Compliance of Physicians with Standard Precautions of Handling Patients with Infectious Respiratory Disease ()
1. Introduction
Healthcare workers (HCWs) means any person working in health care facilities and has the risk of exposure to infectious materials like body fluids, contaminated medical equipment, contaminated environmental surfaces or contaminated air [1] .
Physicians are generally skilled workers who handle patients and technical equipment, performing related procedures and are exposed to different kinds of hazards [2] . Physicians work in the frontiers of the battles against any infectious diseases around the world including the emergence, spread, control and resolution of infectious outbreaks [3] . Due to the front-line nature of their work physicians are at increased risk of healthcare-associated infections (HAI) [4] . Physicians are at an occupational risk of developing infectious respiratory disease, and they can also spread these infections to other employees and patients. Even if a physician has no symptoms when attending work, they have the potential to transmit respiratory infections to both co-workers and other patients [5] .
Following the standard precautions (SPs) is the most effective and simple way to prevent infection. SPs are a set of recommendations outlined to prevent or minimize exposure to infectious agents by physicians, patients and their attendants [6] .
In 1985, the United States’ centers for disease control (CDC) introduced universal precautions (UPs) to protect HCWs from the spread of nosocomial infections. As a result, in 1996, CDC revised the infection control practice from Universal precautions to Standard precautions (SPs). Standard Precautions are the minimum practices to prevent infection that should be practiced on all patients regardless of suspected or confirmed infection status of the patient in all health care facilities. The components of SPs include hand hygiene, injection safety, use of personal protective equipment (PPE) and environmental cleanliness, as well as waste management, and respiratory hygiene and cough etiquette [6] . These practices are outlined to protect both the physicians and the patients from healthcare associated infections (HAIs) [7] .
Respiratory diseases are responsible for a huge global health burden (Forum of International Respiratory Societies, 2017). Respiratory infections are the main cause of acute infections in humans [8] .
Physicians can act as a mechanical vector for the spreading of HAIs from patient to patient [9] . On exposure, physicians can equally transmit nosocomial infections to their patients and may be the source of infection for their families and communities. Many studies suggest that there is increased probability of physicians being infected from both invasive and non-invasive procedures [4] .
Standard Precautions are applied for all patients at all times to prevent healthcare-associated transmission of infectious agents among patients and healthcare personnel [10] . Therefore, physicians should have proper knowledge and awareness about SPs and they should be always compliant to the standard precautions to control infection [11] .
Healthcare associated infections among physician’s leads to an increased rate of illness, absenteeism and even death amongst physicians. And it a burden for the health care system that comes at a large financial cost [8] . Therefore, the risk becomes high if physicians do not have awareness and compliance of SPs [11] .
Lack of awareness of infection control among HCWs has been recognized to hamper compliance with SPs. Therefore, strengthening SPs’ training for HCWs is recommended as a major means of promoting adherence to SP and protecting physicians as well as patients from nosocomial infections [7] .
In spite of the fact that HCWs are aware of infection control measures, often it is seen that compliance with these SPs are low among HCWs [4] . Lack of awareness about infection control practices among physicians is one of the leading causes responsible for low compliance to SPs [7] .
Measurement of the awareness of SPs among physicians is important because many studies show that compliance or noncompliance with SPs in a healthcare facility is related to the awareness of professionals [12] . This is an effective way to protect health professionals, patients and the public and to reduce hospital infections. Failure to comply may be reflected in high incidence rates of occupational accidents with exposure to bodily fluids and sharps.
Identifying the causes of lack of awareness about SPs and factors influencing non-compliance with SPs is important to design public health programs that offer pragmatic strategies to ensure the adherence of SPs across all health facilities for the protection of physicians as well as safety of the patients.
2. Materials and Methods
2.1. Study Design and Place
This was a cross-sectional questionnaire-based study was carried out to assess the level of compliance of physicians with standard precautions of handling patients with infectious respiratory disease. The study was carried out in two tertiary level hospitals named Rajshahi Medical College and Hospital, Rajshahi, Bangladesh and M Abdur Rahim Medical College and Hospital, Dinajpur, Bangladesh providing outdoor and indoor care to patients with infectious respiratory disease from 1st January 2020 to 31st December 2020.
2.2. Study Population
Physicians handling patients with infectious respiratory disease at M Abdur Rahim Medical College and Hospital, Dinajpur, Bangladesh and Rajshahi Medical College and hospital, Rajshahi, Bangladesh was considered as the study population.
2.3. Sampling
Purposive sampling technique was used for collection of data in my study. Samples were selected from study place after evaluating inclusion and exclusion criteria. Data was collected by conducted by face-to-face interview to the respondents. Only the willing participants were taken as sample.
Sample size was calculated using the following formula:
n = z2pq/d2
where, n = the desired sample size
z = At 95% confidence level usual value is 1.96
p = expected prevalence rate which was presumed 85%
i.e. 0.85 (Kotwal and Taneja, 2010)
q = = (1 − p) = 1 − 0.85 = 0.15
d = Absolute precision, 5% (0.05)
Since the largest calculated sample size was found to be 272, it was taken as the sample size for this study. To minimize non-respondents, after 10% increase in the size the desired sample size was 299.
