Thyrotoxicosis Related Coronary Artery Spasm Presenting as Acute Coronary Syndrome ()

1. Introduction
Coronary artery spasm (CAS) defined by a severe reversible diffuse or focal vasoconstriction is the most common diagnosis among ischemia with no obstructive coronary artery (INOCA) disease patients irrespective to racial, genetic or geographic variations. A wide spectrum of clinical manifestations from silent disease to sudden cardiac death has been attributed to this complex entity with unclear pathophysiology [1] . Multiple mechanisms such as the autonomic nervous system, endothelial dysfunction, chronic inflammation, oxidative stress and smooth muscle hypercontractility are involved. Regardless of the limited benefits proffered by the newly emerged cardiac imaging modalities, the provocative test remains the cornerstone diagnostic tool for CAS. It allows to reproduce CAS and to evaluate reactivity to nitrates. Different invasive and noninvasive therapeutic approaches are approved for the management of CAS [1] .
Thyrotoxicosis can cause acute chest pain without ST-segment changes on electrocardiogram (ECG) due to coronary artery spasm [2] . This diagnosis can be particularly challenging as the symptoms may mimic acute coronary syndrome. The diagnosis of coronary artery spasm is confirmed by coronary angiography. The use of intracoronary nitroglycerin can relieve spasm and reveal the true extent of coronary artery disease [3] .
We present a case of a perimenopausal woman with newly diagnosed hyperthyroidism who presented with chest pain. Coronary angiography showed spasm of the left main coronary artery and right coronary artery which was relieved by intracoronary nitroglycerin.
The possible mechanisms of coronary occlusion with thyrotoxicosis include significant underlying coronary atherosclerosis, direct damage to coronary artery and coronary embolization. Thyroid hormones affect the cardiovascular system by increasing stroke volume and heart rate. Several hypotheses have been proposed for the mechanism of thyroid hormone and coronary artery spasm [4] . The basic hypothesis is sensitization of the coronary arteries related to the thyrotoxic state. In addition, coronary spasm produces a higher chance of atherosclerotic events owing to thrombus formation and fibrinolysis delaying [5] . Thyrotoxicosis also leads to a hypermetabolic state and causes imbalance between blood supply and oxygen demand, resulting in cardiac symptoms [2] .
2. Case Presentation
A 41 years old lady, with no known past medical history presented with cardiac chest pain for the first time. It was central, non-radiating and associated with vomiting and sweating. The pain was intermittent for last one month and was associated with dry cough and weight loss of approximately 20 kilograms (KG).
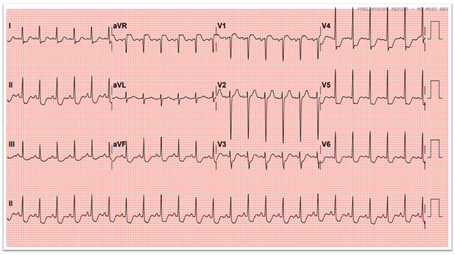
Her ECG showed sinus rhythm with ST-segment depression in the infro-lateral leads that were dynamic (Figure 1(a)) and improved after sublingual nitrate (Figure 1(b)). Her troponin level initially was 250 ng/L then increased to 310 ng/L. In view of her chest pain we started her on anti-ischaemic treatment.
On subsequent laboratory tests she was found to have severe thyrotoxicosis for which she was commenced on Carbimazole and a beta blocker. Transthoracic echocardiography showed preserved left ventricular systolic function.
(a)

(b)
Figure 1. (a) Case ECG: initial on presentation; (b) Case ECG: Follow up after GTN Sublingual tab.
She then proceeded to coronary angiography that showed severe diffuse spasm, particularly involving the ostium of the right coronary artery (RCA) (Figure 2(a)) and left main coronary artery (LMCA) (Figure 3(a)). This improved after multiple boluses of intracoronary nitrate (Figure 2(b)) and (Figure 3(b)). No atherosclerosis coronary artery disease was noted.
3. Discussion
At a glance, coronary spasm or vasospastic angina (VSA) has become a common disease. On the contrary, there are several uncertain or unsolved problems regarding coronary spasm, including the presence of medically refractory coronary spasm (intractable VSA), or an appropriate use of implantable cardioverter defibrillator in patients with cardiac arrest who have been confirmed as having coronary spasm [4] .
![]() (a)
(a) ![]() (b)
(b)
Figure 2. (a) Angiographic finding of RCA, showing severe spasm at the RCA ostium (blue arrow) pre GTN intracoronary injection. (b): Angiographic finding of RCA, showing no spasm or lesion in the ostium (blue arrow) post GTN intracoronary injection.
![]() (a)
(a)![]() (b)
(b)
Figure 3. (a): Angiographic findings. Showing severe spasm in LMCA, pre GTN-intracoronary injection (blue arrow). (b): Angiographic findings. Showing no spasm or lesion in LMCA, post GTN intracoronary injection (blue arrow).
VSA is characterized by severe chest pain at rest with concurrent ST-segment changes on ECG. Patients may also experience ventricular arrhythmias and complete atrioventricular block, which can occur even in the absence of chest pain. The pathophysiology is related to vagal withdrawal and a change in sympathetic activity, smooth muscle hyper-reactivity, and endothelial dysfunction. Prior studies report a genetic role in some populations as well as an association with cigarette smoking, type A behavior patterns, anxiety or panic disorders, and use of cocaine, amphetamines and other drugs. While some data suggest coronary artery spasm may be more common in women, other observational studies indicate a greater frequency in men (ref required). Racial differences have also been documented, with the highest occurrence in Japanese populations [5] .
Vasoconstriction causing acute coronary syndrome (ACS) can be located also at the microvascular level. Intense coronary microvascular vasoconstriction is diagnosed by rise in cardiac enzymes as it is the case for several autoimmune diseases. The uses of biomarkers that are specifically involved in the mechanisms of disease could greatly impel the early identification of patients with ACS in whom inflammation plays a key pathogenetic role [6] .
According to the guideline on coronary spasm, the recognition of transient changes in ST-T segments on ECG during chest symptoms, as well as the presence of chest symptoms derived from coronary spasm, including the good responses to sublingual nitroglycerin and timing of occurrence of coronary spasm at rest, during sleep, or early in the morning, is very important in the diagnosis of VSA [4] .
4. Conclusions
The length of the CAS episode is important in terms of clinical manifestations from the asymptomatic event to the different aspects of ACS (unstable angina, NSTEMI, and STEMI) and sudden cardiac death. This is thought to be the result of the autonomous nervous system involvement in the pathophysiology of it [1] .
Any stenosis found on coronary angiography of a thyrotoxic patient, the possibility of coronary artery spasm must be explored. Our case emphasizes the use of intraprocedural nitroglycerin in these patients, which can relieve the spasm and reveal the true extent of coronary artery disease. Restoration of euthyroid is the cornerstone of management and abates the need for long-term coronary vasodilator medications [3] .
Anti-thyrotoxicosis and anti-anginal medications should be used actively. Beta-block agents are strongly recommended and should be titrated gradually to the maximal doses that patients could tolerate [2] .