COVID-19 Downgraded Already Impaired Mental Health of Medical Undergraduates during the Pandemic Years ()
1. Introduction
A new coronavirus emerged at the end of 2019, with consequences mostly related to severe acute respiratory syndrome (SARS-CoV-2). The syndrome was responsible for affecting more than 430 million people, with more than 5 million deaths in 229 countries [1] . In order to contain its transmission, many countries have adopted non-pharmaceutical measures, such as isolating symptomatic individuals and quarantining their contacts; general physical distancing; closing schools; working remotely, and canceling events and meetings that could have end up in crowding [2] [3] [4] . These insulation measures could have mental health consequences, so that both the infected and uninfected population is vulnerable to generalized anxiety and other conditions [5] [6] . In universities there is an inherent crowding, making it impossible to hold classes in person, a fact that, along with the uncertainty about the return of activities, directly influenced the mental health of university students [7] [8] .
Entering medical school is a successful moment. However, this period can become critical due to the changes in lifestyle that the course requires [9] . Intrinsic to this, the student receives responsibilities, duties and deadlines to which most they were not used to [10] [11] . This change leads some to break family ties and been forced to create new social bonds [9] [10] [11] [12] [13] . In studies conducted with medical students, it has been shown that rates of stress and depression are higher in this audience than in the general population [10] - [15] . The pandemic of COVID-19 (SARS-CoV-2) may be an aggravating factor worsening of this reality, since the schools had to introduce new teaching methods, and the students had to adapt and fulfill the proposed activities, regardless of their capacities or difficulties [16] [17] [18] .
This study assessed mental health and teaching aspects among medical undergraduate students during quarantine imposed due to the SARS-CoV-2 pandemic.
2. Methods
This is a cross-sectional observational study with a non-probability convenience sampling design. After approval by the Research Ethics Committee (CAAE 35666820.2.0000.0068), medical students regularly enrolled in higher education institutions were invited to participate. The inclusion criteria were students regularly enrolled in a Brazilian medical school and over 18 years of age. The exclusion criteria were refusal to give informed consent or incomplete filling of the questionnaire. The survey was disseminated digitally, including mailings to social media groups, which contained medical students or professors from medical schools, and emailed to medical societies that had interface with academics. Each participant was also asked to forward the survey to fellow medical students enrolled in Brazilian medical schools. After 30 days of the first dissemination, a new wage of dissemination was made. The collection of responses was conducted until no more responses were received for a period longer than seven days, which meant opening on August 10, 2020, and closing on October 5, 2020 (55 days).
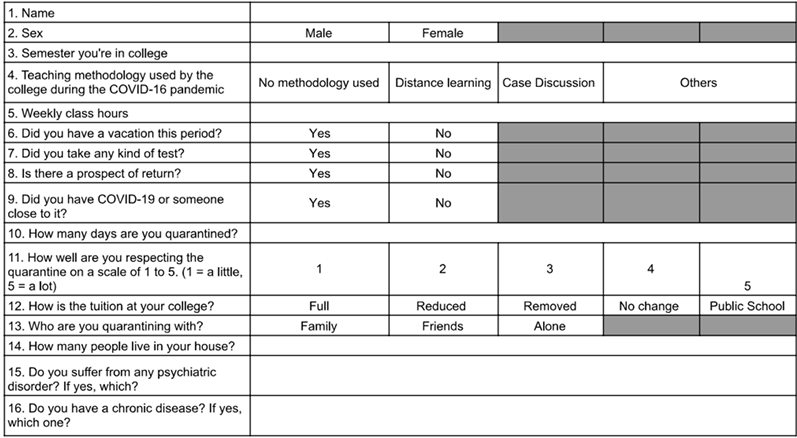
Participants answered the DASS-21 form (21 items) (Appendix 1) and the epidemiological questions (16 items) (Appendix 2), which covered issues related to mental health during quarantine by COVID-19 and social and academic aspects. The questionnaire used to assess stress, anxiety and depression was the reduced version of the DASS scale [19] .
The items are divided into three factors (Items Depression: 3, 5, 10, 13, 16, 17, 21; Anxiety: 2, 4, 7, 9, 15, 19, 20; Stress: 1, 6, 8, 11, 12, 14, 18). The response scale to the items is a four-point Likert type ranging from 0 (did not apply at all) to 3 (applied a lot or most of the time). In the present study, we used the Portuguese version of the DASS-21 [20] . The sum of the values obtained for each sub-item in the DASS-21 was multiplied by 2 to obtain the final score [19] . The DASS-21 cut-off values were considered (Table 1).
