Cervical Myelopathy: Diagnostic Aspects, Surgical Treatment and Evolution of Patients Operated upon in Yaounde ()
1. Introduction
Cervical myelopathy is a spinal cord disorder resulting from a reduction of the cervical diameter of the spinal canal due to degenerative phenomena [1] . It accounts for 55% of myelopathies in adults over the age of 50 years [2] [3] and is caused by static and dynamic factors [4] [5] . The clinical presentations include the ataxospasmodic form, where gait and balance disorders predominate; amyotrophic form, in which the upper limbs are predominantly affected; spastic paraparesis form; Brown Sequard syndrome form; and the forms evolving with progression [6] . The common combination of clinical presentation is clumsiness of the hands, gait problems, and progressive cervicobrachial neuralgia [7] . Magnetic resonance imaging (MRI) is the preferred diagnostic examination, supplemented by computed tomography (CT) and standard radiography [8] . The value of dynamic cervical MRI in surgical planning has also been demonstrated in the literature [5] [9] . The goal of surgical treatment is to prevent neurological worsening [10] by decompressing the spinal cord and roots and restoring adequate spinal statics. The surgical decision in the case of cervical myelopathy is based on radiological criteria (compression of the spinal cord with absence of cerebrospinal fluid [CSF] around the cord, the presence of spinal hypersignal in a T2-weighted sequence) and clinical criteria (progression of neurological symptoms and deficits with significant and recent functional effects). The surgical approach can be anterior, posterior, or combined. Surgery can be indicated by the Nurick grade and the modified Japanese Orthopaedic Association (mJOA) score. However, in our context, the few available studies that have described the clinical and surgical aspects of the treatment in patients were published two decades ago. With the technical improvements, in particular, the availability of MRI devices and the creation of new neurosurgery centres, the recommendations proposed in the literature have been increasingly incorporated in patient management. Thus, it is important to determine the Nurick grade at which surgery leads to good functional outcomes and the arguments in the context of our research that led to choosing the anterior or posterior approach. Therefore, this study aimed to describe the clinical presentation, current surgical treatment, and progression of cervical myelopathy.
2. Materials and Methods
2.1. Type of Study and Location
This was a 10-year retrospective and descriptive cross-sectional study conducted between January 2011 and January 2020 in the neurosurgery departments of the Central Hospital, the Military Hospital, and the General Hospital of Yaoundé. These neurosurgery centres are the only ones in Yaoundé and they supervise the university neurosurgery training programme in Cameroon.
2.2. Study Population and Inclusion Criteria
All complete medical files of patients who underwent surgery for cervical myelopathy during the study period were consecutively included. The diagnosis of cervical myelopathy was made using spinal MRI; additionally, in some cases a CT scan of the cervical spine was used in cases where MRI was unavailable. Standard radiography was systematic. Severity of myelopathy was assessed using the Nurick grade.
2.3. Study Variables
The variables of the study were obtained from medical files: age; sex; circumstances of discovery; clinical presentation; imaging data of radiography, CT, and MRI (static disorder, area of compression, level of compression, and signs of spinal cord injury); surgical treatment (indications and approaches); and the progression of patients who underwent surgery. Patients were followed up in an outpatient setting at 3 months, 6 months, 1 year, and on demand depending on their progress. Patients living far away from neurosurgery centres were contacted by telephone for follow-up after 1 year. The postoperative evaluation was clinical using the Nurick grade (Nurick classification system) at six months and one year, and we asked X ray for patients who had undergone stabilisation to assess the correct placement of the implant and to evaluate sagittal balance.
2.4. Statistical Analysis
The data were analysed using the Epi info software 7.2.2.6 and Excel 2013.
2.5. Ethical Consideration
The protocol of our study was submitted to the University and we have obtained ethical clearance of this study. We have also obtained administrative authorizations from Central Hospital, Military Hospital and General Hospital of Yaounde.
3. Results
Overall, 61 patients were operated on for cervical myelopathy during the study period out of 434 patients who underwent surgery for degenerative pathologies of the spine, i.e., a rate of 14.05%. We retained 52 patients: 26 patients from Central Hospital, 14 patients from Military Hospital and 12patients from General Hospital as showed in Diagram 1.
