The Lebanese Society of Cardiology Consensus Statement on the Use of Natriuretic Peptides for the Management of Heart Failure ()
1. Aims
This consensus statement intends to create a clear diagnostic flowchart for diagnosing HF in both the acute and chronic setting in Lebanon.
2. Methods
This project was led by the members of the HF working group of the Lebanese Society of Cardiology and the Director of HF and biomarker trials at the Baim Institute for Clinical Research. The authors engaged in virtual meetings to define and agree on the aim and content of the consensus paper. Articles in English that provided relevant information and had a satisfactory publication date were reviewed. The authors presented their research and created an outline. The manuscript was then prepared according to the latest guidelines and approved by all authors after a thorough review.
3. Introduction
Plasma concentrations of Natriuretic Peptides (NPs) can be used as initial diagnostic tests for patients with symptoms suggestive of heart failure (HF). Elevated NP levels can help establish a working diagnosis of HF and guide further cardiac investigation. However, it is important to note that several conditions, including cardiovascular and non-cardiovascular causes such as atrial fibrillation, age, and renal failure, can impact the diagnostic accuracy of NPs. On the other hand, NP levels may be disproportionately low in obese patients [1] .
Heart failure (HF) is a condition that requires careful monitoring and treatment. An ideal biomarker for HF should have the following three characteristics: 1) low cost and quick measurement, 2) complementary information to clinical evaluation, and 3) ability to guide therapy.
In Lebanon, natriuretic peptides are not widely utilized due to their cost and the lack of knowledge among physicians on how to use them in an economically efficient manner. Furthermore, there are no established dosage and utilization protocols for these peptides in the country.
4. Background: Overview of Biomarkers in Heart Failure
Atrial natriuretic peptides (ANP) and B-Type natriuretic peptides (BNP) are activated in response to changes in heart volume and pressure and can reduce ventricular filling pressures by reducing cardiac preload and afterload [2] [3] . Pre-Pro-BNP (134 amino acids) is synthesized in cardiomyocytes and cleaved into Pro-BNP (108 amino acids) and then into N-terminal proBNP (1 - 76) and BNP (77 - 108) [4] .
BNP and NT-proBNP are both important markers for HF, but they have different properties. BNP is a 32-amino-acid polypeptide that has a half-life of around 20 minutes and is cleared from circulation by a receptor-mediated mechanism and neutral endopeptidases such as neprilysin. Its extraction requires an EDTA tube and waiting time to process the sample may result in a falsely low value. On the other hand, NT-proBNP is a hormonally inactive 76-amino-acid fragment that is passively eliminated by the kidneys and other organs with high blood flow with a longer half-life of around 1 - 2 hours. NT-proBNP is more stable than BNP in vivo and in vitro and less susceptible to circadian variation and repeated testing fluctuations. NT-proBNP levels are 8 - 10 times higher than BNP in HF due to its slower clearance and molecular weight [4] [5] . However, elevated NT-proBNP levels should be interpreted with caution in elderly patients with dyspnea and altered kidney function [6] .
5. How to Interpret Natriuretic Peptides Values
5.1. SomeConsiderations to Keep in Mind
1) Thresholds used to diagnose or rule out heart failure (HF) in both acute and chronic settings;
2) The influence of renal clearance and age on NP values;
3) Reasons for low NP values which are unexpected;
4) Causes of elevated NP concentrations which are unrelated to HF;
5) The impact of new treatments for HF and changes in HF demographics.
Over the years, many biomarkers have been developed for HF, but B-type natriuretic peptides (BNP/NT-proBNP) are the most commonly used for diagnosis, prognosis, treatment guidance, and therapy monitoring. They have been given a class I recommendation by the ACC guidelines [7] for diagnosis and prognosis in both acute and chronic HF, and a class I recommendation for risk stratification [8] . However, it is important to use these biomarkers wisely and with clinical expertise [9] [10] .
NP cutoff points vary based on the clinical presentation and type of NP measured. For example, in an outpatient setting for suspected heart failure, a BNP value of less than 35 pg/ml and an NT-proBNP value of less than 125 pg/ml would rule out heart failure. If BNP is greater than 35 pg/ml or NT-proBNP is 125 pg/ml or greater, heart failure should be suspected and confirmed through a cardiac ultrasound [1] [7] [11] .