Due to COVID-19 situation, a total of 17 days was allowed for data collection excluding weekends (Friday). After few days of initial data collection, it was observed that on an average 17 data could be collected per day. So the new sample size was calculated to be 17 × 17 = 285. The study was ultimately conducted on 285 respondents.
As number of target population in Rajshahi Medical College and Hospital, Rajshahi was higher than in M Abdur Rahim Medical College and Hospital, Dinajpur, 60% of the data were collected from Rajshahi Medical College and Hospital and 40% of the data were collected from M Abdur Rahim Medical College and Hospital. So out of 285 data 171 data were collected from Rajshahi Medical College and Hospital and 114 data were collected from M Abdur Rahim Medical College and Hospital.
2.4. Selection Criteria
Inclusion criteria
1) Physicians handling outdoor and indoor patients with infectious respiratory diseases.
2) Physicians who were willing to participate.
Exclusion criteria
1) Health care workers other than physician.
2.5. Data Collection Instrument
A semi structured questionnaire was developed in English. The questionnaire was developed using the selected variables according to the specific objectives. Questions were developed from review of qualitative and quantitative literature for relevant items [6] [7] [9] [14] [15] [16] including guidelines on standard precautions provided by the World Health Organization [17] and National guideline for health care provider on infection prevention and control of COVID-19 pandemic in healthcare setting [18] .
The questionnaire contained questions related to:
1) Socio-demographic characteristics of the respondents.
2) Assessment of awareness of physicians of standard precautions of handling patients with infectious respiratory disease.
3) Assessment of compliance of physicians with standard precautions of handling patients with infectious respiratory disease.
4) Assessment of reasons for non-compliance with standard precautions among physicians handling patients with infectious respiratory disease.
Awareness was assessed by a set of 25 questions. Compliance was assessed by a set of 30 questions using a five-point Likert’s scale. The final score for each section was classified into four categories: very poor (0% - 25%); poor (26% - 50%); moderate (51% - 75%); and good (76% - 100%) [14] .
The reasons for non-compliance were assessed by a set of 10 fixed options.
The questionnaire was pretested among respondents of similar characteristics. The questionnaire was then finalized after necessary modification according to the finding of pretesting.
2.6. Pre-Testing of Questionnaire
Before going to the process of data collection, pretesting was carried out on 10 physicians of similar characteristics to finalize the procedure and to evaluate the effectiveness of the research instrument. During pretesting participants were asked if any specific words or sentence they failed to understand as well as were any part of it was unacceptable or offensive word or had difficult expression. Participants were also asked about language difficulties or any alternatives fits better to their own language.
Pretesting was performed to identify the problem regarding the approach to ask the question and to evaluate the effectiveness of the research instruments and data collection tool. Then modifications were made as necessary and the research instrument was finalized. The average total time needed per respondents for data collection was 15 minutes.
2.7. Data Collection Technique
The data was collected by direct face to face interview of the respondents. The interview was conducted in M Abdur Rahim Medical College and Hospital, Dinajpur, Bangladesh and Rajshahi Medical College and Hospital, Rajshahi, Bangladesh providing outdoor and indoor care to patients with infectious respiratory diseases and privacy was maintained as far as possible. The data was collected by a prepared pre-tested questionnaire. Before preceding to the data collection, the detail of the study was explained properly to each respondent and written consents were taken from them. Assurance was given regarding confidentiality and secrecy of information they provided. Then the study participants were requested to answer the question according to developed format of questions. Collected data was checked, edited and verified at the end of the work in each day. Any inaccuracy and inconsistency were corrected in the next working day.
2.8. Ethical Consideration
The data was collected by direct face to face interview of the respondents. The interview was conducted in M Abdur Rahim Medical College and Hospital, Dinajpur, Bangladesh and Rajshahi Medical College and Hospital, Rajshahi, Bangladesh providing outdoor and indoor care to patients with infectious respiratory diseases and privacy was maintained as far as possible. The data was collected by a prepared pre-tested questionnaire. Before preceding to the data collection, the detail of the study was explained properly to each respondent and written consents were taken from them. Assurance was given regarding confidentiality and secrecy of information they provided. Then the study participants were requested to answer the question according to developed format of questions. Collected data was checked, edited and verified at the end of the work in each day. Any inaccuracy and inconsistency were corrected in the next working day.
2.9. Data Management and Analysis
At the end of each days of data collection, each questionnaire was checked to see whether it was filled completely and consistently or not. The data entry was started immediately after compilation of data collection. After the collection of whole range of data, they were processed and tabulated. Editing, coding and decoding of collected data were also done simultaneously, avoiding irrelevant and unreliable information. Data processing and analysis was done using IBM SPSS (Statistical Package for the Social Science) version 26. Data was analyzed according to the objectives of the study.
