Use of Trans-Vaginal Ultrasound to Diagnose and Treat Infertility and Its Performance ()
1. Introduction
When a clinical pregnancy cannot be established after 12 months of regular, unprotected sexual activity, it is said to be infertility. Between 8% and 12% of couples who are of reproductive age are thought to be affected globally. Males are shown to be the only ones at fault in 20% - 30% of infertility cases, yet they are involved in 50% of all instances [3] . The most prevalent type of female infertility worldwide is secondary infertility, which is frequently brought on by infections of the reproductive system (Tan & Robertson, 2011) [4] . Infertility is defined as the inability to conceive after one year of sexual activity without contraception. Male factor accounts for 20% to 30% of infertility cases, anovulation accounts for 10% to 30%, tubal factor accounts for 15%, cervical factor accounts for 5%, endometriosis accounts for 5% to 25%, and unexplained factors account for the remaining 15% to 30% [5] . However, the causes of infertility may change depending on where you live. Since the mid-1980s, high resolution transvaginal sonography (TVS) has been widely available and employed as an integral aspect of gynecologic sonographic examination, including infertility evaluation. A transvaginal ultrasound is a diagnostic imaging procedure that allows doctors to visualize the pelvic cavity and the organs inside the pelvis [6] . The cervix, uterus, fallopian tubes, and ovaries are among these organs. A transvaginal ultrasound can detect abnormal formations or growths in the pelvic area, which may be indicative of a disorder or disease [7] . Since the mid-1980s, high resolution transvaginal sonography (TVS) has been widely available and employed as an integral aspect of gynecologic sonographic examination, including infertility evaluation. Transvaginal Ultrasound (TVU) has emerged as a pivotal tool in the field of infertility diagnosis and treatment. Infertility, defined as the inability to conceive after a year of regular unprotected intercourse, affects millions of couples worldwide. With the advancement of medical technology, TVU has gained prominence due to its non-invasive nature and ability to provide high-resolution images of the female reproductive organs. This imaging technique enables clinicians to assess various anatomical and functional aspects of the reproductive system, aiding in the accurate diagnosis of underlying conditions that contribute to infertility. Furthermore, TVU plays a crucial role in guiding infertility treatments, such as assisted reproductive techniques and surgical interventions, by providing real-time visualization and monitoring.
A transvaginal ultrasound captures images of the pelvic cavity and organs using sound waves and projects them onto a screen. A transducer is a wand-like tool that is placed into the vagina and emits sound waves that bounce off the various tissues inside the pelvis [7] . The sound waves return to the transducer and are transformed into electrical signals. These signals display a real-time visual image of the pelvic organs on a screen in front of the technician performing the treatment. The ultrasound also captures still photographs of the graphics on the screen, which your clinician can examine later. The image created during an ultrasound is known as a “sonogram” [7] . In the diagnosis of infertility, transvaginal ultrasound is commonly used to assess the ovaries for the presence of follicles, which contain the eggs. Ultrasound can also detect abnormalities in the uterus or other structures that may be contributing to infertility. In addition to diagnosis, transvaginal ultrasound can also be used in the treatment of infertility. For example, it can be used to guide the placement of a catheter or other device for intrauterine insemination or in vitro fertilization. It can also be used to monitor the growth and development of follicles during fertility treatments.
2. Rationale of the Study
Transvaginal Ultrasound (TVU) plays a critical role in identifying specific features and abnormalities in the female reproductive organs that are closely associated with infertility. By providing detailed visualization of these structures and conditions, TVU contributes significantly to the accurate diagnosis of infertility-related issues, enabling targeted interventions and treatment strategies to improve the chances of successful conception and pregnancy. Transvaginal Ultrasound (TVU) is a powerful diagnostic tool that can identify various features and abnormalities in the female reproductive organs, shedding light on underlying causes of infertility [8] . The specific features and abnormalities was detected by TVU and it was associations with infertility. Some key features and abnormalities which were detected by TVU are given as follows:
Uterine fibroids: Uterine fibroids are noncancerous growths that develop in the wall of the uterus. TVU can identify the presence, size, and location of fibroids. Larger fibroids or those distorting the uterine cavity can hinder embryo implantation by altering the uterine environment or blocking the fallopian tubes’ entrance.