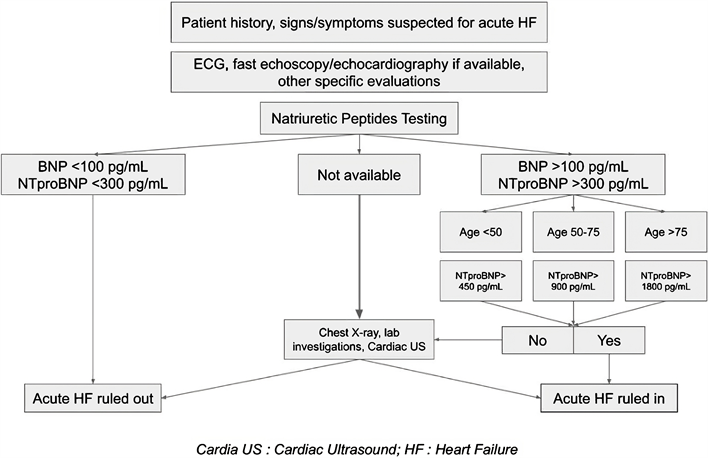
In acute HF, the negative predictive value of BNP and NT-proBNP is very high. A BNP concentration below 100 pg/mL and NT-proBNP below 300 pg/mL exclude acute HF with 99% negative predictive value.
To diagnose acute HF, the positive predictive value remains 75% - 80% for both BNP and NT-proBNP. When using BNP, values between 100 and 500 pg/mL are associated with increasing likelihood for acute HF. When using NT-proBNP age-adjusted cut-offs of 450/900/1800 pg/mL for ages < 50 years/50 - 75 years/>75 years are useful.
Understanding causes of elevated NT-proBNP outside of acute HF is important. Reasons for elevated NP concentrations that are not related to HF include acute coronary syndrome, pulmonary embolism/pulmonary hypertension, left ventricular hypertrophy, myocarditis, valvular heart disease, congenital heart disease, arrhythmias/cardioversion, and heart contusion/heart surgery [2] [12]
Reasons for unexpectedly low NP values include obesity, HF with preserved ejection fraction, mild acute HF, isolated right HF, partially treated HF, flash pulmonary edema, and constrictive pericarditis [13] [14] .
Treatments that may lower NP concentrations include diuretics, ACE inhibitors/ARBs, anti-aldosterone medications, cardiac resynchronization therapy, exercise, rate control for atrial fibrillation, and beta-blockers (after a rare temporary increase). The use of Sacubitril/valsartan can result in varying changes in NP concentrations [15] [16] [17] [18] .
5.2. Changes in Cut-off Values According to Comorbidities
1) Pulmonary Disease (COPD): The accuracy of NT-proBNP (NP) to diagnose heart failure (HF) is unchanged in the presence of preexisting pulmonary disease [1] [19] [20] .
2) Renal Dysfunction: The cut-off concentration is raised when the estimated glomerular filtration rate (eGFR) is less than 60 mL/min/m2. Age-specific cut-off points can be used for NT-proBNP, regardless of eGFR. The rule-out cut-off for BNP is 200 pg/mL. NP testing is discouraged in patients on dialysis [6] [12] [21] .
3) Diastolic Dysfunction: The BNP cut-off value of 100 pg/mL still has a sensitivity of 86% and a negative predictive value of 96%. BNP/NT-proBNP levels are unable to differentiate between heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF) [1] .
4) Atrial Arrhythmias (mainly atrial fibrillation): NP levels are higher with atrial fibrillation (AF) [4] No specific cut-off is recommended, however clinicians should be aware that both BNP and NT-proBNP are expected to be higher in the setting of atrial arrhythmia.
5) Patients Treated with Sacubitril/Valsartan: NT-proBNP is the recommended NP for diagnosis and monitoring of patients receiving treatment with sacubitril/valsartan [17] [18] .
7) Obesity (BMI ≥ 30 kg/m2): Lower NP levels are expected in the context of obesity. Interpret with caution and advise lower cut-off value by 50% when BNP is used [22] . Lower values are not advised with NT-proBNP.
8) Heart Failure due to Causes Upstream from the Left Ventricle (Mitral Stenosis or Acute Mitral Regurgitation): Low NP levels. Echocardiography is mandatory in cases of pericardial disease such as constriction or tamponade, as NP levels may be normal or near normal. NP concentrations may not help in these cases [8] .
9) Flash Pulmonary Edema: NP levels may be low, so rely on chest X-ray and physical examination [6] .
In light of all the various conditions that may affect NP levels, especially lowering their concentrations, it is important to know these conditions and to keep in mind that the clinical evaluation remains a cornerstone in the workup of a heart failure patient. As for conditions that elevate the cut-off concentration of NPs, the clinical exam is also of the utmost importance when facing for example a patient with atrial fibrillation and dialysis and elevated NPs.
