Female Genital Fistula Deemed Incurable in a National Obstetric Fistula Reference Center in Niger ()
1. Introduction
Female genital fistula is a pathology as old as antiquity. Of all the infirmities related to pregnancy, it is the most feared. The notion of this infirmity goes back to the dawn of time: “if a woman has urine that flows continuously, she will lose it all her life” said Papyrus Ebbers 2000 years BC. The prevalence of fistula is higher in under-medicalized poor communities in Africa, especially sub-Saharan Africa and Asia where qualified obstetric assistance is random [1] [2] [3] [4] [5]. It is necessary to highlight the other circumstances of occurrence of fistula like: iatrogenic, that caused by a surgical act or by non-medical trauma such practice (excision, infibulation) neoplasia, congenital, radic and rare infectious cause. Obstetric fistula is caused by dystocic delivery. It is an acquired communication between the lower urinary tract and the genital tract on the one hand and/or between the rectum and the genital tract on the other hand. It is the consequence of a delay in the management of dystocic delivery with prolonged labor. Survivors will have obstetric fistula. In most cases the child dies. If surgery is essential, it is not enough to cure all female victims. Some of these women develop a debilitating chronic form of genital fistula.
Our study focused on female genital fistulas considered incurable observed at Centre National de reference de Fistule Obstétricale National Reference (National Obstetrical Fistula reference center (CNRFO)) of Niamey dedicated to the management of complex cases.
The objective is to make our modest contribution to a better knowledge of this condition by looking at the epidemiological, anatomopathology, treatment and prognosis of 5 cases in a third level center of the health pyramid of Niger for the management of femal genital fistula (fgf).
2. Methodology
This is a retrospective and prospective descriptive study from January 2, 2017 to July 14, 2021 on obstetrical female genital fistulas judged incurable at the (CNRFO) of Niamey. Inclusion criteria was any case of obstetrical female genital fistula operated several times or admitted spontaneously in the service, judged incurable despite adequate surgical care during the period concerned. Were studied obstetric and surgy histories, lesions of vagina, uretra, bladder, treatement results. Were excluded unexplored fistula and non-treated one Data were collected from in service patients files during the period of four and a half years (January 2, 2017-July 14, 2021), then we analyzed those cases considered incurable. All ethical and deontological procedures were respected.
3. Results
During the study period 522 patients were operated, of which 5 cases were considered incurable (0.95%).
Case N˚1: 43 years old primigravid primiparous patient. She delivered by vaginal a stillborn after 3 days of labor. Since then she suffered from fistula for 5 years during which she was operated 5 times. The clinical examination found a severe sclerosis vagina and completely destroyed urethra. On June 14, 2021, the patient was admitted with two fistulas diagnosis, (one urethrovaginal and the second on right median rectovagina). She was operated on August 27, 20021 with the following operative report: 1st step: We practiced H-shaped incision from the bilateral ischio-pubic branch to the urethral wall, horizontal branch at 3 cm from the meatus. Then we did urethrovaginal and vesico-vaginal splitting, on the pubo-cervical fascia flap, then rethral reconstruction from the edges of the H-shaped incision on a Foley probe CH18. The vaginal mucosa was repositioned. In the 2nd step, horizontal incision was made on both sides of the recto-vaginal fistula, and cutano-vulvar of about 1.5 cm. We did fistulorraphy, vulvoplasty on the bulbo-cavernous and repositioned the vaginal mucosa. We fixed Bladder probe on the pubis and vaginal tampon for 24 h (Photo 1).
Case N˚2: 42 year old primigravida patient. The fistula started at 18 years old during a dystocic delivery with prolonged labor of 6 days at home of a stillborn. She was operated for fistula successively on January 8, 2012; March 22, 2013; November 15, 2013, August 5, 2015 June 12, 2016 without success. Then she was referred: March 4, 2018 at NRFO. She had an extensive supra trigonal fistula with the vesical part remaining prolapsed into the vagina (Photo 2).
Case N˚3: 49 years old primigravida patient suffering from fgf for 12 years with history of several unsuccessful attempts of surgical cure: in 2010, August 2012, November 2013, June 2014. The examination on July 13, 2018: at NRFO found severe sclerosis vagina, posterior vaginal flange, urethra partially destroyed in the proximal 1/3. and endovaginal meatus. The blader destroyed with important bladder substance loss (Photo 3).
Case N˚4: 39 years old primigravida patient living with fistiula since 17 years with multiple interventions cure of fgf of which the last one goes back to February 2005 Admitted to the CNRFO, she benefited from a cystolithotomy by vaginal way in 2017. Fistula is extensive supra-trigonal with transsection and total absence of the urethra. We preceded to the catheterization of ureters then, Dome incision following the ischio-pubic arches, dissection of the Retzuis. We did Vesico-vaginal splitting posteriorly, sub pubic urethralization, retro trigonal and trigonal reconstruction, and fixed of the urethral stump obtained under the pubic. Then repositioned the vaginal mucosa and fixed the Foley 18 probe under pubic, placed vaginal tampon for 24 hours. On July 30, 2019, the loss of urine continued all the time. So the fistula was declared Incurable Wide urethrovaginal fistula with total urethral destruction (Photo 4).
Case N˚5: 37 year old primigravida patient came to the cnrfo on January 2, 2017 for urinary incontinence for 6 years, with 5 successive operations. The examination discovered a severe vaginal sclerosis, prolapse of the bladder dome mucous, urethra completely destroyed therefore extensive supra trigonal fistula with total urethral destruction and pyuria. It was operated on October 09, 2018 by right ureteral catheterization (left ureter not visualized), vesico-vaginal and vesico-cervical splitting, detachment of the Retzuis vesical neck, reconstruction of the anterior face of the urethra, trigonal reconstruction by apposition of the supra-trigonal bladder mucosa, repositioning of the vaginal mucosa. The patient was Rehospitalised on March 28, 2019. It was tried urethral reconstruction on micro bladder by Incision on the edges of the vaginal/bladder mucosa, vesico-vaginal splitting, parallel longitudinal incision on the urethral bed, making a trigonal flap which is sutured, repositioning of the vaginal mucosa. Foley 14 catheter was placed for 7 days and vaginal tampon for 48 hours. On March 29, 2019 was removed vaginal tampon, but she continued urinaryincontinence the next day (Photo 5).