After completing data collection, the data was entered in SPSS version 26 software. Data clean-up was performed by running the frequency of each variable to check the accuracy, outliers, inconsistencies and missing value. The result was presented in tabulated form and charts. The distribution of age was categorized in five groups comprising of 25 - 31, 32 - 38, 39 - 45, 46 - 52 and 53 - 59 years. Gender was categorized into two groups male and female.
To assess or measure the objectives for descriptive statistics—frequency, percentage, mean, median, standard deviation (SD) was used for socio demographic factors such as age and gender.
The analysis of awareness and compliance related variables were done using descriptive methods (frequency, percentage).
Awareness was assessed by a set of 25 questions. 25 questions were divided into 7 sections, namely basics of standard precautions, awareness about respiratory hygiene and cough etiquette, awareness about personal protective equipment, awareness about hand hygiene, awareness about prevention of injuries and sharp instruments, awareness about disinfection of respiratory equipment, awareness about cleaning the patient-care environment.
In basics of standard precaution section there were 5 questions, in awareness about respiratory hygiene and cough etiquette section there were 2 questions, in awareness about personal protective equipment section there were 11 questions, in awareness about hand hygiene section there were 2 questions, in awareness about prevention of injuries and sharp instruments section there were 2 questions, in awareness about disinfection of respiratory equipment there was 1 question, in awareness about cleaning the patient-care environment section there were 2 questions.
Each question of awareness was coded by 1 for true or yes and 0 for false or no. Among 25 questions to assess awareness of standard precaution, 10 questions were negatively worded. So these 10 questions were re-coded as 0 for true or yes and 1 for false or no.
According to the response to these 25 questions by the participants, for each question every correct response was given 1 point and 0 was given for an incorrect answer. So, the total score of awareness of standard precautions of each participant ranged from 0 to 25.
Compliance was assessed by a set of 30 questions. 30 questions were divided into 6 sections namely hand hygiene, personal protective equipment’s, respiratory hygiene and cough etiquette, prevention of injuries from needles and other sharp instruments, cleaning and disinfection of respiratory equipment, cleaning the patient-care environment.
In hand hygiene section there were 7 questions, in personal protective equipment’s according to standard precaution section there were 5 questions, in respiratory hygiene and cough etiquette section there were 4 questions, in prevention of injuries from needles and other sharp instruments section there were 4 questions, in cleaning and disinfection of respiratory equipment section there were 5 questions, in cleaning the patient-care environment there were 5 questions.
Compliance was assessed using a five-point Likert’s scale with responses including “always”, “most of the time”, “sometimes”, “rarely” and “never”. Each questions of compliance were coded as 5 for always, 4 for most of the time, 3 for sometimes, 2 for rarely and 1 for never.
Among these 30 questions to assess compliance with standard precaution, 3 questions were negatively worded. So, these 3 questions were re-coded as 1 for always, 2 for most of the time, 3 for sometimes, 4 for rarely and 5 for never.
In the assessment of compliance 27 questions where positive responses were expected, scores of 5, 4, 3, 2 and 1 was given for any of always, most of the time, sometimes, rarely and never respectively. On the other hand, in 3 questions where negative responses were expected, scores of 5, 4, 3, 2 and 1 were given for never, rarely, sometimes, most of the time and always respectively. So, according to the response to these 30 questions by the participants, the total score of compliance with standard precautions of each participant were calculated and the score ranged from 30 to 150.
To calculate the percentage of the score of participant’s responses in awareness section and in compliance section, the total obtained scores from each section were divided by the maximum attainable scores in each section (25 and 150 for awareness and compliance, respectively) and then multiplication by 100.
The percentage of final score for each section (awareness and compliance) was classified into four categories.
Table showing classification of awareness and compliance with standard precautions of the participants according to the percentage of score obtained [14] :
To calculate the compliance of respondents with different components of standard precautions, obtained score in each section were divided by number of total questions in that section. After this calculation the obtained final score of each section was classified into five categories.
Table showing compliance of standard precautions into five categories:
A score of 1 was categorized as very poor, score of 2 was categorized as poor, score of 3 was categorized as moderate, score of 4 was categorized as good and finally a score of 5 was categorized as very good.
The reasons for non-compliance were assessed by a set of 10 fixed options. The responses for each option were added and percentage of response by the participants for each of the option regarding the reasons of non-compliance was calculated.
To assess the association between awareness of standard precautions and compliance with standard precautions was done using ANOVA test.
To assess the association between training on infection control and awareness of and compliance with standard precautions was done using independent T test.
A “p” value of less the 0.05 was considered significant.
3. Results
This cross-sectional study was conducted to see the compliance of physicians with standard precautions of handling patients with infectious respiratory disease. Total population of the study was 285 which were selected purposively according to inclusion criteria. Data were cleaned, edited, analyzed using SPSS version 26.
The results are organized into following sections:
1) Socio-demographic characteristics of physicians.
2) Awareness of physicians with standard precautions of handling patients with infectious respiratory diseases.
3) Compliance of physicians with standard precautions of handling patients with infectious respiratory disease.
4) Reasons for non-compliance with standard precautions among physicians of handling patients with infectious respiratory disease.