Ovarian Cysts: Ovarian cysts are fluid-filled sacs that form on the ovaries. TVU can detect cysts and assess their characteristics. Large cysts or polycystic ovaries, often associated with conditions like Polycystic Ovary Syndrome (PCOS), can disrupt ovulation and affect fertility.
Endometrial Polyps: Endometrial polyps are growths within the uterine lining. TVU can identify these polyps, which may interfere with embryo implantation by affecting the uterine environment. They can also cause irregular bleeding, impacting menstrual cycles.
Ovulatory Dysfunction: TVU can track the development of ovarian follicles and monitor ovulation. Anovulation (lack of ovulation) or irregular follicular development can result in irregular menstrual cycles and fertility issues.
Thin Endometrial Lining: TVU measures the thickness and characteristics of the endometrial lining. A thin or inadequate endometrial lining may not provide an optimal environment for embryo implantation and may lead to difficulty in achieving and maintaining pregnancy.
Anatomical Variations: TVU can identify anatomical variations such as septate or bicornuate uterus. These conditions can affect embryo implantation, pregnancy progression, and the risk of miscarriage.
Tubal Abnormalities: TVU can assess the patency of the fallopian tubes. Blocked or damaged tubes prevent the natural meeting of sperm and egg, hindering fertilization. They can also impede the transport of embryos to the uterus, leading to infertility.
Hydrosalpinx: Hydrosalpinx is a condition where the fallopian tubes are filled with fluid. TVU can detect this and understand its impact on fertility. Hydrosalpinx not only affects embryo transport but also creates a toxic environment within the tubes, reducing the chances of successful conception.
Ovarian Reserve Assessment: TVU assists in evaluating ovarian reserve by counting the number of antral follicles present in the ovaries. A reduced ovarian reserve indicates a lower potential for successful conception.
Corpus Luteum Assessment: TVU can visualize the corpus luteum, a temporary endocrine structure formed after ovulation. Absence of the corpus luteum suggests anovulation and decreased chances of pregnancy.
These features and abnormalities are associated with infertility due to their direct impact on the ability to conceive and maintain pregnancy. Transvaginal Ultrasound (TVU) enables clinicians to accurately diagnose these issues, facilitating targeted interventions and personalized treatment strategies to address the underlying causes of infertility and improve the likelihood of successful conception and pregnancy. The Study was designed to evaluate the patients by using TVU to diagnosis the accuracy of the causes of infertility and identify the standard treatment option for the patients who have the problem.
3. Research Objectives
3.1. Primary Objectives
The primary objective of this study is to investigate the multifaceted application of Transvaginal Ultrasound (TVU) in the assessment of infertility. The study aims to delve into the specific aspects of TVU’s application that contribute to the comprehensive evaluation of infertility-related issues.
3.2. Specific Objective
1) To explore how TVU assists in assessing the anatomical structures of the female reproductive system, such as the uterus, fallopian tubes, and ovaries. This involves investigating the ability of TVU to identify abnormalities, such as uterine fibroids, ovarian cysts, and anatomical variations that might hinder conception.
2) To investigate how TVU aids in evaluating ovulatory function by monitoring the growth and rupture of ovarian follicles. This objective encompasses the use of TVU to track the development of the dominant follicle and the release of the egg, which are crucial for successful fertilization.
3) To analyze how TVU assists in assessing the endometrial lining of the uterus, particularly its thickness and characteristics. The study aims to understand how TVU can help identify conditions like endometrial polyps or inadequate uterine lining, which can affect embryo implantation.
4) To examine the role of TVU in evaluating tubal patency, that is essential for the passage of sperm and fertilized eggs. The study aims to investigate the accuracy of TVU in detecting tubal blockages or abnormalities that may hinder the transport of gametes.