5.3. NT-proBNP in Predicting Heart Failure
NT-proBNP strongly predicts the first onset of HF and is confirmed by a meta-analysis from 40 studies published before 2014 that included 95,617 individuals without a history of cardiovascular disease [23] . In patients with type 2 diabetes hospitalized for HF, a sharp increase in NT-proBNP levels was noted 6 months preceding hospitalization [24] .
NP should be evaluated as an essential test before echocardiography to avoid delay in diagnosis and reduce unnecessary tests. An NT-proBNP level of less than 125 pg/mL indicates that chronic HF is unlikely and further cardiac investigation is not needed [25] . At a NT-proBNP threshold of 125 pg/mL, 94% of patients who went on to have HF were identified.
In cases of acute HF, a plasma NP level should be measured in all patients with acute dyspnea upon presentation to the emergency department. An NT-proBNP level of less than 300 pg/mL makes the diagnosis of acute HF unlikely [25] . NT-proBNP acts as a gatekeeper to reduce resource wastage in cardiac ultrasound, in both chronic and acute settings.
BNP and NT-proBNP are both strong predictors of adverse cardiovascular events. They are also highly sensitive and specific for myocardial infarction. However, NT-proBNP might be a better diagnostic biomarker than BNP because it remains elevated for an average of 12 weeks [25] .
5.4. Natriuretic Peptides in Prognosis
The measurement of NT-proBNP levels on admission to the hospital can provide valuable information in determining the prognosis of patients with acutely decompensated heart failure (ADHF) [8] . In a study of 1256 patients with acute dyspnea and HF, elevated levels of NT-proBNP were strongly predictive of death within 76 days [26] . The optimal cut-off point for predicting one-year mortality was 986 pg/ml. A decrease of 30% in NT-proBNP levels from admission to discharge is also a strong predictor of improved outcomes [27] . The change in NT-proBNP levels is a significant predictor of subsequent events, regardless of treatment. The use of NPs as an initial diagnostic test can reduce the cost of healthcare by reducing the number of unnecessary cardiac echographies and identifying patients likely to require hospital admission. NT-proBNP has strong prognostic value in the outpatient setting, even in patients treated with sacubitril/valsartan (ARNI) [17] [18] .
All heart failure treatments, including ARNI, ACE inhibitors, angiotensin receptor blockers, beta blockers, aldosterone antagonists, and SGLT2 inhibitors, lead to a decrease in NT-proBNP levels and improved outcomes [28] ; clinicians should remember that ARNI treatment may lead to increase in BNP.
In patients with chronic HFrEF, NT-proBNP levels < 1000 pg/ml were associated with greater reverse left ventricular remodeling and improved clinical outcomes. A rise or fall of 25% - 30% in NP levels from one measurement to the next is necessary to determine a significant change has occurred [22] .
The majority of heart failure patients (acute or chronic) have elevated troponins, reflecting the progressive death of cardiomyocytes. The ACC/AHA guidelines strongly recommend a dosage of troponins on admission in order to stratify the risk of patients hospitalized for heart failure. On the contrary, ESC guidelines only recommend a dosage of troponins on admission of acute heart failure [28] . Galectin-3, a lectin expressed in heart failure, is a good predictor of re-hospitalization for heart failure within 1 to 4 months. However, it doesn’t appear to be a useful tool to diagnose acute heart failure. The dosage of Galectin-3 is recommended according to the ACC/AHA guidelines for prognostic stratification of patients with chronic heart failure. ESC guidelines however still do not recommend its use in clinical practice due to a lack of strong evidence [28] .
Natriuretic peptides remain the gold standard for the diagnosis of acute and chronic heart failure, and a dosage of troponins or galectin-3 can be added to stratify the risk of the patients.
5.5. The Role of NT-Pro BNP in Cardiovascular Disease Prevention for Diabetic Patients
The earliest recorded instance of diabetes dates back to the Egyptian physician Hesy-Ra around 3000 BC. Patients with prediabetes have a higher prevalence of hypertension, dyslipidemia, chronic kidney disease, and cardiovascular disease (CVD) risk. In 2015, 24% of diabetic patients and 88% of prediabetic patients were unaware of their condition [29] .