3.1. Socio-Demographic Characteristics
The distribution of the respondents according to their age category shows the younger one was 25 years old while the older one was 59 years old. Mean was 36.42 ± 10.37 years. Most of the respondents (40.7%) belong to the age group of 25 - 31 years of age whereas 25.3% respondents were in 32 - 38 years age group. 11.2% were in 53 - 59 years age group (Table 1).
![]()
Table 1. Distribution of respondents by age group.
Maximum: 59; Minimum: 25; Mean ± SD: 36.42 ± 10.373.
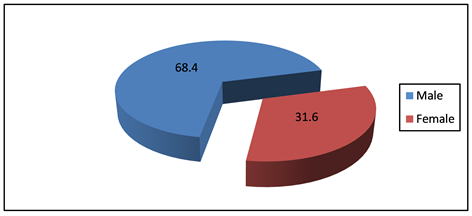
Above figure shows the distribution of respondents according to their gender. Among 285 respondents, most of them (68.4%) were male and rest of them (31.6%) was female.
3.2. Awareness of Physician with Standard Precautions
31.9% of the respondents were not aware of the fact that standard precaution should be performed on all patients. Nearly 60.7% of the respondents were not aware that medical mask provides protection from fine aerosol which is kept suspended in the air. 71.6% of the respondents were not aware that during use of double gloves big one should be worn first then the small one. Maximum respondents were not aware of the sequence of wearing and removing the different components of PPE. Maximum respondents that are 81.8% and 76.8% were not aware that needle should be never recapped and needle should be never bent respectively (Table 2).
Most of the respondents (78.6%) have moderate awareness about standard precautions whereas only 13.3% of the respondents have good awareness about standard precautions and 8.1% of the respondents have poor awareness about standard precautions (Table 3).
3.3. Compliance of Physicians with Standard Precautions
The compliance of hand hygiene among physicians among 285 respondents, 28.4% of the respondent sometimes performed hand hygiene immediately on arriving at work and also 31.6% performed hand hygiene sometimes before direct contact with patient. 43.9% of the respondent always performed hand hygiene after contract with patients. Most of the respondent had a good compliance about hand hygiene before putting on gloves for performing any invasive procedure (Table 4).
Most of the respondent 37.5% rarely and 16.8% never choose the right PPE before exposure to an infectious disease patient. 12.3% respondents never and 24.6% rarely changed their gloves between patients care and any procedure of another patient. 24% always and 31.6% sometimes wore plastic gown or fluid resistant gown during procedures which may result in splashes onto body. 37.5% respondents sometimes removed all PPE as soon as possible after completing the health-care procedure (Table 5).
79.3% respondents always cover nose and mouth during coughing and sneezing and 49.8% respondents always used upper arm in case of sudden episode of coughing or sneezing. 33% respondents always and 46.7% respondents most of the time performed hand hygiene after coughing and sneezing (Table 6).
Majority of the respondent have very poor compliance about using needles and sharps. 68.8% of the respondent always recapped used needles and 53% always break, bend, and removed needles by hand. 22.5% of the respondents always and 15.8% never disposed syringes, needles, scalpel blades and other sharp items in appropriate puncture resistance container (red container) (Table 7).
![]()
Table 2. Assessment of awareness of the respondents about standard precautions.
![]()
Table 3. Distribution of the respondents according to awareness of standard precautions of handling patients with infectious respiratory disease.
![]()
Table 4. Respondents compliance with hand hygiene.
![]()
Table 5. Respondents compliance with personal protective equipment.
![]()
Table 6. Respondents compliance with respiratory hygiene and cough etiquette.
![]()
Table 7. Respondents compliance with prevention of injuries from needles and other sharp instruments.
The compliance of respondents with cleaning and disinfection of respiratory equipment among 285 respondents, only 27% of the respondent sometimes clean and disinfect respiratory equipment between uses and 54% of the respondent never uses PPE while cleaning and disinfection of respiratory equipment. 41.4% of the respondent rarely keep clean and disinfected items dry and in individual packages (Table 8).
Majority (53%) of the respondent always decontaminate cloths or dresses used by physicians by washing or autoclaving but 35.1% of the respondent sometimes clean the environment used by the patient. 25.6% of the physician rarely clean or disinfect examination table used by the patient. 35.1% sometimes used techniques to avoid aerosolization of dust (Table 9).
![]()
Table 8. Respondents compliance with cleaning and disinfection of respiratory equipment.
![]()
Table 9. Respondents compliance with cleaning the patient-care environment.
The distribution of compliance of the respondents with the different components of standard precautions shows most of the respondents have moderate compliance with most of the components of standard precautions. Only in case of respiratory hygiene and cough etiquette 58.9% of the respondents have very good compliance and 37.2% of the respondents have good compliance. In case of personal protective equipment 27% of the respondents have poor compliance (Table 10).
76.5% of the respondents have moderate compliance with standard precaution and only 23.5% of the respondents have good compliance with standard precautions (Table 11).