5) To assess how TVU guides infertility treatments, including intrauterine insemination (IUI) and in vitro fertilization (IVF). This involves understanding how TVU helps with follicular monitoring, embryo transfer guidance, and the detection of potential complications during treatment.
By addressing these specific aspects of TVU’s application in infertility assessment, this study aimed to provide a comprehensive understanding of the role of TVU in diagnosing and treating infertility. The purpose of this paper was to explain how to use vaginal sonography in the study of infertile women, including uterine evaluation. Endometrial receptivity, endometrial polyp, uterine myoma, adenomyosis, intrauterine adhesion, and morphological anomalies are all evaluated. Furthermore, the examination of ovaries and fertility problems such as polycystic ovarian syndrome and endometrioma will be explained. Furthermore, the ultrasonographic details of a pseudo cyst and a hydrosalpinx are presented.
4. Material & Methods
The study was a retrospective study. The study location was Combined Military Hospital (CMH), Cumilla, Bangladesh. The study was conducted from January, 2019 to July 2021. The Study is a cross sectional study and used purposive sampling methods through a series of screening. The study identified 45 medical records of women who underwent transvaginal ultrasounds as part of their infertility evaluation within the study time and treatment are reviewed. The ultrasound findings are compared to other diagnostic tests, such as blood tests and hysterosalpingography, and the outcomes of the fertility treatments were analyzed. Through the study, the performance of transvaginal ultrasound in diagnosing and treating infertility was evaluated based on several criteria, including:
Diagnostic accuracy: The ability of transvaginal ultrasound to accurately diagnose causes of infertility, such as polycystic ovary syndrome, endometriosis, or uterine abnormalities.
Predictive value: The ability of transvaginal ultrasound to predict the success of fertility treatments, such as in vitro fertilization (IVF) or intrauterine insemination (IUI).
Safety: The safety of transvaginal ultrasound procedures, including the risk of complications such as bleeding, infection, or damage to the reproductive structures.
Patient experience: The patient’s comfort and satisfaction with the transvaginal ultrasound procedure, including the level of pain or discomfort experienced during the exam.
Cost-effectiveness: The cost-effectiveness of using transvaginal ultrasound compared to other diagnostic tests or treatment options for infertility.
Inclusion criteria:
● Women of reproductive age who were referred to a fertility clinic for evaluation and treatment of infertility.
● Women who underwent transvaginal ultrasound as part of their fertility evaluation
● Women who received fertility treatments, such as IVF, IUI, or ovulation induction, based on their ultrasound findings.
Exclusion criteria:
● Women who did not undergo transvaginal ultrasound as part of their fertility evaluation
● Women who received fertility treatments that were not based on their ultrasound findings
● Women with medical conditions or disorders that could interfere with fertility, such as premature ovarian failure or cervical cancer.
● Women with incomplete medical records or missing ultrasound reports
The inclusion and exclusion criteria were carefully considered so that the study population ensures the correct representative of the Population and the study results were generalizable to the population of interest. Both primary and secondary infertility within 20 to 44 years of aged patients were selected for this study. Additionally, Informed consent form was filled up by the patients or their guardian and make them ensure that the ethical implications of using retrospective data had been be taken into account, including ensuring patient confidentiality and obtaining appropriate permissions for data access and use. Moreover, the study design was approved by the ethical review committee of the CMH.
Transvaginal Ultrasound Technique:
Transvaginal ultrasound is a diagnostic imaging technique that uses high-frequency sound waves to produce images of the female reproductive structures. The procedure is performed by inserting a small, wand-shaped transducer into the vagina, which emits sound waves and detects their echoes as they bounce off the reproductive structures [9] . During a TVU procedure, the patient lay down on an examination table, and a lubricated and covered ultrasound probe was gently inserted into the vagina. This probe emitted high-frequency sound waves that bounce off the internal structures, creating real-time images on a monitor. These images provided a clear view of the uterus, ovaries, fallopian tubes, and surrounding tissues. Here are the steps involved in a transvaginal ultrasound procedure:
● The patients were asked to remove clothing from the waist down and lie on an examination table with their feet in stirrups.
