and delayed groups was performed using Fisher’s exact test for discrete variables and by two tailed t-test with unequal variances for continuous variables. The significance threshold for all tests was defined as < 0.05.
3. Results
A total of 919 patient records met the study inclusion criteria. Table 1 shows patient demographics. The mean patient age was 64.9 ± 8.6 years. Over 98% were male and had a mean weight of 198.6 ± 38.8 lbs. Comorbidities were common in the cohort; 96.6% of the patients were ASA class 4, and 37.7% had been diagnosed with chronic obstructive pulmonary disease and 34.6% with diabetes. Additionally 21.6% had a history of smoking and 47.5% had a history of prior myocardial infarction.
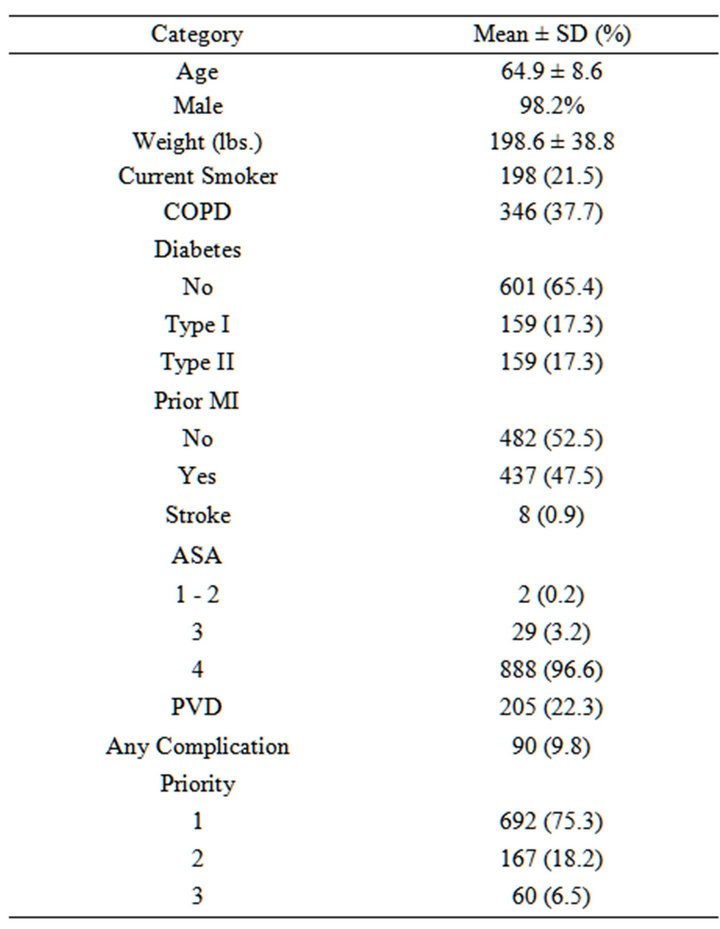
Table 1. Demographics of study cohort (N = 919). The mean age was 64.9 ± 8.6, majority of patients were males. The mean weight was 198.6 ± 38.8 lbs. 21.6% were current smokers; there were 37.7% with a diagnosis of chronic obstructive pulmonary disease (COPD) prior to surgery. 47.5% had a prior myocardial infarction (MI). 34.6% had diabetes.
To better understand the severity of patient comorbidity and their long-term mortality risk, we calculated the mean Charlson score for the patients included in the study by year of surgery. The results of these calculations are given in Table 2. Overall, the mean Charlson score was 5.99 ± 2.54. Additionally, over time there was a statistically significant trend toward decreasing Charlson score as determined by one-way ANOVA (p < 0.0001).
A log-rank test was performed for time to extubation by year of surgery. The p-value for both overall and trend log-rank tests for surgical years was <0.0001, indicating that there were significant differences in time to extubation between surgical years. As shown in Figure 1, it is possible to see a clear decrease in extubation time over the study period. This trend coincides becomes most apparent around 2004, where we see a distinct transition from a linear decrease in Extubation-free probability over time to a high probability of extubation within 7 hours of surgery. This coincides with a decisive change in management at our institution, to move to more rapid extubation in our patients following coronary artery bypass graft procedures.
The median time to extubation for all records was less than 7.3. We then divided the records into two groups, the EE group (extubated in less than 7.3 hours) and the

Table 2. Mean Charlson score by surgical year. The overall score calculated for this population was 5.99 ± 2.54. The overall trend appears to be a decreasing Charlson score over time. Based on one-way ANOVA, the p-value for surgical year is <0.0001 indicating that the mean Charlson score significantly varies by surgical year. According to Turkey’s HSD post hoc test, 1995 > (1998, 1999, 2000, 2005, 2006, 2007); 1996 and 1997 > (1998, 1999, 2000, 2001, 2002, 2004, 2005, 2006, 2007).

Figure 1. Kaplan-Meier curves for time to extubation by surgical year showing the extubation free probability on the Y axis and time to extubation on the X axis. Each curve represents a single surgical year, with a trend toward shorter extubation times over time. This was a statistically significant difference in time to extubation by surgical year as indicated with a log rank p-value of <0.0001.
conventional group (extubated in more than 7.3 hours). Comparing the two groups we found statistically significant differences in length of ICU and total hospital stay. The early extubation group had an average hospital stay of 5.10 ± 4.03 days, versus 7.78 ± 8.14 days in the delayed group (two tailed t-test, p < 0.0001). The early extubation group also had shorter ICU stays than the delayed extubation group by about 1 day (1.92 ± 4.17 vs. 3.80 ± 17.29, p = 0.02). Notably, there was no significant difference in the tracheotomy rates between the two groups nor was there any difference in the frequency of re-intubation.
Table 3 shows the results of the Cox proportional hazard model adjusted for age and gender to determine the variables that were predictive of time to extubation. These results show that longer ischemic times predicted delayed extubation (HR = 0.992; CI = 0.988-0.997, p = 0.0015). Additionally, lower body surface area (HR = 1.57; CI = 1.13, 2.17, p = 0.007) and more independent patient functional status prior to surgery, classified as independent versus fully dependent (HR = 1.68; CI = 1.30 - 2.16, p < 0.0001), or partially dependent versus fully dependent (HR = 1.33; CI = 1.03 - 1.70, p = 0.03) were associated with earlier extubation times.