Respondents having poor awareness of standard precaution have a mean compliance score of 93.91, respondents having moderate awareness of standard precaution have a mean compliance score of 106.04 and respondents having good awareness of standard precaution have a mean compliance score of 106.82. The compliance score for each category of awareness was significantly different from one another (p < 0.05) (Table 12).
Compliance with standard precautions of physicians having poor awareness of standard precautions is statistically significantly different from the physicians having moderate and good awareness of standard precautions. But there is no statistically significant difference of compliance with standard precautions between physicians having moderate and good awareness of standard precautions (Table 13).
3.4. Non-Compliance of Physicians with Standard Precautions
Maximum (86.7%) respondents consider lack of adequate facilities and resources was the main reason of non-compliance with standard precaution. Excess workload (76.1%), lack of training of infection control (63.2%) and time constrain (43.2%) were the other three main reasons that were considered by the respondents as reason for non-compliance with standard precautions. 49.1% of the respondents stated that PPE were not comfortable to use is another reason of non-compliance. But only 6.7% respondents consider that use of PPE may offend the patients (Table 14).
![]()
Table 10. Distribution of the respondents on their compliance of standard precautions of handling patients with infectious respiratory disease.
![]()
Table 11. Distribution of the respondents on their compliance of standard precautions of handling patients with infectious respiratory disease.
![]()
Table 12. Standard precautions compliance score with the level of awareness of physicians handling patients with infectious respiratory disease.
![]()
Table 13. Statistical analysis (level of significance) of inter group variation of compliance with standard precautions of physician having different level of awareness of standard precautions.
![]()
Table 14. Distribution of respondent’s reason for non-compliance with standard precautions of handling patients with infectious respiratory disease.
4. Discussion
Physicians are usually exposed to various occupational hazards in healthcare setting, especially biological because they are directly in contact with patients or body fluids. The common occupational risk in a hospital setting is contracting any infection. Particularly, exposure to body fluids containing infectious agents has long been recognized as a potential threat to physicians. Among the hospital acquired infections respiratory infection is one of the most common as during history taking, examination of the patients and performing any procedures physicians come in very close contact of the patients. While performing such task physician have a high risk of exposure to the respiratory secretions and droplets produced by patient while taking, coughing or during some medical procedures. Then physicians can further spread these infections from patients to patients as physicians can act as a mechanical vector for the spreading of infectious respiratory diseases. They can also spread these infections to other employees and patients and also have potential risk of transmission of respiratory infection to both co-workers and patients, even when having no symptoms while attending work. To reduce such risk for both physicians and patients, authorities like WHO and CDC have strict guidelines. These guidelines are commonly known as standard precautions. Proper awareness of these standard precautions and strict compliance with them can protect both physicians and patients from the risk of hospital acquired infections specially the respiratory infections which can spread very easily without the knowledge of any one. It is often times seen that physician are not completely and correctly aware of these standard precautions and it is also seen that despite being aware of the standard precautions physicians are not compliant with these standard precautions.
This study was intended to assess the compliance with the standard precautions of the physicians handling patients with infectious respiratory diseases. This cross-sectional study was conducted among 285 physicians handling patients with infectious respiratory disease at M Abdur Rahim Medical College and Hospital, Dinajpur, Bangladesh and Rajshahi Medical College and Hospital, Rajshahi, Bangladesh.
In the present study, the mean age of the respondents was 36.42 ± 10.373 years and age ranged from 25 - 59 years. The major portion of the respondents 40.7% belong to the age group 25 - 31 years of age whereas 25.3% respondents were in 32 - 38 years’ age group. Among the respondents 68.4% were male and 31.6% were female.
Several studies have described about the importance of standard precautions for HCWs mainly physicians of handling patients with infectious disease. Arinze-Onyia, et al. (2018) [7] mentioned in their study that the mean age was 37.20 years and age range was 20 - 59 years which was more or less similar to this present study. According to the study of Honarbakhsh, Jahangiri and Ghaem (2018) [14] , the mean age of the respondents was 31.63 ± 8.27 years. Another cross-sectional study conducted by Yazie, Sharew and Abebe (2019) [9] , mentioned that the age ranges of the HCWs was from 23 - 59 years. In the present study, the age range was 25 - 59 years because maximum physicians completed their MBBS degree in 24 years of age and usually retires at age 59 years.
Arinze-Onyia, et al. (2018) [7] examined the knowledge and practice of standard precautions among health care workers by conducting a descriptive cross-sectional study which was done in October 2014 at University of Nigeria teaching hospital, observed that 73% of the respondents in their study were female. Arinze-Onyia, et al. (2018) [7] and Honarbakhsh, Jahangiri and Ghaem (2018) [14] also observed that majority of the respondents in their study were female. But in this current study only 31.6% were female and rest of them (68.4%) were male. It may be due to the fact that the present study only included physicians but in Arinze-Onyia, et al. (2018) [7] study, among 629 participants, 290 participants were nurses and also in Honarbakhsh, Jahangiri and Ghaem (2018) [14] study nurses were predominant. As nurses were not included in this study could be the reason behind the disparity of gender distribution among this study and the other two studies stated here.