Data were managed using the REDCap (Resarch Electronic Data Capture) software [21] [22] . REDCap (University of Vanderbilt, USA) is a secure, digital interface-based system designed to assist in data capture for clinical research, providing an intuitive interface for data feeding, audits to verify data export and insertion, automatic procedures for data export and import.
Statistical Data Analysis
At the time of the survey there were 38.808 authorized university places in 366 higher education institutions for the first year of medical school in Brazil. Considering this, there was a potential amount of 194.227 medical students [23] . The sample calculation estimated a 99% confidence level, with confidence interval at 5%, summing up 663 answers. Considering up to 30% of incompleteness, we estimated a total of 862 answers.
The study used a non-probability convenience sampling design.
Data are presented as median [interquartile] for non-parametric data; and mean ± standard deviation for normal data. To follow these criteria, the variables
were tested by the Shapiro-Wilk test for normality. The association between the variables was tested by the Chi-Squared test for categorical variables. The continuous variables were tested by the Mann-Whitney test or—when the comparison involved more than 2 factors—the Kruskal-Wallis. Variables that showed a p value below 0.20 were selected for multiple analysis using the Binomial regression model. The modeling process began with the variable that presented the lowest p value from bivariate analysis and then, successively, the other variables with a p value lower than 0.20. Remaining in the final model only the variables with a descriptive value below 0.05 (p < 0.05). At last, the odd ratios were estimated for each variable from the final model with its respective CI 95%.
In order to form a multivariate model, the sample was randomly divided in 70% and 30%; this higher percentage was kept for the creation of the model and the lower was used to evaluate the model’s accuracy. The probability of each person having the outcome of this study based on the idealized model was calculated using the 30% of data that was left. When the probability value estimated by the model was above 50%, the individual had a positive outcome. These data were compared with the value obtained from the DASS-21 Scale.
The area under the Receiver Operator Curves (ROC) and the confidence intervals were calculated and compared using the Delong & Clarke-Pearson method [24] . The accuracy was calculated summing the true positive individuals—that is, individuals with a positive outcome for both method and DASS-21 Scale—with the true negative points (individuals selected by the model and DASS-21 Scale that don’t have an outcome) divided by the total of individuals analyzed. The precision was calculated dividing the number of true positives by the sum of true and false positives. The rates of true positives and negatives were calculated dividing the number of true positive or negative individuals by the total positive or negative individuals of the model. The F-Score was calculated by the following mathematical expression:
All of the statistical analyses were realized on R 3.5.1 software (R Foundation for Statistical Computing, Vienna, Austria) and Rstudio (Rstudio Team, Boston, MA). The value of p < 0.05 was adopted for significance level.
3. Results
The survey reached 1009 answers; 663 answers were complete and considered for analysis—275 showed incomplete epidemiological and form data, 64 did not fill completely the DASS-21 form and seven did not sign TCLE. The median age of participants was 22 [3] years old, with 71.9% women, 81% Caucasian. Students were 34.7% at the basic cycle (1st - 4th semester), 51% at the clinical cycle (5th - 8th semester) and 14% (9th - 12th semester) at the internship.
As educational institutions actions, 73.6% were on vacation and the median workload was reduced by 66.7%. This survey reached respondents at 146 [30.0] days of quarantine. Most were on isolation with their parents (99.4%) and 90.3% resided along with 5 people at most. Those under a reduction of workload, 50.5% developed activities through online videoconferencing; 30.5% had only online lessons; 11.6% did not have any activity; 5.4% had other activities and 1.9% had only online case discussions.
A total of 34% of respondents studied at non-profit schools. While 81.5% of those enrolled in for-profit medical schools kept full-tuitions, 17.2% had a certain reduction on their monthly payment and only 1.4% had payment exemption.
The responses showed a profile of 24.3% with a psychiatric illness diagnosis and 15.7% with a chronic disease. Those within risk groups for COVID-19 mortality, 57.3% had pulmonary diseases (including asthma) and 20.5% were obese. Only 3.3% of respondents had COVID-19, but 45.1% had a relative diagnosed with it during the period of research. The adherence to the preventive measures during quarantine reached 80% [25.7].
The median at DASS-21 score was placed in 20 [18] points for stress, 14 [20] for depression and 8 [16] for anxiety, suggesting a prevalence of 77.5% for any disorder and, of these, 63% were in a severe form. When analyzed by disorder, 61.8% had stress criteria, 52.1% of these were classified as severe; 66.6% had depression criteria, 48.1% of these were severe; 56.3% had anxiety criteria; 57.1% classified as severe.
