Mortality of Children in the Intensive Care Unit of the Pediatric University Hospital of Bangui ()
1. Introduction
In-hospital mortality remains very high in pediatric wards in many low-income countries, particularly in Africa where up to 30% of children die during hospitalization [1] . The World Health Organization (WHO), estimates that 5,700,000 children under the age of 10 years died worldwide in 2019 [2] . Of these, those under 28 days old accounted for 2.4 million, those 1 to 11 months old 1.5 million, those 1 to 4 years old 1.3 million, and 500,000 were 5 to 9 years old [2] . The same report states that older children [5 - 9 years] have experienced one of the largest declines in mortality since 1990 (61%), due to a decline in infectious diseases. Those under 5 years of age continue to die most often from preventable or treatable diseases [2] . While sub-Saharan Africa and Central and South Asia, account for only 52% of the world’s under-5 population, they continue to pay the heaviest toll with more than 80% of the 5.2 million deaths in children under 5 in 2019 [3] . The clinical course of patients is correlated with the severity of the disease on admission and the quality of care in the hospital. Hospitals have an important role in reducing mortality [4] . It has been shown that progress has accelerated in reducing hospital mortality in the West, with pediatric ICU mortality rates ranging from 6.2‰ in the United States to 3.3‰ in France. In contrast, developing countries continue to have record high rates of ICU deaths (21.8‰ in Algeria and 47‰ in Gabon) [5] . A reduction in pediatric mortality in developing countries requires, among other things, the creation of well-equipped and staffed pediatric intensive care units in addition to improving socioeconomic conditions and the health care system [3] [6] [7] [8] . The concept of creating pediatric intensive care units or resuscitation units started about 60 years ago in Sweden and then spread gradually around the world [9] . The creation of the intensive care unit at CHUPB dates back to 1988. The unit was renovated in 2015. It constitutes the only reference structure in the country. Until now, no study has evaluated the mortality of children referred to this unit.
In initiating this study, our goal was to determine the extent of mortality and then to consider the best strategies for improving hospital management of lethal pathologies in children.
2. Material and Methods
Our study took place at the University Pediatric Hospital of Bangui (CHUPB), the only referral hospital and the only structure specialized in the care of children with vital distress in CAR. It receives children between the ages of zero and 15 years, coming from home or referred from a public or private health center in the capital and the provinces. This was a retrospective descriptive study, covering the period from January 1 to December 31, 2021, i.e., one year. We included in the study, children from 1 month to 15 years of age, who died during hospitalization in the intensive care unit of the CHUPB during the study period and whose records were usable (records with all items retained in our survey form). We did not include in the study children between 1 month and 15 years of age with a non-operable medical record and those whose records were marked death on admission to the intensive care unit. For each child included, we collected data related to epidemiological (age, sex, place of residence, origin), anamnestic (reason for hospitalization, time of consultation or hospitalization, symptoms presented before hospitalization, treatment instituted before admission and the child’s history), clinical (general signs, physical examination signs) and paraclinical (Biological: CSF (Cerebrospinal fluid), thick blood drop (GE), CBC, blood ionogram, capillary blood glucose and Morphological: chest X-ray, transfontanellar ultrasound, abdominal and cardiac ultrasound). The data collection started with the obtaining of the research authorization and the favorable opinion of the ethical committee of Bangui; then we presented ourselves to the head of the intensive care unit of the CHUPB. After explaining the purpose of our work, we were given access to the children’s medical records and hospitalization registers. Confidentiality was also respected. There was no conflict of interest. Thus, for each child, the various data collected were entered and analyzed using the SPSS 20.0 statistical software. For word processing we used Microsoft Word 2003. The statistical test used, was Pearson’s chi2, any p-value < 0.05 was considered statistically significant and the Odds ratio was calculated with a 95% confidence interval. As an operational definition:
➢ Early deaths: deaths occurring within 48 hours of admission.
➢ Late deaths: deaths occurring beyond 48 hours of admission.
➢ Coma: Glasgow score less than 8.
➢ Severe malaria: any child with WHO 2015 criteria for severe malaria who had a positive thick blood drop and asexual forms of Plasmodium falciparum on blood smear and or a positive RDT.
➢ Hypoglycemia: The capillary blood glucose values usually used at CHUPB.
• If the blood glucose level is <45 mg/dl (<2.5 mmol/L) in a non-diabetic child who is not severely malnourished.
• In diabetic and severely malnourished children < 55 mg/dl in diabetics.
➢ Severe anemia: hemoglobin < 5 g/dl or hematocrit < 15% in children.
➢ Incomplete record: Record with vital information missing.