Awareness of standard precautions is very much important to be compliant with the standard precautions. Despite the SPs guideline, awareness varied among physicians.
In the present study overall awareness of the respondents regarding respiratory hygiene and cough etiquette and hand hygiene was good but 71.9% of the respondents didn’t know when to use the alcohol-based hand products. Majority of the respondents were not aware about personal protective equipment. Nearly 60.7% of the respondents were not aware that medical mask provides protection from fine aerosol which is kept suspended in the air, but 70.2% of the respondents were aware about when to use of particulate respirator instead of medical mask. Majority (71.6%) of the respondents were not aware about the procedure of using double gloves. Maximum participants were not aware of the sequence of wearing and removing the different components of PPE. But in current COVID-19 situation, it’s really a burning issue, because if the physicians are not aware of the sequence of wearing and removing different components of PPE, then the infectious respiratory disease will transmit to the physicians and then from physicians to the other patients. Majority of the respondents that is 81.8% were not aware that needle should be never recapped and 76.8% of the participants did not know that needle should be never bent. Although overall awareness about disinfection of respiratory equipment and cleaning the patients care environment was 69.5%.
In another cross-sectional study conducted by Akagbo, Nortey and Ackumey (2017) [19] among HCWs on standard precautions, only 39% of the respondents knew about respiratory hygiene and cough etiquette which is lower than the present study. Arinze-Onyia, et al. (2018) [7] and Ndu and Arinze-Onyia (2017) [15] study results about awareness of respiratory hygiene are also lower than the present study. The reason behind the increased awareness about the respiratory hygiene and cough etiquette among the participants of the current study could be due the fact that in this current COVID-19 pandemic situation the physicians are now more aware about this matter. But the awareness about prevention of injuries and other sharp instruments and also the awareness about how to discard sharps are very low compared to other study. In Ogoina, et al. (2015) [6] study more than half of the respondents didn’t know that sharp should never be recapped but very few only 12% didn’t know that, it was wrong to bend or break sharps or needles. Another study also revealed that 25% of the respondents didn’t recapped needles after use (Akagbo, Nortey and Ackumey, 2017) [19] . Compared with the present study, these study results are much better than present study; this could be due to the fact that none of the institutes where the current study was conducted had the facility of electric needle destroying machines in all working areas.
Compliance with hand hygiene after patient contact is one of the most important components of standard precaution. In the current study we found that 28.4% of the respondents sometimes performed hand hygiene immediately on arrival at workplace and 31.6% of the respondents performed hand hygiene before direct contact with patients, whereas 43.9% of the respondents always perform hand hygiene after contact with patients. 52.3% of the respondents always performed hand hygiene after contact with blood or body fluids or secretions. But surprisingly, only 36.5% of the respondents performed hand hygiene sometimes, 11.9% rarely performed hand hygiene after touching the patient’s surrounding environments which is more contagious for spreading infectious respiratory disease. 57.5% of the physicians had moderate level of compliance with hand hygiene which is not satisfactory during COVID-19 pandemic situation. The reasons may be the high workload, rigors of hand washing in between handling patients is considered burdensome and also may be lack of training on infection control.
Punia, Nair and Shetty (2014) [16] undertook a cross sectional questionnaire-based study among 162 HCWs in which 109 were doctors. Among them 95% of the respondents claimed to use hand rub after touching patients surrounding. 28% of the respondents in Ogoina, et al. (2015) [6] study practice hand hygiene after touching patient’s surroundings. But in the present study only 26.7% respondents perform hand hygiene after touching patient’s surroundings which is very low and not satisfactory during COVID-19 pandemic situation.
Ather, Khan and Shabnum (2020) [11] conducted a descriptive cross-sectional study which included 180 participants which also included physicians from Bahria International Hospital Lahore, Pakistan to assess knowledge and practice of health care workers regarding standard precautions. Ather, Khan and Shabnum (2020) [11] study revealed that 28.9% of the participants always washed their hands before and after patients care, 35.6% sometimes, which is more or less similar with the present study but the percentage of hand hygiene after touching the patient was higher (43.9%) in the present study. According to Ogoina, et al. (2015) [6] and Akagbo, Nortey and Ackumey (2017) [19] study, percentage of participants performing hand hygiene before touching any patients was 58.5% and 55% respectively which is higher than the present study. In Arinze-Onyia, et al. (2018) [7] study 52.1% of the respondents performed hand hygiene after contact with blood, body fluid or secretion which is more or less similar with the present study.
