Complications of Circumcision: Epidemiological, Anatomo-Clinical and Therapeutic Aspects ()
1. Introduction
Mutilation imposed on oneself or others for religious reasons or to mark one’s membership of a community is an ancient practice that spares no region of the body [1] . Circumcision (peritomy, posthectomy), from the Latin circumcisio, “to cut around, to cut out”, refers, in its most widespread form, to the total or partial removal of the foreskin, leaving the glans exposed. It is a ritual practice imposed by Mosaic law for Israelites, a tradition for Muslims, a rite of passage to adulthood for many people of Africa and the East. Circumcision is also a widely used therapeutic surgical procedure for a number of balanopreputial affections [2] . Due to multiple reasons (religion, cultural or therapeutic), the prevalence of male circumcision varies by continents and is common in countries of North America, Australia, Africa, the Middle East, has interintercountry variations throughout Asia, and is uncommon in Europe and South America [3] . Risk of complications is about four per hundred circumcisions and higher risk of complications is determined by therapeutic circomcisions and aged 2 - 18 years at circumcision as compared to infants [4] . The aim of this study was to list the cases of circumcision complications received in urological hospitals, and to analyze their epidemiological, anatomo-clinical and therapeutic aspects.
2. Patients and Method
This was a retrospective, descriptive study of 33 patients presenting with complications of circumcision, collated at our center over a 5-year period (January 1, 2013 to December 31, 2017). We included any patient received for a circumcision complication during the study period. Patients with incomplete medical records were not included in the study. The different parameters studied were: age, consultation time, chief complain, types of complications, treatments carried out and therapeutic results. The data was collected from the consultation registers, recorded on Excel and processed by SPSS software.
3. Results
Thirty-three cases of circumcision complications were collected over a 5-year period. The mean age of the patients was 7.63 years (9 months - 16 years) (Figure 1). Time to consultation varied according to the type of complication, with an average of 1.6 years (1 day - 10 years). The chief complains were dominated by urine leakage from the ventral surface of the penis (18.2%) and swelling of the penis (15.1%). In anatomical terms, granuloma of the penis accounted for 36.3% of the complications (n = 12). It was followed by local infection (30.3%, n = 10) and urethro-cutaneous fistula (18.2%, n = 6) (Table 1). The treatment
![]()
Figure 1. Distribution according to age groups.
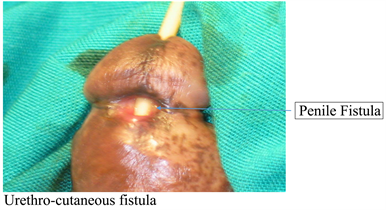
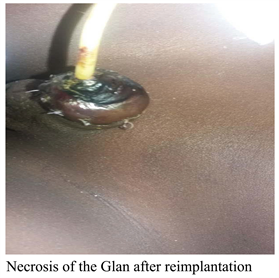
technique used depended on the nature of the lesion. Urethro-cutaneous splitting was performed in 5 patients with urethro-cutaneous fistula, while the same complication necessitated urethroplasty in another patient. We noted five cases of verge plasty for verge granuloma, one glan reimplantation and one glan plasty for the two patients with glans amputation. All patients underwent antibiotic prophylaxis after repair of the lesion. The eight cases of local infection were managed with antibiotic therapy and local care, while the one case of tetanus was treated specifically for tetanus with antibiotics, tetanus serum and tetanus vaccine.
Post-treatment follow-up was straightforward in all patients, with the exception of the two cases of glans amputation, which necrotized after re-implantation, necessitating a second stage penile plasty.
4. Discussion
The mean age of our patients was 7.6 years, with extremes of 9 months and 16 years. The various series reported show a similar age. SYLLA [5] and DIABATE [6] respectively report a mean age of 7.6 and 7.1 years, close to that found in our series. On the other hand, some authors report a different mean age from ours: RIMTEBAYE [7] (9.68 years), DIALLO [8] (14.9 years) and DIETH [9] (28 months, i.e. 2 years 4 months). This difference in age could be explained by the diversity of cultures and customs in African countries. In some countries, circumcision is performed in an early age, while in others it is performed in late age. In European countries, circumcision is performed in the neonatal period. The time taken for consultation varied widely, depending on the mentality of the population concerned and, above all, on the type of accident. In our series, the average consultation time was 1.6 years, with extremes of one day and 10 years. The latter was different from that of some authors [5] [7] [8] [10] . It was shorter for hemorrhage and glans rupture, and later for urethral fistula and penile granuloma. This delay in consultation could be explained by a lack of awareness of the subsequent consequences that could affect the boys’ aesthetic and sexual prognosis. In our series, urinary leakage from the ventral surface of the penis accounted for 18.18% of cases (n = 6), dysuria and hemorrhage for 3 cases each. Other signs were less frequent. These results are close to those of some authors [5] [7] [10] . Urinary leakage, a direct consequence of urethro-cutaneous fistula, was the lesion most frequently reported in the literature [8] [11] [12] . Granuloma of the penis was the most frequent lesion, accounting for 36.36% (n = 12). It was the lesion least frequently found in the literature, as reported by other authors. SYLLA [5] , over 11 years, found 2 cases of granuloma of the penis secondary to circumcision, SOW [13] (2 cases), BA [14] (5 cases), OZDEMIR [15] (3 cases), TLIL [16] (4 cases). It is due to a local reorganization of lymphatic drainage after circumcision [10] . This could be explained by the trivialization of the lesion by victims, who tend to hide it from their