3.1. Demographic, Clinical, and Radiological Characteristics
The average age was 52 ± 10 years with extremes between 40 and 82 years. The predominant age group was between 50 and 65 years (Figure 1). The M/F sex ratio was 3/1. The onset of symptoms was progressive in 86.54% and post-traumatic in 13.46% of the patients. The main clinical presentation was gait problems (100%) associated with cervicobrachial neuralgia (59.62%); motor deficiency was noted in 47 patients (90.38%), sphincter disorders in 8 patients (11.38%), and sexual problems in 3 patients (5.77%) (Table 1). The diagnosis was made with MRI in 76.92% and CT in 23.07%. All patients underwent standard radiography. Most patients (67.30%) had three or four levels of compression, and spinal hypersignals were present in 9 patients (22.50%) (Table 2). The Nurick classification was grade 0 and 1 (0%), grade 2 (17.31%), grade 3 (38.46%), grade 4 (32.69%), and grade 5 (11.54%).
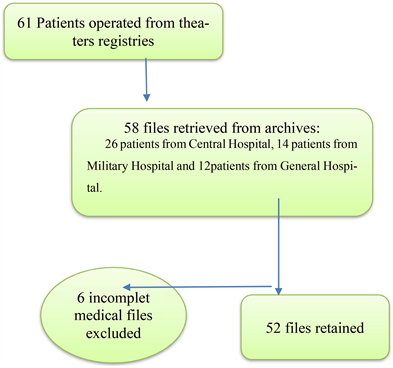
Diagram 1. Flow diagram.
![]()
Figure 1. Patient age range distribution
![]()
Table 2. Radiological presentation.
3.2. Surgical Treatment and Evolution
The surgical indication was decided based on the Nurick grade. Grades 3 (38.46%) and 4 (32.69%) represented the majority of indications (Figure 2). The surgical approach was posterior in 86.54%. Decompressive laminectomy was used in all cases with stabilisation in 8% of cases. The anterior approach was performed in 13.46% of cases. It involved a discectomy with the placement of a graft and a screwed plate. The anterior approach was essentially used in patients with one or two levels of compression. The postoperative progression at one year using the Nurick grade showed an improvement in 82%, no progression in 8%, and a worsening in 6% of patients (Figure 3 and Figure 4). Notably, 21% of the patients had a follow-up at 2 years, and the average follow-up of patients was 4 years with a range of 1 - 10 years.
![]()
Figure 3. One-year post-operative evolution.
![]()
Figure 4. Pre and post-operative Nurick score evolution at one year.
4. Discussion
The patients who underwent surgery during the study period were relatively young and predominantly male. The clinical presentations were mostly advanced. In addition to MRI, we used radiography to evaluate the spinal statics. Three quarters of the patients had three or four levels of compression. The surgical indication was based on the Nurick grade: the majority of patients had grades 3 and 4. The surgical approach was anterior in the case of one or two levels and posterior in the case of 3 levels or more. The progression after surgery was characterised by an improvement in the neurological condition in the majority of cases.
4.1. Demographic Characteristics
Cervical myelopathy is a relatively common pathology in our environment. It represents 14% of surgical indications among degenerative spinal pathologies. The most represented age group was between 50 and 65 years; the average age of the patients was 52 ± 10 years. In Morocco, Djoubairou et al. [11] also found in 2014 that the average age of patients was 52 years. This relatively young age was also predominant in other African studies [12] - [17] compared to Western studies, where the average age was higher [1] [5] [9] .
4.2. Clinical Characteristics
The onset of symptoms is usually progressive for the given clinical form. Cervical myelopathy can appear following trauma. In our series, 13.46% of patients presented with decompensated myelopathy due to cervical spine trauma. Previous studies have reported that 15% to 20% of patients are admitted after decompensation following cervical spine trauma [12] [13] . The clinical presentation consists predominantly of gait problems (100%), followed by cervicobrachial neuralgia (59.62%) and neck pain (42.31%). In particular, this is the usual clinical presentation of cervical myelopathy. The radicular or medullary signs depend on the level of compression. Gait problems can be of the cord type in the case of posterior compression and spastic in the case of anterior compression. Neck pain is generally found in a static disorder. Almost all patients had a sub-lesional motor deficit (90.38%). Nurick grades 4 and 5 were found in one-third and 11% of patients, respectively, indicating late arrival of patients for a neurosurgery consultation, which poses a problem in diagnosing of cervical myelopathy. Notably, Nyada et al. [14] in Cameroon, Hima Maiga et al. [12] in Niger, and Loembe [15] in Gabon also found similar results.