● The healthcare providers were inserted a small, lubricated transducer into the vagina, which is connected to an ultrasound machine.
● The transducers were moved around to obtain images of the uterus, ovaries, and other reproductive structures.
● The images were displayed on a monitor and can be analyzed by the healthcare provider to diagnose any potential causes of infertility.
● The procedure was typically taken 15 - 30 minutes to complete.
The procedure was more comfortable for the patient and some tips was taken like emptying the bladder before the exam, taking slow, deep breaths, and communicating any discomfort or pain to the healthcare provider. Overall, transvaginal ultrasound is a safe and noninvasive diagnostic tool that can provide valuable information on the reproductive structures and help to diagnose and treat infertility.
During the ultrasound exam, the Study physician evaluated the following structures for any abnormalities or conditions that may be causing infertility:
Uterus: The size and shape of the uterus was evaluated, and any abnormalities such as fibroids, polyps, or adhesions can be detected.
Endometrium: The thickness and texture of the endometrial lining was evaluated, which helped to diagnose conditions such as endometrial hyperplasia or polyps.
Ovaries: The size and number of follicles were assessed, which helped to determine the ovarian reserve and predict the response to fertility treatments.
Fallopian tubes: The patency of the fallopian tubes was also evaluated using saline-infused sonohysterography or hysterosalpingography, which helped to diagnose tubal occlusion or damage.
Cervix: The cervix was evaluated for any abnormalities, such as cervical stenosis or mucus plug.
In addition to diagnosing structural abnormalities, transvaginal ultrasound was used to monitor follicular development during fertility treatments such as ovulation induction, and to confirm pregnancy in the early stages.
5. Results
The Study used TVU methods to the 45 Female Patients by the researcher. The Patients who are coming at the CMH are study participants. Figure 1 Revealed that, 62 % (n = 28) of the patients were coming from urban area and 38% (n = 17) of the Patients were coming from Rural area.
At Table 1 stated that the age for the study participants was categorized into five groups starting from 20 years and up to 44 years. Based on the study participants, 35.6% (n = 16) were from 35 - 39 years of age, 26.7% (n = 12) were from 30 - 34 years, 15.6% (n = 7) were from 25 - 29 years of age and 13.3% (n = 46) were from 40 - 44 years of age and only 8.9% (n = 4) were from 20 - 24 years of age.
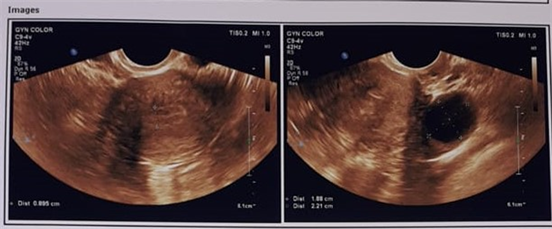
At Table 2 stated that Among the 45 patients 4 cases were found to have Leiomyoma which is 8.89 % of total cases, 5 cases having endometrioma which is 11.11%. 3 cases having 6.67 % had developmental abnormalities i.e. absent uterus, rudimentary uterus, ovarian agenesis, vaginal agenesis and short vagina. Normal findings of pelvis were found in 9 cases which is 20.00% of total cases. 7 cases had bulky uterus with PID. These groups are 15.56% of total study. 11 cases found to have PCOD, responsible for 24.44% of total number of cases, 2 cases found to have retroverted uterus which was 4.44%, 3 cases (6.67%) have adnexal Cyst, 1 cases (2.22%) found to have hydrosulphynx.
Table 3 stated that the study included 45 patients and the Comparison between clinical correlation and TVS findings were done in which 7 patients clinically
![]()
Table 1. Age Distribution with infertility.
![]()
Table 3. Comparison between clinical correlation and TVS findings.
seemed to have endometrioma with cyst formation which correlates 5 cases (71.43%) of TVS findings. The remaining 2 cases had normal findings by TVS examination. 5 cases of developmental anomaly had seemed clinically which corelates 3 cases (60%) of TVS findings. 9 of bulky uterus with PID found by clinical examination, but it was 7 cases (77.78%) clinically corelates by TVS findings. Leiomyoma was in 9 cases by clinical examination, which corelates 4 cases (44.44%) by TVS. The study found 13 cases of normal findings of pelvis but by TVS it was 9 cases. PCOD cases were 13 by clinical findings but by TVS examination it was 11.