parents. Treatment of this lesion is based on excision of the pseudo-elephantiasis mass (penile plasty) and antibiotic therapy. Urethro-cutaneous fistula was the second most frequent lesion in our study, accounting for 18.18% (n = 6). Most authors agreed on the location of fistula in the balanoprepucial groove, where the urethra is more superficial. Variable mechanisms have been put forward to explain the occurrence of fistula. The most common mechanism is probably the capture of part of the urethral wall by a too-deep suture at the time of hemostasis of the brake artery [10] , resulting in secondary urethral necrosis, followed by fistulization. However, other penile anomalies, such as the mega urethra, have been incriminated in the occurrence of urethral fistula. Random or insufficient anatomical knowledge and non-compliance with anesthesia rules have also been implicated. We used the urethro-cutaneous splitting technique for fistula cure in 5 cases. Only one case of Davis urethrorrhaphy was performed. The first method was the one most used by many other authors: SOW [17] , RIMTEBAYE [5] , SYLLA [5] . Stenosis of the ureteral meatus occurs most often at a distance from circumcision and seems to be a direct consequence of the latter, as it is a pathology rarely found in uncircumcised patients [18] . There is fibro-sclerotic tissue around the urethral orifice. It is secondary to infection or trauma, sometimes minimal, of the urethral meatus, often unnoticed at the time of circumcision [10] . Meatoplasty was the method of cure used in our series, the technique of choice for other teams [5] [10] . Amputation of the glans penis is the most dramatic complication, since it jeopardizes aesthetic, urinary and sexual prognosis. In our series, we found two cases of total glans amputation, all secondary to circumcision performed by a paramedic. The consultation time was 5 hours for one of the cases, and the other was seen seven days later. However, the incidence of glans amputation is unknown. Its frequency is differently reported in the literature. MSEDDI et al. [19] reported eight cases of glans amputation following traditional circumcision in Tunisia, whereas in Côte d’Ivoire, Dieth et al. [9] collected four cases in fourteen years. Contributing factors cited were: the child’s flailing during foreskin sectioning, live circumcision (without anesthesia), and failure to follow the various stages of circumcision [10] . These consist in first decapping and cleaning the glans smegma, then incising the foreskin and its mucous membrane longitudinally and transversely 4 mm from the balanoprepucial groove along lines marked in advance with a felt-tip pen. Circumferential mucocutaneous suture is made with 5/0 absorbable thread. For ritual circumcision, particularly in our country, the foreskin and its mucous membrane are cut transversely at the same time, after good traction on the foreskin by the operating assistant. This section is performed after wedging and pushing down the glans between the thumb and forefinger, or at best, after placing a clamp over the glans previously located by the fingers [19] . Therapeutic management depended on how soon the patient was seen after the accident, and the conditions under which the severed glans was transported. In our series, balanic reimplantation was attempted in one case, but the therapeutic outcome was glansal necrosis. In the second case, a late-stage meatoplasty was performed for comfort. However, many authors recommend attempting balanic reimplantation regardless of the delay in management. DIABATE [20] et al. reported a case of successful glansal reimplantation of a patient admitted 15 minutes after amputation. ESSID [21] reported a case of amputation successfully reimplanted after a delay of 2 hours and a half. SYLLA [5] reported a case of failed reimplantation. SOW [10] had attempted four reimplantations, all of which failed. This therapeutic failure explains all the difficulties in managing glansal amputations involving microsurgery. This type of lesion can be avoided by correct traction on the foreskin, placing a clamp over the glans penis and wedging the thumb over the glans penis [21] . The frequency of post-circumcision infections is highly variable, and can be significantly elevated when circumcision is performed by inexperienced hands whose asepsis rules are often ignored. Infections may be local (localized suppuration) or general (sepsis), and may be life-threatening. In our series, ten cases of infection were recorded, including eight local infections and two cases of septicemia (tetanus) secondary to circumcision by a traditional practitioner and a community agent. One of the two cases of tetanus died in intensive care, while the other recovered. TAMBO [22] reported one case of suppuration in his series. SOUMARE et al. [23] reported 54 cases of tetanus in seven years. DIABATE [6] found 9 and 10 cases of infection respectively in two of his studies, including one case of necrotizing fasciitis. The frequency of these infectious complications can be explained by failure to observe basic asepsis rules and to master the circumcision technique. They were higher when circumcision was performed by a paramedic or traditional practitioner.
The limitations of this study are the retrospectivity and a smaller number of participants.
5. Conclusion
Circumcision is a medical procedure widely practiced throughout the world for cultural, health, religious or aesthetic reasons. The particularity in Africa, and specifically in Senegal, lies in its trivialization, carried out mainly by paramedical staff or traditional practitioners with mass circumcisions for cultural reasons. The serious complications encountered in our study, such as glans amputation, should encourage health authorities to provide a legal framework for this surgical procedure, and to facilitate its performance by qualified personnel.