Post-Operative Complications of Transvesical Prostatic Adenomectomy at Bouake Teaching Hospital: Epidemiological, Diagnostic and Therapeutic Aspects ()
1. Introduction
Benign prostatic hyperplasia (BPH) is the leading cause of bladder obstruction in men aged 50 and over. His treatment is twofold. The first is medical treatment, the effectiveness of which is indisputable. However, the second part, which is the curative treatment, is based on surgery. Trans-urethral resection of the prostate (TURP) represents the reference surgical technique when the technical platform is correct. In Bouaké, we still resort to open surgery due to the lack of endoscopic equipment. FREYER HRYNTCHACK’s transvesical approach is the most common technique in our department. It sometimes leads to complications that can be life-threatening. Few studies have been carried out in our work context in Côte d’Ivoire and particularly in Bouaké. This is how we decided to carry out this work, the general objective of which was to describe the morbidity and mortality linked to this surgical technique and their management at the Bouaké Teaching Hospital.
2. Material and Methods
This was a retrospective descriptive study, covering a period of five years from January 2016 to December 2022. This study took place in the Urology department of the Bouaké Teaching Hospital. It focused on the postoperative complications of trans-bladder prostatic adenomectomy. Included in our study were all patients operated on at the Teaching Hospital of Bouaké for BPH and who had postoperative complications or who were operated on and subsequently transferred to our department for complicated postoperative course. In total, over the study period, we collected 150 patients corresponding to the inclusion criteria and who had complete medical records. The parameters studied were age, postoperative complications, treatment, and mortality.
The results were analyzed by the logiciel Ep-info 2007.
3. Results
The average age was 67.2 ± 7.37 years with extremes of 54 and 84 years (Figure 1).
Immediate complications were dominated by postoperative hemorrhage of prostatic compartment in 7.33% of cases (Table 1).
Secondary complications were dominated by postoperative suppuration (Table 2).
Late complications were mainly represented by retrograde ejaculation in 73.33% of cases (Table 3).
Treatment of immediate and secondary complications (Table 4).
Concerning the late complication such as sclerosis of the prostate compartment, all our patients were treated endoscopically (Table 5).
All late complications such as urethral stricture were treated by endoscopic internal urethrotomy. Scrotomy a liquid reaction which was translucent in 76.08% of cases and squint in 23.90% of cases.
We observed 1.33% of deaths in the immediate postoperative period in our work.
![]()
Figure 1. Distribution of the 150 patients by age.
![]()
Table 1. Distribution of patients according to immediate follow-up.
![]()
Table 2. Distribution of patients according to secondary consequences.
![]()
Table 3. Distribution of patients according to late postoperative course.
![]()
Table 4. Management of immediate and secondary complications.
![]()
Table 5. Distribution of patients according to type of sclerosis treatment.
4. Discussion
In our study, the patients who presented postoperative complications after transvesical prostatic adenomectomy had an average age of 67 years plus or minus 7.37 years. This result can be superimposed on those of Kambou et al. in Burkina Faso [1] and Torésanni et al. in Benin [2] and Luhirirind et al. [3] which were respectively 68, 68.4 and 69.5 years. These results could be explained by age, but also by the presence of comorbidities.
Considered the main immediate complication of prostate surgery at a time when adenomectomy did not involve any haemostasis, postoperative haemorrhage currently seems to be better controlled [4] . Eleven patients or 7.33% presented postoperative hemorrhage in our study, this rate is slightly lower than that of Fourcade [5] and Guissé [6] who in their study found 9% and 11% respectively. Among the 11 patients, 5 presented with hemorrhagic shock during immediate postoperative monitoring. Their management was essentially done by blood transfusion, as in the study by Fourcade [5] and Ndemanga Kamoune et al. [7] . The 6 other patients had their hemorrhage subsided by administration of tranexamic acid and traction of the probe.