➢ Usable records: Records that include a maximum of items from the survey form.
➢ Time to visit: This is the time from the onset of symptoms to the first visit or hospitalization.
3. Results
3.1. Mortality Rate in the Intensive Care Unit of CHUPB
Of the 1489 infants and children hospitalized in the intensive care unit during the study period, 320 had died, for an in-hospital mortality rate of 21.49%. For this work, we selected 251 children according to the inclusion criteria. The flow of children is shown in Diagram 1.
3.2. Epidemiological Data
3.2.1. Sex, Age and Place of Residence
The infants and children were divided into 53.38% (n = 134) males and 46.62%
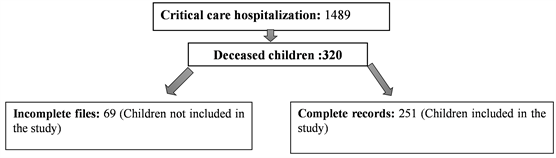
Diagram 1. Flow of children.
(n = 117) females, a sex ratio of 1.14. The mean age of the children was 3.17 ± 2.21 years with a range of 1.03 months to 14.4 years and a median of 3.9 years. The distribution of children according to age groups reveals that 78.49% (n = 197) were under 5 years old versus 21.51% (n = 54). The children came from the urban area of Bangui in 68.53% (n = 172) of cases and from the rural area in 31.47% (n = 79).
3.2.2. Mode d’admission et Période d’hospitalisation
Children came from home in 76.09% (n = 191) of cases—were transferred from health facilities (FOSA) in 17.13% (n = 43) of cases and from a medical office in 6.78% (n = 17).
From month to month, we observed deaths in the intensive care unit of CHUPB of 21.42% (24/112) in January, 18.03% (22/122) in February, 21.15% (22/104) in March, 23.07% (27/117) in April, 14.75% (n = 18/122) in May, and 12.14% (n = 17/140) in June, as shown in Figure 1.
3.3. Consultation Time and Reason for Consultation
The average consultation time was 6.91 ± 1.8 days with extremes of [0.7 - 18.7 days].
It was less than two days in 9.16% (n = 23), between 2 and 5 days in 13.95% (n = 35), greater than or equal to 5 days in 76.89% (n = 193). Fever was the main symptom in 78.48% (n = 197), followed by diarrhea/vomiting in 35.45% (n = 89) and convulsions in 26.29% (n = 66). The reasons for consultation are recorded in Figure 2.
3.4. Children’s History and Prehospital Drug Treatments
A previous history was found in 16.33% (n = 41) of children. These were cardiovascular disease 41.46% (n = 17/41), HIV infection 24.39% (n = 10/41), sickle cell disease 17.09% (n = 7/41), diabetes 14.63% (n = 6/41) and asthma 2.43% (n = 1/41).
3.5. Pre-Hospital Drug Treatments
Before admission, treatment was administered in 73.38% (n = 184) children. It was self-medication 67.39% (n = 124/184) and medical prescription 32.61% (60/184). The type of pre-hospital treatment was antipyretic 35.62% (n = 173/184),
![]()
Figure 1. Distribution of children by month of death.
![]()
Figure 2. Distribution of children according to the main reasons for consultation. *The same child could have one or more symptoms.
traditional herbal medicine 85.32% (n = 157/184), corticosteroid 51.63% (n = 95/184), Anti-malarial 38.58% (n = 71/184), Antibiotic 36.96% (n = 68/184) and others * 36.96% (n = 68/184).
3.6. Vital Parameters
The distribution of children according to vital parameters is recorded in Table 1.
3.7. Paraclinical Data
The rapid diagnostic test for malaria was performed in all cases on admission and was positive in 14.34% (n = 36) of patients. The thick blood sample for haematozoa was performed in all children and was positive in 10.75% (n = 27) of cases. The mean parasite density was 9115.5/mm3 with extremes [80 - 15,900/mm3]. Lood glucose was performed at entry in all cases. The mean blood glucose level was 87.5 ± 7.6 mg/dl with extremes (Lo* - HI**). Glycemic abnormality was noted in 45.94% (n = 201) of cases. It was hypoglycemia in 55.72% (n = 112) of cases and hyperglycemia in 44.27% (n = 89) of cases.
*LO: Low (blood glucose level < 40 mg/dl) ** HI: HIGT (blood glucose level > 500 mg/dl).
![]()
Table 1. Distribution of children according to vital parameters.