In the current study 37.5% respondents rarely and 16.8% never choose the right PPE before exposure to an infectious disease patient. But in Akagbo, Nortey and Ackumey (2017) [19] and Arinze-Onyia, et al. (2018) [7] study 61% and 53.4% of the participants wore the basic protective equipment respectively, which is very low in this present study. In the present study 12.3% respondents never changed their gloves between patients care and any procedure of another patient, only 23.2% always changed gloves which were very much lower than the Yazie, Sharew and Abebe (2019) [9] study. According to Yazie, Sharew and Abebe (2019) [9] study 64.5% and 88.7% of the participants changed gloves between patients care and during invasive procedure respectively. In Punia, Nair and Shetty (2014) [16] study 28.4% of the participants used protective gowns in case of risk of fluid splash. The present study revealed that 24% of the participants always wore plastic gown in case where there was risk of fluid splashes which is more or less similar to the findings of Punia, Nair and Shetty (2014) [16] study. In the present study 37.5% of the respondents sometimes removed all PPE as soon as possible after completing the health-care procedure which is more important for not spreading infection diseases through contaminated PPE. 48.8% of the physicians had moderate level of compliance with using PPE which is again not satisfactory in the current COVID-19 situation. The reason behind this finding could be due to the fact that most of the participants did not have any training on infection control. Arinze-Onyia, et al. (2018) [7] study revealed that those who were trained on SPs and PPE were significantly more likely to always use PPEs.
In the present study 79.3% respondents always covered their nose and mouth during coughing and sneezing and 49.8% respondents always used their upper arm in case of sudden episode of coughing or sneezing. 33% respondents always and 46.7% respondents most of the time performed hand hygiene after coughing and sneezing. 58.9% of the physicians had very good compliance with respiratory hygiene and cough etiquette. The reason behind the increased compliance with respiratory hygiene and cough etiquette among the physicians of the current study could be due the fact that in this current COVID-19 pandemic situation the physicians are now more aware about this matter.
Kotwal and Taneja (2010) [13] study evaluated the universal precautions perceptions on compliance and non-compliance of 96 participants, out of them 50 were doctors through a cross sectional study. According to Kotwal and Taneja (2010) [13] study 60% doctors admitted that they never recapped needles and 90% always disposed used needles in proper way. In Punia, Nair and Shetty (2014) [16] study 72.4% of the participants always recapped needle and in Fadeyi, et al. (2011) [1] study 56.9% of the participants recapped needle and 92.3% of the participants discarded needles and sharps in safety box. But in the present study majority (68.8%) of the respondent always recapped used needles which should never be done according to standard precaution protocol whereas only 13% never recapped and 22.5% of the respondents always and 15.8% never disposed syringes, needles, scalpel blades and other sharp items in appropriate puncture resistance container (red container).
In Punia, Nair and Shetty (2014) [16] study only 12.8% of the participants broke or bended needles by hand whereas in the present study 53% of the respondents always broke, bended and removed needles by their hand which is much higher than the findings of Punia, Nair and Shetty (2014) [16] study. Compared with the present study, the study results of Punia, Nair and Shetty (2014) [16] study are much better. This could be due to the fact that none of the institutes where the current study was conducted had the facility of electric needle destroying machines in all working areas. 60.7% of the physicians had moderate level of compliance with prevention of injuries from sharps and needles but 18.2% of the physicians had poor compliance which in regard to physicians is much higher.
In the current study, among 285 respondents only 27% of them sometimes cleaned and disinfected respiratory equipment between uses and 54% of the respondents never used PPE while cleaning and disinfection of respiratory equipment. 41.4% of the respondent rarely kept cleaned and disinfected items dry and in individual packages. 56.1% of the physicians had moderate level of compliance with regard to cleaning and disinfection of respiratory equipment.
In the present study, majority (53%) of the respondent always decontaminated cloths or dresses used by physicians by washing or autoclaving. Yazie, Sharew and Abebe (2019) [9] conducted a cross sectional in which 48.9% of the respondents always cleaned working environment at the end work. But in the present study 35.1% of the respondent sometimes cleaned the environment used by the patient and 25.6% of the physician rarely cleaned or disinfected examination table used by the patient which is much lower than the previous study. In present study 35.1% of the participants sometimes used techniques to avoid aerosolization of dust. 39.3% of the participants had moderate level of compliance with cleaning patient-care environment in present study.
The current study also assessed the reasons of non-compliance by a set of 10 fixed options. Maximum (86.7%) physicians in this study identified lack of adequate facilities and resources as the main reason of non-compliance with standard precaution. Non-availability of PPE was found to be one of the major cause of non-compliance with standard precautions (SPs) among the participants in the Arinze-Onyia, et al. (2018) [7] study, Ndu and Arinze-Onyia (2017) [15] study and Akagbo, Nortey and Ackumey (2017) [19] study. One study in India reported that, PPE not being readily available especially during emergency (Punia, Nair and Shetty, 2014) [16] and another study in Nigeria reported lack of adequate resources as a major reason for non-compliance with SPs [6] but surprisingly another study in India reported that availability of PPE was not the main cause of non-compliance with standard precautions rather lack of training was the main cause [13] .
Excess workload (76.1%), lack of training of infection control (63.2%) and time constrain (43.2%) were the other three main reasons that were considered by the physicians as reasons for non-compliance with standard precautions in the present study. One study in India reported that lack of training was the main reason but time constrain was another cause [13] and HCWs in Nigeria indicated that lack of training (51.9%) was a hindrance to compliance with standard precaution [6] .