At Table 4 stated that the volume of ovaries was measured according to a simplified workable formula as follows: Volume = Length × Breath × Thickness × 0.5. All the measurements were taken in centimeters and Volume expressed in milliliters. The average volume of the right ovary was found 15.98 ml where that of the left ovary found 14.99 ml.
In this study, Figure 2 depicted that the total number of developmental anomalies is 03 in which 02 cases of septed uterus is 67% of total study and 01 cases are due to ovarian and vaginal agenesis which is 33.33% of the study.
![]()
Table 4. Volume of ovaries in 11 polycystic ovaries.
![]()
Figure 2. Developmental anomalies of ovary, uterus and vagina.
Here out of total leiomyoma 01 cases were in subserous position which is 25% of total study. 02 cases in intramural situated and is of 50.00% of the total cases and submucous case is 01 which is 25% of the study (Figure 3).
Performance Evaluation of TVS:
Advantages of TVU in Infertility Assessment:
High Resolution Imaging: TVU provides high-resolution images of the pelvic organs, allowing clinicians to visualize fine details and subtle abnormalities that may not be easily detected by other imaging methods.
Non-Invasive: Unlike some other diagnostic procedures, TVU is non-invasive and generally well-tolerated by patients. It eliminates the need for surgical interventions or contrast agents, minimizing discomfort and risk.
Real-time Monitoring: TVU offers real-time imaging, enabling clinicians to observe the dynamic changes within the reproductive organs. This is particularly valuable for tracking the growth of ovarian follicles and monitoring the ovulation process.
Direct Visualization: The close proximity of the ultrasound probe to the pelvic organs in TVU results in clearer images compared to external ultrasound techniques. This direct visualization enhances the accuracy of diagnosis.
No Radiation Exposure: Unlike certain imaging methods, such as X-rays or CT scans, TVU does not involve ionizing radiation. This makes it a safer option, especially for women who are trying to conceive or are already pregnant.
Better Assessment of Ovarian Reserve: TVU aids in assessing ovarian reserve by visualizing the number and quality of follicles in the ovaries. This information is crucial in determining a woman’s fertility potential.
Follicular Monitoring: TVU is widely used in assisted reproductive technologies (ART) like in vitro fertilization (IVF) to monitor the development of follicles and determine the optimal timing for egg retrieval.
Guidance for Procedures: TVU provides real-time guidance during procedures such as intrauterine insemination (IUI) and embryo transfer. It helps clinicians accurately place the catheter or embryo into the uterus.
Tubal Assessment: TVU can detect abnormalities in the fallopian tubes, such as blockages or hydrosalpinx (fluid-filled tubes), which are significant factors in infertility.
In summary, Transvaginal Ultrasound (TVU) offers numerous advantages in infertility assessment due to its high-resolution imaging, non-invasiveness, real-time monitoring capabilities, and direct visualization of pelvic structures. These benefits make TVU an indispensable tool for diagnosing reproductive abnormalities and guiding infertility treatments, ultimately improving the chances of successful conception and pregnancy.
Endometrial Evaluation:
Transvaginal ultrasonography is a useful tool for evaluating the endometrium, which is the inner lining of the uterus. Some common findings on transvaginal ultrasound indicated abnormalities in the endometrium. It was observed that if an endometrial thickness was greater than 14 mm in premenopausal women or 5 mm in postmenopausal women might be indicative of an abnormality. Areas of increased echogenicity indicated the presence of fibroids, polyps, or other abnormalities [10] . Polyps are small, benign growths that can develop in the endometrium. They may appear as echogenic masses on ultrasound. Endometrial hyperplasia appeared as diffuse thickening or as focal areas of increased echogenicity. In some cases, TVS evaluated the endometrial pattern. The endometrial pattern is the appearance of the inner lining of the uterus, which can vary depending on the phase of the menstrual cycle or the presence of certain medical conditions. It’s important to note that the endometrial pattern seen on TVS should always be interpreted in the context of a patient’s medical history and symptoms. A healthcare provider can use the TVS findings to guide diagnosis and treatment decisions.