As for anxiety, the previous diagnosis of any other psychiatric disturb was the risk factor with the highest OR (OR 2.78 CI95% 1.44 - 14.25, p = 0.044) followed by the presence of chronic disease (OR 1.83 CI95% 1.07 - 3.19, p = 0.029). Male (OR 0.57 CI95% 0.37 - 0.85, p = 0.078) and age (OR 0.04/year CI95% 0.90 - 0.99 p = 0.016) were protective factors (Table 2). As for severe anxiety, having a chronic disease remains as an independent risk factor (OR 2.15 CI95% 1.28 - 3.61, p = 0.004), as well as having had a relative infected by COVID-19 (OR 1.73 CI95% 0.83 - 0.95, p = 0.006) (Table 2). These models presented AUC of 0.6 (CI95% 0.6 - 0.7), with precision of 59.6% and accuracy at 69.6% for anxiety; and AUC of 0.7 (CI95% 0.6 - 0.7), with precision and accuracy of 64% and 63.2% respectively for a severe form (Table 3).
Depression showed that a previous diagnosis of psychiatric disorder (OR 3.37 CI95% 1.98 - 6.02, p < 0.001) was a risk factor, while male (OR 0.63 CI95% 0.41 - 0.97, p = 0.035) and age (OR 0.094 CI95% 0.89 - 0.99, p = 0.022) were protective factors. In its severe form, a previous psychiatric (OR 2.81 CI95% 1.81 - 4.35, p < 0.001) and chronic diseases (OR 2.18 CI95% 1.27 - 3.71, p = 0.004) were independent risk factors. An expected date to return to on-site activities was a protective factor (OR 0.57 CI95% 0.37 - 0.86, p = 0.007) (Table 2). These models presented an AUC of 0.67 (CI95% 0.6 - 0.7), with precision of 68.1% and accuracy at 67.5% for depression; and an AUC of 0.66 (CI95% 0.61 - 0.71), with precision and accuracy of 61.2% and 70% respectively for its severe form (Table 3).
![]()
Table 2. Multivariate model for anxiety, depression, and stress. Values are Median [IQ].
![]()
Table 3. Area under the curve values for precision, accuracy, true positive rates (TPR) and true negative rates (TNR) for the multivariate models.
Psychiatric (OR 3.70 CI95% 2.21 - 6.44, p = 0.001) as well as a chronic disease (OR 2.09 CI95% 1.19 - 3.83, p = 0.013) and being male (OR 0.56 CI95% 0.37 - 0.86, p = 0.009) were associated independently with stress. Psychiatric (OR 3.18 CI95% 2.03 - 5.00, p < 0.001) and chronic diseases (OR 1.80 CI95% 1.07 - 3.03, p = 0.027) were independent risk factors for a severe form of stress (Table 2). These models presented an AUC of 0.66 (CI95% 0.62 - 0.71), precision and accuracy of 65.9% and 63.4% respectively for stress, and AUC of 0.64 (CI95% 0.59 - 0.69), precision and accuracy of 53.7% and 69.4% for its severe form (Table 3).
4. Discussion
This study showed a high prevalence of stress, depression and anxiety in undergraduate medical students during the first wave of COVID-19, and almost half of them in a severe form. Previous psychiatric disorder was the main risk factor for all three, with the addition of chronic illness for stress, while age and male gender were protective, but not age for stress. Both anxiety and depression in their severe forms have chronic illness was a risk factor, while a relative positive for COVID sum up as risk for anxiety and a psychiatric disorder for depression. Interesting to notice that the expectation for the return of activities was protective for severe form of depression.
Rates of anxiety, stress and depression among medical students vary widely in the literature [25] [26] [27] [28] . Before the COVID-19 era, only 8.3% of this population had any mood disorder, while stress seemed to be a higher as 71% [25] [26] . DASS-21 results suggest around 65% of depression, 61% of anxiety and 75% of stress, with severe forms in the range of 10% - 15% [25] , with incidences varying between men and women [25] [26] [27] [28] .
During the pandemic period, a Chinese sample (2.168 men and 4.975 women) showed anxiety around 75% in this population, a visible increase in this disorder [7] . In our study, beside the high prevalence of stress, depression, and anxiety, we found that the severe forms were much more prevalent, with 52.1% of severe stress, 48.1% of severe depression, and 57.1% of severe anxiety. This sample of medical students worsened their psychological behavior during the pandemic COVID-19.