Lumbar puncture was performed in 11.95% (n = 30) of cases. The appearance was clear in 46.66% (n = 14/30), cloudy in 43.33% (n = 13/30) and purulent in 10.01% (n = 3/30). The mean glycorrhaphy/blood glucose ratio was 36.5 ± 2.1; extremes (21.34 g/l - 1.7 g/l). Glycorachy was normal in 43.34% (n = 13/30) of cases, hypo-glycorachy in 53.33% (n = 16/30), and hyper-glycorachy in 3.33% (n = 1/30). The mean proteinorachy was 0.92 ± 0.2 g/l; extremes (0.21 - 1.5 g/l). Hyperproteinorachia was noted in 56.66% (n = 17/30) of cases. Pleocytosis was noted in 53.33% (n = 16/30) with a mean value of 234.7/mm3. The culture had isolated germs in 43.34% (n = 13/30) of cases. These are: Streptococcus Pneumoniae 69.23% (n = 9/13), Neisseria meningitidis 23.08% (n = 3/13) and Haemophilus influenzae 7.69% (n = 1/13).
A blood count was performed in all patients. The mean white blood cell count was 5908.5/mm3 with extremes (109 - 85,000/mm3). They were normal in 48.21% (n = 121) of cases, hyperleukocytosis in 42.23% (n = 106) of cases and leukopenia in 9.56% (n = 24) of cases. The mean hemoglobin level was 7.6 g/dl with extremes (2.9 - 13.6 g/dl). This level was normal for age in 38.64% (n = 97) of the cases and below the only normal for age 5 g/dl in 61.35% (n = 154).
The mean platelet count was 140,000.67/mm3; extremes (1100 - 420,000). Thrombocytopenia was noted in 35.45% (n = 89) of cases (Figure 3).
![]()
Figure 3. Distribution of children by platelet count.
The blood ionogram performed in 22.31% (n = 56) of children showed an abnormality in 58.92% (n = 33/56) of cases. Creatinine levels were performed in 165 (65.73%) children with a mean level of 63.6 ± 3 micromole/l. The mean glomerular filtration rate was 132 ± 27 ml/min/1.75m2. A decrease in glomerular filtration rate was noted in 38.78% (64/165) of cases. Renal failure was mild in 43.75% (28/64) of cases—moderate in 32.81% (21/64) of cases—pre-terminal in 15.62% (10/64) of cases and end-stage in 7.81% (5/64) of cases. Among the 85 (33.86%) cases of International Normalized Ratio (INR), hepatocellular insufficiency was noted in 49.41% (42/85) of cases.
A test for acid-fast bacilli (AFB) in sputum was performed in 15.13% (n = 38) of cases and was positive in two (0.79%) children. GeneXpert was performed in 19 (1.89%) children. The result was positive in 63.15% (n = 12/19) of cases. The mean bilirubin level in 55 (21.91%) children was 4.69 ± 1.3 (0.6 - 18.3 mg/dl).
3.8. Main Diagnoses at Time of Death (Table 2)
![]()
Table 2. Distribution of children according to main diagnoses at time of death.
3.9. Length of Stay
The average length of hospital stay before death was 1.82 days with extremes of [0.3 days to 23.2 days]. It was less than or equal to 2 days in 66.53% (n = 167) of cases, and greater than 2 days in 33.46% (n = 84).
3.10. Time of Day of Death and Time of Death
Children died between [16 pm - 8 am] in 68.12% (n = 171) versus 31.88% (n = 80) between [8 am - 16 pm].
3.11. Therapeutic Data
The treatment of the children depended on the clinical orientation and the etiological research. Thus, the drug treatments administered are recorded in Table 3.
![]()
Table 3. Distribution of children according to treatments undertaken in the intensive care unit.