Leiomyomas: Transvaginal ultrasound (TVS) is a common imaging technique used to identify leiomyomas, which are also known as fibroids. Leiomyomas are benign tumors that develop in the muscular wall of the uterus. Here are some of the characteristics of leiomyomas that was identified on TVS like location, Size, Shape, Echogenicity, Margins, Blood flow etc. Leiomyomas are typically vascular and can be visualized using color Doppler imaging. Increased blood flow to the leiomyoma may indicate a more aggressive or rapidly growing tumor. It’s important to note that while TVS is a useful tool for identifying leiomyomas, a definitive diagnosis may require additional testing, such as MRI or biopsy. The study used the TVS findings to guide diagnosis and treatment decisions.
Developmental anomalies: Developmental anomalies are abnormalities that occur during fetal development and can affect the structure and function of the reproductive organs. Here are some of the developmental anomalies that can be identified through TVS like Uterine anomalies, Ovarian anomalies, Vaginal anomalies, Cervical anomalies, Tubal anomalies etc. Through using TVS, Developmental anomalies were identified; a definitive diagnosis might require additional testing, such as MRI or hysterosalpingography. It was imperative that physicians used the TVS findings to guide diagnosis and treatment decisions.
Bulky Uterus in PID: A bulky uterus can be a sign of pelvic inflammatory disease (PID), an infection of the reproductive organs that can cause inflammation and swelling in the uterus. Transvaginal ultrasound (TVS) was used to evaluate the size, thickness, fluid accumulation and shape of the uterus and to identify any signs of inflammation or infection.
Adnexal abnormalities: PID can cause inflammation and infection in the fallopian tubes, ovaries, or other adjacent structures. TVS can be used to identify any signs of adnexal abnormalities such as fluid-filled cysts or enlarged ovaries.
Overall, TVS can be a valuable tool in diagnosing and monitoring PID-related changes in the uterus and other reproductive organs. Treatment for PID typically involves antibiotics to clear the infection, and if there is a bulky uterus or other structural abnormalities, surgery may be necessary [11] . It is important to seek medical attention promptly if you suspect that you may have PID or any other reproductive health concerns.
6. Discussion
Leiomyoma, endometrioma, developmental anomalies, bulky uterus with PID, and PCOD, retroverted uterus, adnexal cysts, hydrosalpinx etc are all conditions that affected female reproductive health and potentially lead to infertility [12] . Here’s a brief overview of how each condition was related to infertility:
Leiomyoma: Also known as uterine fibroids, leiomyomas are benign growths that develop in the uterus. Depending on their size and location, they can interfere with fertility by affecting implantation or blocking the fallopian tubes. In our study, we have identified 8.89% of the patients have it and clinically 44.44% of them have correlated with TVS findings. A systematic review and meta-analysis of 25 studies found that uterine fibroids are associated with decreased fertility, with an odds ratio of 0.62 (95% CI, 0.49 - 0.78). The presence of submucosal fibroids was particularly associated with decreased pregnancy rates and increased miscarriage rates [13] .
Endometrioma: Endometriomas are ovarian cysts that develop when endometrial tissue grows outside of the uterus. They can interfere with fertility by affecting ovulation or implantation and can also cause pain and inflammation. In this study, 11.11% of the patients have endometrioma and have 71.43% have clinical corelations. Endometriomas, or cysts formed by endometriosis within the ovary, have been associated with decreased ovarian reserve and decreased fertility. One study found that women with endometriomas had lower pregnancy rates compared to women with other types of ovarian cysts, and that surgery to remove the endometriomas improved pregnancy rates [14] .