Confinement, cessation of socializing, lockdown and the severity of the infection actively contributed to this scenario [29] [30] [31] . Among theories about the psychology of such constraints, the S-O-R Model (Stimulus, Organism and Response) states that environmental stimuli (restrictions) may cause psychological detachment, leading to responses like anxiety [31] . Kola L et al. [32] suggested that a higher impact on mental health caused by the COVID-19 was in underdeveloped and developing countries, which includes Brazil, supporting the high prevalence in our results.
As reported in the literature, psychiatric or chronic illnesses were the main factors related to the occurrence of mental health; and now a sick relative – at least during pandemic fear was also a factor. However, protective factors (male and age) did not change [33] [34] . Interesting to notice that female gender was a “permanent” risk factor and the progression in the course reduced depression while anxiety increased. As the literature shows, women tend to have higher rates of physical and mental diseases than men at all ages and in all regions of the world [35] [36] [37] . Our results confirm this theory, and the present article adds that in medical school this observation was maintained during the pandemic COVID-19.
It is known that major stressful life events, such as the COVID-19, can precipitate psychiatric events or aggravate an existing one [38] [39] . This is our hypothesis why students with a previous psychiatric disease were at increased risk of stress, anxiety, and depression disorders. This factor was also present in the severe form of depression and stress. Our model also showed that previous chronic illnesses contributed for all forms of severe anxiety, stress, and depression. Medical students, as well as other health related courses, were more exposed to COVID-19 since most of the course demands patient-interaction. Thus, risk factor for COVID-19 severity, greatly added to sever forms of depression and stress and all form of non-severe diseases [40] . The pandemic years added intensify to all performed models for anxiety, depression, and stress.
Many studies have pointed out that fear of failure, intense workload, time pressure, family expectations and the leaving from parent’s home acted as external stress-triggering events [41] [42] [43] [44] . The newly restrictions included a diversity of negative effects, ranging from sleep-related problems and low academic and professional performance to burnout, self-extermination ideations and putting patients at risk [44] [45] [46] . Medical students are particularly vulnerable to any external event during their long education like the difficult choices or personal and professional challenges. Resilience, perception of hope and compassion are protective against stress, depression and burnout, however, these factors are reduced in medical students, and at potentially sickening levels [47] [48] [49] .
It seems interesting to notice as an outside event not directly related to education could decompensate a stressed, anxious, or depressed student in the field of medicine. This survey suggests the frailty of some medical students as a new stressor factor triggers the total of a psychological load, especially when it implies in sudden new lifestyles.
One of the limitations of the present study includes the data collection that reached 55 days in the period ranging from August to October 2020, representing only the first regional wave of COVID-19. In addition, social restriction and isolation were still tightly controlled, but some teaching activities were in the process of incomplete return. The study did not do any follow-up analysis for evaluation, as the pandemic persisted at the time of writing, with uncertain restrictions.
Anxiety, depression, and stress of medical students were high during the COVID-19 pandemic, half of them in a severe form. Previous psychiatric conditions as well as chronic illnesses were considered risk factors. While male gender was protective for all three conditions, age did not for stress. Interesting, the return to onsite activities protected for depression. Thus, we conclude that COVID-19 was a factor that contributed to the already impaired mental health of medical undergraduates during the pandemic years and that the medical schoolteachers and staff should be in close contact with the students whenever new stressful life events arise.
Data Availability
The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.
Authors’ Contributions
RS Fossa, VC Timaco and MF Vane conceived and designed the study, and participated in the acquisition of data. JMS Moraes and LA Vane supervised the experimental work, contributed to the acquisition of data, and revised the manuscript. EM Martins and RHA Silva participated in the acquisition of data and contributed in writing of the manuscript. JE Vieira, LA Vane and MF Vane analyzed the data, prepared and revised the manuscript. All the authors read and approved the final manuscript.
Acknowledgements
The investigators are grateful to the students who answer the survey to fulfill this work that, they hope, may help students of the health sciences.
Disclosures
All authors of the manuscript have read and agreed to its content and are accountable for all aspects of the accuracy and integrity of the manuscript; The submitted article presents an original work and is not under consideration or reviews by any other publication, as well as has not been published elsewhere in the same or a similar form.
Ethical Board
Certificate of Presentation for Ethical Appreciation (CAAE) 35666820.2.0000.0068; Conselho Nacional de Saúde, Brasil https://plataformabrasil.saude.gov.br/login.jsf.
Appendix
Appendix 1. Dass 21 Scoring

Appendix 2. Epidemiological Questionnaire—Students