4.3. Radiological Characteristics
MRI is the preferred examination method to assess the elements of anterior (herniated disc, ossification of the posterior common vertebral ligament) and posterior (hypertrophy of the yellow ligament) compressions. It is also used to detect the presence of a medullary hypersignal in a T2-weighted sequence or a spinal hyposignal in a T1-weighted sequence, which is a factor of poor prognosis [16] . CT is performed for bone assessment, and dynamic radiography for the analysis of spinal statics. Dynamic cervical MRI has reportedly been valuable in surgical planning [9] . MRI was performed in 76.92% and CT in 23.07%. MRI has been the systematic examination for almost 6 years, but patients who underwent surgery and were examined with CT were older. The medullary hypersignal was found only in 22% of the patients and the majority of the patients had at least three levels of compression.
4.4. Surgical Treatment and Evolution
The goal of the treatment is to prevent a deterioration in the neurological status of the patients. The surgical decision in the case of cervical myelopathy is based on radiological criteria (compression of the spinal cord with absence of CSF around the cord, the presence of spinal hypersignal in a T2-weighted sequence), and clinical criteria (progression of neurological symptoms and deficit with significant and recent functional effects). In this study, surgery was indicated for a Nurick grade ≥ 2. All patients who underwent surgery with a Nurick grade of 5 (11%) had experienced cervical spine trauma leading to decompensation of the pre-existing myelopathy. Of them, 86.54% underwent the posterior approach, which was similar to the results of Hima Maiga et al. [12] whose approach was exclusively posterior. This result was unlike those of Ahanogbe et al. [17] with a series of 12 cases in Togo and Loembe et al. in Gabon [15] where the approach was anterior in 83.33% and 100% of patients, respectively. In this study, an anterior approach was applied in a patient with one or two levels of compression (Image 1), in which discectomy with iliac graft or cage and a screwed plate was performed (Image 2). The posterior approach was indicated in patients with three or more levels of compression (Image 1), in which laminectomy was performed. Posterior stabilisation (Image 3) was indicated in patients with kyphosis or mobile listhesis shown on dynamic radiography. The progression at 1 year after surgery measured by the Nurick grade showed an improvement in the neurological status in 82%. Prognostic factors include age, duration of symptoms, preoperative neurological status [18] , and the presence of a hyposignal in a
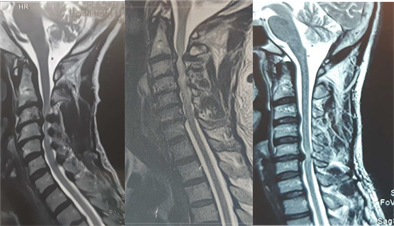
Image 1. Left: MRI: C3-C6 cervical myelopathy: hypertrophy of the yellow ligaments; Middle: MRI: C2-C7 cervical myelopathy: T2-weighted hypersignal; Right: MRI: C5C6 cervical myelopathy by disc herniation with hypersignal.

Image 2. Left: cervical spine MRI, sagittal view: C5-C6-C7 cervical myelopathy. Right: control x ray anterior approach C5-C6, C6-C7, discectomy, cage and plate.

Image 3. Left: cervical spine MRI, sagittal view: C3-C4-C5 cervical myelopathy with a mild kyphosis. Right: control x ray, posterior approach C3-C4-C5, laminectomy and stabilization.
T1-weighted sequence [16] . In our study, clinically speaking, 63.46% of patients were under 65 years of age and 71.15% were classified as Nurick grades 3 and 4. On the radiological level, there was a spinal cord hypersignal in the T2 sequence in 22.5%, and no patient had a spinal cord hyposignal in the T1 sequence. The study involved relatively young patients, most of whom did not show severe signs of myelopathy on MRI. Bedridden patients were those who had experienced cervical spine trauma. In Hima Maiga et al.’s study [12] , half of the patients who underwent surgery and were considered to have Nurick grade 5 remained in the same condition and the condition worsened in 20%.
4.5. Study Limitations
This was a retrospective study and the data obtained by telephone during the postoperative evaluation at one year constituted the limit in terms of their reliability.
5. Conclusion
Cervical myelopathy is a relatively common pathology in our environment. In our study, the patients who underwent surgery were relatively young, the clinical presentations were mostly advanced, and most of the patients arrived late for their neurosurgery consultation. In addition to MRI, we used radiography to evaluate the spinal statics. The surgical indication was based on the Nurick grade and the surgical approach depended on the number of compression levels. The progression after surgery was characterised by an improvement in the neurological condition in the majority of cases.