Developmental anomalies: Developmental anomalies are structural abnormalities that affect the female reproductive organs. Depending on the type and severity of the anomaly, they can interfere with fertility by affecting ovulation, implantation, or pregnancy. The study identified 6.67% of the patients with these anomalies and clinically 60% have correlated with infertility. Congenital abnormalities of the uterus, such as septate uterus or unicornuate uterus, have been associated with infertility and pregnancy complications. A retrospective study of 386 women found that women with congenital uterine anomalies had lower live birth rates and higher rates of preterm delivery and cesarean delivery compared to women with normal uterine anatomy [15] .
Bulky uterus with PID: Pelvic inflammatory disease (PID) is an infection of the reproductive organs that can cause inflammation and swelling in the uterus. A bulky uterus can be a sign of PID and may interfere with fertility by affecting implantation or causing scarring in the fallopian tubes. The Study identified 15.56% Bulky uterousw with PID which clinically 77.78% corelated with the infertility. Pelvic inflammatory disease (PID) can cause scarring and adhesions within the reproductive organs, potentially leading to infertility. One study found that women with PID were more likely to have uterine adhesions and a thicker endometrium on ultrasound, potentially indicating a higher risk for infertility [16] . Treatment involves antibiotics to clear the infection and may require surgery if there are structural abnormalities.
PCOD: Polycystic ovary syndrome (PCOS) is a hormonal disorder that can interfere with fertility by causing irregular ovulation or preventing ovulation altogether. It can also lead to other reproductive health issues such as endometrial thickening or insulin resistance. The study revelated that 24.44% of the patients had PCOD and have mostly 85.6% clinically corelated with the infertility. PCOS is a common hormonal disorder that can cause irregular periods, anovulation, and other reproductive issues. A meta-analysis of 35 studies found that women with PCOS had lower pregnancy rates and higher miscarriage rates compared to women without PCOS, and those treatments such as ovulation induction and in vitro fertilization may be helpful in achieving pregnancy [17] .
Retroverted uterus: A retroverted uterus is one that is tilted backward, toward the rectum, instead of forward. While this is a common variation in uterine position, in some cases it may be associated with infertility due to difficulty with sperm transport or implantation. The study identified 4.44% of the patients having retroverted uterus and 66.67% of them having clinically correlated with the infertility. A retroverted uterus, where the uterus is tilted backwards instead of forwards, is a common anatomical variation that is usually asymptomatic. However, some studies have suggested that a retroverted uterus may be associated with infertility. A systematic review and meta-analysis of 11 studies found that women with a retroverted uterus had a lower clinical pregnancy rate compared to women with a normally positioned uterus. However, the difference was not statistically significant after adjusting for confounding factors such as age and infertility duration [18] .
Adnexal cysts: Adnexal cysts are fluid-filled sacs that develop in the ovaries or fallopian tubes. While most adnexal cysts are benign and don’t interfere with fertility, larger cysts or those that affect ovulation or block the fallopian tubes can cause infertility. The study identified 6.67% of the patients having adnexal cysts and had clinically 60% had correlated with the infertility. Adnexal cysts, or cysts within the ovary or fallopian tube, are common and often asymptomatic. However, some types of cysts, such as endometriomas, may be associated with decreased ovarian reserve and infertility. A retrospective study of 109 women with endometriomas found that women with larger cysts and higher serum levels of CA-125, a tumor marker associated with endometriosis, had lower pregnancy rates compared to women with smaller cysts and lower CA-125 levels [16]
Hydrosalpinx: Hydrosalpinx is a condition in which the fallopian tubes become filled with fluid, typically due to a blockage or damage. This can interfere with fertility by preventing the egg and sperm from meeting or by affecting implantation. The study revealed 2.22% of the patients having hydrosalpinx and clinically 33.33% have corelated with infertility. Hydrosalpinx, or a fallopian tube that is blocked and filled with fluid, can be caused by pelvic inflammatory disease, endometriosis, or previous pelvic surgery. It is a known risk factor for infertility, as the blocked tube can prevent the egg and sperm from meeting. A meta-analysis of 22 studies found that the presence of hydrosalpinx was associated with a decreased clinical pregnancy rate after in vitro fertilization (IVF), with an odds ratio of 0.42 (95% CI, 0.32 - 0.54). Surgical removal of the affected tube or tubal occlusion may improve IVF outcomes in these cases [17]
Overall, these conditions can all potentially impact fertility and it’s important to seek medical attention if you have any concerns about your reproductive health. Treatment options vary depending on the specific condition and individual factors, so it’s important to work with a healthcare provider to determine the best approach for your needs. It’s important to note that not all women with these TVS findings will experience infertility, and not all cases of infertility will have these specific findings. TVS is just one tool used in the evaluation of infertility, and a full medical evaluation including a detailed history and physical exam, lab testing, and other imaging studies may be necessary to fully assess a woman’s fertility potential.