The overall prevalence of diabetes in heart failure is 20% - 25% [30] . Patients with diabetes have a two-fold risk of increased heart failure, hospitalization and death. The prevalence of heart failure in elderly diabetic patients is 39%. Diabetes patients make up 25% of all patients enrolled in large heart failure trials. Additionally, heart failure increases the risk of diabetes.
Individuals without CVD and with prediabetes may not necessarily be at elevated cardiovascular risk, but still warrant risk scoring for CVD like the general population.
A meta-analysis of data from 40 studies including 95,617 individuals without a history of CVD found that NT-proBNP strongly predicts first-onset heart failure and improves the prediction of coronary heart disease and stroke [31] . NT-proBNP was superior to HbA1c and albuminuria as a predictor of CV outcome and heart failure hospitalization in type 2 diabetes mellitus (T2DM) [24] .
The prognostic value of NT-proBNP in a cohort of patients with diabetes, including those with known CVD, showed that patients with low levels of NT-proBNP (<125 pg/mL) have an excellent short-term prognosis. The value of NT-proBNP in identifying patients with T2D who will benefit from intensified control of cardiovascular risk factors (CVRFs) was demonstrated in a small randomized controlled trial. NT-proBNP screening is gaining importance in T2D patients and is also increased in T2D patients with no overt heart disease [32] [33] .
5.6. Cost Effectiveness of Natriuretic Peptides in Diagnosis, Prognosis, and Prevention
Hospitalization is a critical issue for healthcare systems, as it accounts for approximately 70% of the total cost of heart failure (HF), whereas all drug treatments only account for 18% of the total costs [34] [35] . This is mainly due to the fact that a HF patient is typically hospitalized 2 to 3 times a year, with each stay lasting 5 to 7 days. In the coming years, a significant increase in HF hospitalization is expected, particularly in Lebanon due to the shortage and high cost of certain HF drugs, which will result in a significant impact on healthcare costs.
NT-proBNP testing in combination with clinical judgment was found to be a superior approach for the evaluation of acute dyspnea compared to clinical judgment alone. The use of NT-proBNP testing in the Emergency Department (ED) allows doctors to prioritize resources towards patients who need it most, resulting in improved outcomes and reduced costs from decreased hospitalization time and reduced advanced testing [10] [11] [12] [14] .
In Sweden, the use of NT-proBNP for HF diagnosis resulted in a potential yearly savings of ~?0 million for the healthcare system. This was achieved by using the NT-proBNP HF rule-out cut-off of 300 pg/mL in the Swedish algorithm for HF diagnosis [36] , which resulted in a 30% reduction in costs in the regions of Blekinge, Uppland, and Östergötland. Other countries are encouraged to create similar algorithms to estimate NT-proBNP savings for their healthcare systems.
In Lebanon, the cost of natriuretic peptides is high, but the savings are significant. Meetings with hospital administration to lower the cost of the test and reduce price variation between outpatient, ED, and in-hospital patients are necessary. Discussions with suppliers to provide support programs for patients without coverage to benefit from this test and reduce the need for other expensive medical exams are also important. Additionally, there is a need for a low-cost bedside kit for quick qualitative assay to help rule out heart failure in clinics and EDs, especially in remote areas where patients do not have access to all medical facilities.
6. Conclusion: Indication for NT-proBNP Testing: A Stepwise Approach
In clinical practice, physicians face several challenges, including how to quickly rule out heart failure diagnosis in patients presenting with acute dyspnea in the ED, how to rule out heart failure diagnosis in patients with chronic dyspnea in the outpatient setting, and how to reduce the cost of tests while searching for the cause of dyspnea. BNP and NT-proBNP have a high sensitivity when assessing heart failure. NT-proBNP cut-offs can be adjusted to the age of the patients whereas BNP dosages aren’t able to take age into consideration.
To simplify the decision-making process in these cases, we recommend using the age-independent rule-out cut-off limit of NT-proBNP (<300 pg/mL) and the age-dependent triple cut-point rule-in (>450 pg/mL for age < 50 years, >900 pg/mL for age > 50 years, and >1800 pg/mL for age > 75 years) based on the ICON and PRIDE trials for acute heart failure. For the chronic setting, a value of >125 pg/mL for NT-proBNP and 35 pg/mL for BNP were selected as the cut-off values to rule out heart failure. Both NPs have comparable diagnostic and prognostic accuracy.
Acute Heart Failure:
Chronic Heart failure:

Disclaimer:
The Lebanese Society of Cardiology Consensus Statement on the Use of Natriuretic Peptides for the Management of Heart Failure audited by an international expert from the USA was possible via a grant provided by Roche Lebanon SARL.