In our study, infectious complications constituted the major contingent of secondary complications encountered post-operatively with a rate of 81.33%. These infectious complications were dominated by parietal suppuration resulting in vesicocutaneous fistulas and orchiepididymitis. 72 patients or 48% presented parietal suppuration in our study, this rate is much higher than that of Guissé [6] who in his study was 21%. This excessive rate in our series could be explained by the presence of co-morbidity factors (diabetes) in some patients, by prolonged wearing of the urinary catheter preoperatively, as deplored by Fall et al. [8] in the Senegal, but also by the lack of asepsis during dressings. For these patients a cyto-bacteriological examination of the pus associated with an antibiotic therapy adapted to the antibiogram, as well as a daily dressing with Dakin were carried out, which allowed us to curb the infection.
According to Coulange [9] , vesicocutaneous fistula (VCF) is the specific complication of open adenomectomy using the Freyer Hrynstchak technique. In our study, 27 patients or 18% presented with VCF. This rate is slightly higher than that of GUEYE [10] which was 15% in his study. These vesicocutaneous fistulas encountered are the consequence of a release of thread linked to a local infection. The management was done by bladder drainage (catheterization of the fistula) associated with a daily dressing in twenty of them, i.e. 74.07%, until complete closure of the bladder, and a secondary suture was made in the other seven patients, i.e. 25.92%.
In our study, 23 patients presented with orchiepididymitis, i.e. 15.33%. In the study by Fourcade [5] , 3.4% was noted. Our result is superior to that of Fourcarde and this could be explained by the duration of wearing the preoperative urinary catheter as also deplored by other authors, such as Fall et al. [8] in Senegal, the reflux of urine infected in the vas deferens [11] . For these patients, antibiotic therapy adapted to the antibiogram associated with nonsteroidal anti-inflammatory drugs allowed us to overcome the infection.
In our study, we found transient urinary incontinence in 3.33% of our patients. It was urinary leakage occurring immediately after the removal of the catheter which improved after a few weeks. Anyanwu [12] reported a transient urinary incontinence rate of 7% with normalization of signs after about two months. We did not observe true urinary incontinence in our study. It could be explained by an anatomical impairment of the intrinsic part of the external sphincter which can be injured to a greater or lesser extent intraoperatively, responsible for an inability to maintain sufficient closing pressure in all circumstances to obtain a continence.
Retrograde ejaculation is the commonly accepted “almost constant” consequence of BPH surgery. It is linked to the disappearance of smooth muscle fibers and alpha adrenergic receptors from the bladder neck, which is necessarily severed during enucleation. This French Urological Association report in 1993 pointed out that the rate of retrograde ejaculation affects more than two out of three cases among patients who had sex before surgery [13] . In our study, 105 patients showed retrograde ejaculation, i.e. 70%. This rate can be superimposed on that of Conquy [14] .
5. Conclusion
Trans-bladder prostatic adenomectomy is a surgical technique for the management of BPH in our practice. It remains enamelled with several post-operative complications dominated by hemorrhage and infections. The control of haemostasis, the application of hygiene measures, rigorous asepsis associated with appropriate antibiotic therapy and the introduction of minimally invasive methods such as endoscopy, will considerably reduce the occurrence of these complications.
Ethical Committee Approval
The study was ethically approval from the local ethical committee of our University.
Annex
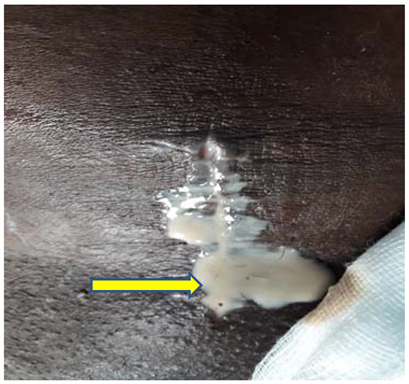
Picture 1. Suppuration of operating site.

Picture 2. Loosening of suture threads.

Picture 3. Loosening of suture threads.

Picture 4. Vesico-cutaneous fistula.