7. Recommendation
Transvaginal ultrasound (TVS) is a valuable tool in the evaluation of infertility, as it allows for the visualization of the uterus, ovaries, and fallopian tubes in a non-invasive manner [10] . Here are some recommendations for the evaluation of infertility by TVS and treatment options:
Initial evaluation: The initial evaluation of infertility by TVS may include a baseline ultrasound to assess the size and appearance of the uterus and ovaries, as well as to evaluate for any adnexal masses or cysts. A hysterosalpingogram (HSG) may also be recommended to evaluate the patency of the fallopian tubes. If endometriosis is suspected, a transvaginal ultrasound with color Doppler may be helpful in identifying endometriomas and other associated findings.
Treatment options: Treatment options for infertility may vary depending on the underlying cause and individual factors. In cases of ovulatory dysfunction, medications such as clomiphene citrate or letrozole may be used to induce ovulation. In cases of tubal factor infertility, surgical repair of the fallopian tubes or in vitro fertilization (IVF) may be recommended. In cases of endometriosis, medical management with hormonal therapy or surgical excision may be considered.
Follow-up imaging: Follow-up imaging with TVS may be recommended to monitor treatment response and identify any new or recurring abnormalities. In cases of IVF, ultrasound may be used to monitor follicle growth and to guide egg retrieval. After conception, TVS may be used to confirm the presence of a viable pregnancy and to monitor fetal growth.
It’s important to note that the evaluation and treatment of infertility is a complex and individualized process, and recommendations may vary based on a patient’s medical history and other factors. It’s important to consult with a healthcare provider for personalized evaluation and treatment recommendations.
8. Conclusion
In conclusion, transvaginal ultrasound (TVS) is a valuable tool in the evaluation and treatment of infertility. TVS allows for the non-invasive visualization of the uterus, ovaries, and fallopian tubes, which can help to identify structural abnormalities and other factors that may be contributing to infertility [19] . Additionally, TVS can be used to monitor treatment response and guide treatment decisions. Studies have demonstrated the high accuracy and reliability of TVS in diagnosing and monitoring infertility-related conditions such as leiomyomas, endometriomas, developmental anomalies, and adnexal cysts. TVS can also help to identify factors such as ovulatory dysfunction and tubal factor infertility, which can guide treatment decisions. In terms of treatment, TVS can be used to monitor response to ovulation induction medications, guide surgical interventions, and monitor IVF cycles. TVS can also be used during pregnancy to monitor fetal growth and development. Overall, the use of TVS in the evaluation and treatment of infertility can improve diagnostic accuracy, guide treatment decisions, and ultimately improve pregnancy outcomes. It is important to note that the evaluation and treatment of infertility is a complex process, and TVS should be used in conjunction with other diagnostic and treatment modalities for optimal care.
Acknowledgements
The authors would like to express their sincere gratitude to the authority of Combine Military Hospital (CMH), Cumilla Cantonment, for their valuable contributions to this research. The author is grateful for their guidance and expertise, which greatly enhanced the quality of this study. The author would like to thank patients and their caregivers for their assistance which was instrumental in the completion of this work. Furthermore, we extend our appreciation to Nondito Bangla Research & Development team for their support in data collection and analysis. Their assistance was crucial in obtaining accurate and reliable results.