Photo 1. Vagin sclerotic obstructed vagina (medical file case N˚1).

Photo 2. Urethral destruction on severe sclerosis (medical file case N˚2).

Photo 3. Fail uretral reconstruction (medical file of case N˚3).
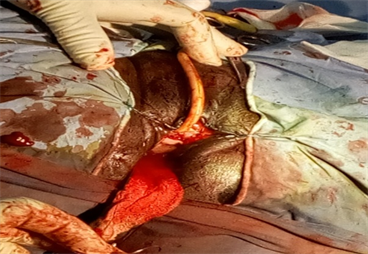
Photo 4. Sclerotic obstructed vagina, fail uretral reconstruction (medical file of case 4).

Photo 5. Extensive lesion with obstructive vagian, no uretra (medical filecase N˚5).
We did not do urinary diversions for all 5 cases
4. Discussion/Comment
In this study, 522 cases of female genital fistula were operated on in 5 years, of which (0.95%) were considered incurable. The 5 patients were aged 37 to 49 years. Studies [1] - [10] report younger cases. They were primigest primipares in contrast to the 62% of multipares of 132 cases of Zaghbib [6] with an average age of 44 years; in 2017, in Niger, a 15-month prospective multicenter study [3] reported 12 out of 148 cases (4.10%) fistulas not closed but not considered incurable.
The lesions in the 5 cases were in the form of extensive uretral, vesical tissues destruction, and with 80% of severe vaginal sclerosis. Alessandri [9] reported 9.09% failure for 2/22 cases operated between 2009-2016. Indeed, each failure of surgical treatment leads to a new sclerosis that is added to it. The lack of flexibility of the vaginal walls is a major problem to the success of surgical treatment.
The patients lived for several years “in the urine”, the oldest of whom was 49 years old. We note in fact that these are, in most cases, fistulas acquired a very long time ago, and that thanks to the obvious involvement of some and others, and the multiplication of awareness campaigns, these women continue to keep the hope of recovery and vote in different health facilities after failing treatement. Is it the long duration of labor, the duration of the fistula and the leakage of urine or the attempts by non-expert or unskilled hands that led to the failure of the treatment? The therapeutic result would be influenced by the time before the fistula is managed, i.e. the age of the fg [4] [6] [9] [10], the state of the peri-fistula tissue (vaginal sclerosis), the extent of urethral and bladder tissue destruction, but also by the association of a recto-vaginal fistula with iterative surgical interventions. In this case, the number of cases of fistula and infection of the urogenital tract [4] [5] [6] [7] was 66/384 17.19%. Nsambi notes four criteria as risk factors for predictive failure of repair of obstetric vesico-vaginal fistula: scar fibrosis, presence of 2 or more fistulas, transvesical approach, and urethral involvement; Ureteral shunts do not improve the prognosis in fact those benefiting from this alternative did not survive long [3].
5. Conclusion
Given the failure of treatment, the best treatment is prevention, whether primary or secondary. We dare to hope for the definitive eradication of this preventable disease. Access to essential and complete obstetrical care is the key to the prevention of obstetrical female genital fistula origine.