4. Discussion
4.1. Mortality Rates
A well-equipped intensive care unit with modern and innovative intensive care greatly facilitates the care of critical patients giving favorable results [10] . The overall mortality rate in the CHUBP ICU during our study period was 21.49%. This rate is close to the 21.7% found in an Indian pediatric ICU by Vinayak et al in 2017 [11] . Our rate was lower than studies performed in pediatric intensive care units of the continent including 27.5% in Gabon by Essola in 2019 [13] , 36.1% respectively in Egypt and Nigeria [13] [14] . Finally, another Nigerian study found a rate of 38% [15] . On the other hand in the Asian continent, the mortality rate in pediatric intensive care units varies from year to year and from country to country, with rates lower than our observed in India: 18% in 2001 [16] - 6.7% in 2004 [17] - 16.7% in 2009 [18] - 2.1% in 2014 [10] and the Chinese study with a mortality rate of 13.2% in 2005 [19] . Another Indian study conducted in 2018 had found a rate higher than ours and the studies conducted in the said country in previous years 39.4% [20] . The lowest rates are observed in the European and American continent. The overall mortality rate in pediatric intensive care units of 6 geographically diverse teaching hospitals in the United States was about 9 times (2.39% and 2%) lower than ours [21] [22] . This rate was 15% in Brazil in the study by Costa et al. [23] . The European study found an overall mortality rate about 2 times (12%) lower than ours in a Turkish intensive care unit [24] . An efficient ICU contributes greatly to reducing hospital morbidity. With a high mortality rate in the CHUBP ICU, we can say that the quality management of our patients was not optimal. Our institution does not meet the international standard of an intensive care unit in terms of doctor/patient ratio and equipment, which does not allow us to offer high quality care with high intensity medical staff, resulting in very high mortality and longer stays in intensive care units. In contrast, the low rates in Europe and America are due to well-equipped pediatric intensive care units with modern and innovative intensive care, greatly facilitating the management of patients [10] . The very high mortality rates observed in other studies from the African continent are related to the fact that pediatric intensive care in many of these countries includes critical children in pediatric surgery and medicine, with very high death rates in children with head injuries. In contrast, at CHUPB the pediatric intensive care unit is separate from the surgical intensive care and the nutritional therapy unit. The development of intensive care units in many countries of the world has been linked to the development of super-specialties in pediatric resuscitation, but in our country, the unit is managed during the day by a pediatrician and during on-call duty by resident physicians. However, the observed death rate seems to be more a reflection of the inadequacy of several factors including those itinerants to the patients.
4.2. Epidemiological Data
4.2.1. Age and Sex
The mean age of the patients was 3.17 ± 2.21 years with a median of 3.9 years. The mean age of our series was similar to the 3.45 years found by Khilnan in an Indian study [17] . However, a higher mean age (4.9 ± 2.5 years) was found by Embu [14] . The median age in our study was higher than those reported by two Asian studies by Choi and Tyagi, who reported respectively 2 years in China and 1 year in India [19] [20] . In 2019, of the 5.30 million children under 5 years of age who died worldwide - 2.86 million were aged 1 - 59 months, sub-Saharan Africa alone was home to 50% of these deaths, with one in 13 children dying before their fifth birthday [25] . This finding corroborates our data with a predominance of deaths observed in children under five years of age (78.49% in our series). This probability increases between the North and the South. The WHO states that the probability of a child dying before the age of five is sixteen times higher for children in underdeveloped countries than for those in more affluent countries [26] . Our hospital-based results support data from the 2021 Multiple Indicator Cluster Survey in CAR, which reported an infant mortality rate of 99 per 1000 [27] . Our rate was comparable to that of El Halal, which noted an under-five mortality rate of 78.3% [28] . On the other hand, three countries had under-five mortality rates higher than ours, led by Sierra Leone where the infant and child mortality rate is the highest in the world [26] , followed by Somalia and Mali [29] . The predominance of early childhood in our series and in other countries with limited income is probably due to a greater susceptibility of this age group to killer infections in children, to the martial deficiency that is rampant in certain regions of the world, to malnutrition and to precarious socioeconomic conditions, as well as to the lack of vaccination [30] . Moreover, it would certainly be related to the main pathologies observed in countries south of the Sahara, among which we note severe malaria, respiratory infection and rotavirus diarrhea. This hypothesis is reinforced by the WHO observation that severe malaria is particularly frequent in children under 6 months of age [31] . A male predominance is noted in our series with a sex ratio of 1.14. This same male predominance is found by several authors [14] [17] [19] [20] .
4.2.2. Origin of the Children
The majority of children came directly from their homes (76.09%), without going to another health facility in Bangui. This finding was also made in two previous studies conducted in the intensive care unit of the CHUPB, on severe malaria, which found respectively 77.35% and 68.48% of children coming from their homes [32] [33] . The choice of parents to bring sick children directly to the national pediatric referral service, without respecting the health pyramid, would be linked as much to the lack of information on the circuit of access to care as to the fact that treatment is provided free of charge at the CHUPB.
4.2.3. Treatment before Hospitalization
Treatment before hospitalization was administered in 73.38% (n = 184) of whom 67.39% (n = 124/184) were self-medication obtained over the counter. The use of herbal medicine before hospitalization was observed in 85.32% (n = 157/184) of cases. Our results are similar to those of an Ivorian study carried out by McCrossan in Nigeria who noted that pre-hospital treatment was administered in 68.3% of cases, 39.8% of which were self-medication [13] [15] .
This recourse to self-medication is explained in most developing countries by the easy availability of over-the-counter drugs. However, the population also uses herbal medicine inherited from ancestral cultures to avoid long waiting lines in public institutions and to save money. This recourse to herbal medicine is also facilitated by the proximity of the population to traditional healers.
4.2.4. Length of Stay in the Intensive Care Unit
In our study, early death occurred in 66.54% (n = 167). This early death was higher than those observed in the intensive care units of most African countries 46.7% in Ankara [34] , 40% in Ethiopia [35] 41.6% in Egypt [36] . In contrast, in developed countries the mortality rate in pediatric intensive care units was lower: 2.1% in Sweden [37] - 3.9% in Switzerland [38] - 5.9% in the United Kingdom [39] - 6% in Australia [40] and 2.4% in Japan [36] . Although some studies show a correlation between length of stay and outcome in pediatric patients [13] , others show no significant relationship [28] [41] . Deaths in pediatric intensive care are not only related to length of stay but also to other factors such as case type, age, and organizational aspects of the unit [42] . Thus, in our work, deaths were influenced by male gender, origin of residence, rural residence, herbal medicine and the occurrence of deaths during on-call duty after 16 hours. In his study, Dursun had noted that the severity of the disease before admission and the presence of comorbid conditions were important factors for patient survival [24] . He had found that important factors that may have contributed to the survival of these patients, including adequate staffing and equipment and provision of continuing medical education on pediatric intensive care from time to time for the facility staff [24] .
4.2.5. Main Diagnoses at Time of Death
The main diagnoses of death were infectious and cardiocirculatory post infection including Septic Shock 29.08% (n = 73), Hypovolemic Shock post severe acute gastroenteritis 17.13% (n = 43), Severe Malaria 10.76% (n = 27), Bacterial Meningitis 6.38% (n = 16) and Severe Acute Pneumonia 6.38% (n = 16). Infectious etiologies predominate in the causes of death of children in most African studies [12] [13] [14] [15] [35] . These results are consistent with the natural evolution of infections that end in septic shock: the most severe form of infection. It is accompanied by a mortality rate that can be around 25% but unfortunately remains much higher (40% - 45%) in developing countries [43] . Most studies note central nervous system and cardiovascular pathologies as the main etiology of death in children hospitalized in pediatric intensive care units [20] [22] [44] .
4.2.6. Time of Death
In our work, deaths were more recorded between 16 of the evening - 8 of the morning 68.12% (n = 171) with a statistically significant relationship (p = 0.001). This result corroborates that of Chen, who noted that the mortality rate of patients was significantly associated with the working hours of hospital staff [45] . Other authors have reached contradictory conclusions, reporting that the majority of deaths occurred in the first half of the morning [46] [47] . The authors explain this difference by the change of doctors and nurses in the intensive care units (who are more familiar with the patient’s problem) and the higher number of orders and medical procedures of the morning team [46] [47] . However, in our series, this period of the day corresponds to on-call duty, generally supervised by pediatric resident physicians who are not always well equipped to monitor critical children admitted to the intensive care unit. In addition, the nurse in charge of the intensive care unit finishes his shift at 3 pm, as does the pediatrician in charge of the unit. Finally, the technical platform is not operational (certain complementary examinations) during the on-call period.
5. Conclusion
This study allowed us to highlight the real problems of mortality of children hospitalized in the pediatric intensive care unit of the CHUPB, which remains a reflection of the health of critical children in the Central African Republic. Deaths were largely characterized by two quite distinct profiles—the predominance of children under 5 years of age and infectious etiology. The reduction of these deaths requires, among other things, the strengthening of the national program for the control of vaccine-preventable diseases and the strengthening of the extended immunization program. The strengthening of the technical platform is another axis of prevention.
Limitations of the Study
Although we are aware of the limitations of a retrospective study based on the use of hospital data, particularly in relation to the quality of the information reported in the files, limiting the parameters studied to those that are available and usable. We believe that these data largely reflect the real problems posed to the health of critical children in Bangui. The present study concerned children treated in the intensive care unit of the only national referral hospital that handles about 95% of the critical children in Bangui and its surroundings. Thus, the results obtained remain valid for the study setting and do not reflect the situation in the general population where the crude mortality rate was estimated at 20.36 per 1000 in 2019 [27] . Despite this pitfall associated with retrospective studies, this study had the advantage of being carried out in the only referral hospital for the care of children in the CAR. This constitutes sufficient coverage of the pediatric population of Bangui. In addition, the methodological rigor and sample size increased the reliability of the statistical analysis. The data obtained should constitute a hospital reference base for future studies in collaboration with other regional hospitals in the country.