Another barrier to adherence to SP in this study was found to be that PPE were not comfortable to use and it was stated by 49.1% of the respondents. This study finding is consistent with finding from other studies [6] [19] . HCWs in Ghana indicated that wearing PPE was uncomfortable (42%) [19] , HCWs (14%) in Nigeria mentioned the same reason [6] but in Fadeyi, et al. (2011) [1] study only 12.5% respondents felt uncomfortable to use PPE but surprisingly 60% respondents felt that it was not essential. Only 6.7% of the respondents in the present study considered that use of PPE may offend the patients. In a study in Ghana, HCWs mentioned that 63% patients felt panic if they wore PPE [19] .
The current study examined the awareness of the physicians handling patients with infectious respiratory diseases and classified them into very poor, poor, moderate and good awareness categories according the percentage of total awareness score. In this study we found that maximum (78.6%) of the physician had a moderate awareness about standard precautions and only 8.1% of the physician had poor awareness and 13.3% of the physician had good awareness about standard precautions. Honarbakhsh, Jahangiri and Ghaem (2018) [14] also classified the knowledge about standard precautions in the similar fashion and found that among the participants of their study 68.7% of the participants had moderate knowledge about standard precautions and only 9.5% and 21.8% of the participants had poor and good knowledge about standard precautions respectively which is more or less similar to the findings of the current study. The similarities between the findings of the two studies regarding awareness of standard precautions could be attributed to the fact that participants of both studies had more or less similar duration of service for current study the mean duration of service is 9 years and the mean duration of service of the participants in the Honarbakhsh, Jahangiri and Ghaem (2018) [14] study was almost 8 years.
The current study also classified the compliance of the physicians with standard precautions in the same categories that is very poor, poor, moderate and good. The current study found that majority (76.5%) of the participants had a moderate compliance with the standard precautions and 23.5% of the participants had good compliance with standard precautions. Honarbakhsh, Jahangiri and Ghaem (2018) [14] found in their study that less than half of the participants had moderate compliance and 36.6% of the participants had good compliance. Though percentage of participants having good compliance with standard precautions is more among the participants of Honarbakhsh, Jahangiri and Ghaem (2018) [14] study but 10.6% and 3.9% of the participants in their study had poor and very poor compliance with standard precautions. The disparity could be due to the fact that the current study only included physicians so none of them had poor compliance with standard precautions but Honarbakhsh, Jahangiri and Ghaem (2018) [14] study included nurses and janitor along with physicians and majority of the participants in their study were nurse and janitor so this could be the reason that some of the participants in their study had poor and very poor compliance with standard precautions.
The current study also found that with increased awareness of the participants regarding standard precautions their mean score of compliance with standard precautions increased which was statistically significant. Ather, Khan and Shabnum (2020) [11] also revealed similar findings. They found that good knowledge about standard precautions positively affected the compliance with standard precautions among the participants.
The present study found that there is no statistical difference of awareness of and compliance with standard precautions between participants having training on infection control and participants who did not have any training on infection control. From this finding inference could be drawn that training on infection control had little or no value on the awareness and compliance of the physicians regarding standard precautions. The reason behind this finding could be due to improper training or lack of monitoring of the physicians who were trained on infection control.
5. Conclusion
The purpose of this cross-sectional study was to assess the level of compliance of physicians with standard precautions of handling patients with infectious respiratory disease. Proper compliance with standard precautions is an important factor in regard to the protection of HCWs including physicians from their workplace occupational hazards especially infectious respiratory diseases. The findings of the current study revealed that most of the physicians handling patients with infectious respiratory diseases had moderate compliance with standard precautions. This study also revealed that most of these physicians had a moderate level of awareness of standard precautions. Physicians who had poor awareness of standard precautions did not follow the standard precautions protocols properly and with increased awareness of standard precautions, physician’s compliance with standard precautions also increased. Very few numbers of physicians had good compliance with standard precaution, which is not satisfactory. Overall compliance level of the physicians with different components of standard precautions which are important to prevent infectious respiratory diseases such as hand hygiene, use of PPE, needle safety, cleaning and disinfection of respiratory equipment and cleaning patient-care environment was also moderate, which begs the attention for improvement and emphasis should be given on the efforts to do it. Some of the main reasons for non-compliance or barrier to compliance with standard precautions pointed out by the participating physicians in this study were lack of adequate facilities and resources for practice of standard precautions, excess workload, lack of regular training on infection control and the fact that PPEs are not comfortable to use.
Limitation of the Study
· The study place was selected purposively and as purposive sampling technique was applied so findings did not reflect the scenario of the entire physicians of country.
· Certain information was recorded by asking question not by observation, so the respondents may have intentionally modified the actual truth.
· There are many chances of recall bias in case of questions related to compliance with standard precautions during handling patients with infectious respiratory disease.
Appendix
Part 1: Socio-demographic characteristics:
Part 2: Assessment of awareness of physicians with standard precautions of handling patients with infectious respiratory disease:
Part 3: Assessment of compliance of physicians with standard precautions of handling patients with infectious respiratory disease:
Part 4: Assessment of reasons for non-compliance of physicians with standard precautions of handling patients with infectious respiratory disease: