1. Introduction
What is meant by intellectual disability is: a person’s intelligence less than the average.
Natural: the incomplete development of a person’s nervous system, which leads to his inability to adapt to himself with the environment around him.
Intellectual disability has several causes, the most important of which are the genetic diseases, the mother and fetus being infected with some diseases during pregnancy, such as German measles, mother’s malnutrition, diabetes, or mother’s exposure to X-rays and pregnancy at a later age, and other reasons.
The city of Damascus paid great attention to the categories of intellectual disability, so it established centers and associations for their education and rehabilitation, and held many seminars to praise them and their rights, in addition to the other services it provided and was still providing towards this category. Since Down syndrome is the most common mental disability in the world, it was chosen to be highlighting it in this article.
2. Search Objective
Raising awareness of the role of people with Down syndrome in societies and finding ways to explore their creative skills, how to properly deal with them, and to raise more special education methods appropriate to their mental health.
The research aims to develop awareness in society about “Down Syndrome” and change the prevailing view of children with it and deal with them in a decent manner and without shame or shyness from society, which results in negative effects that delay the rehabilitation of this forgotten group about which little is known.
Knowing the family and environmental conditions that a person with Down syndrome is currently experiencing within his family, in addition to the extent of the family’s interest and knowledge of him and his rights.
3. Definition of Down Syndrome
Down syndrome is a condition in which a person has an extra chromosome. Chromosomes are small “packages” of genes in the body. They determine how a baby’s body forms and functions as it grows during pregnancy and after birth. Typically, a baby is born with 46 chromosomes. Babies with Down syndrome have an extra copy of one of these chromosomes, chromosome 21. A medical term for having an extra copy of a chromosome is “trisomy”. Down syndrome is also referred to as Trisomy 21. This extra copy changes how the baby’s body and brain develop, which can cause both mental and physical challenges for the baby. Even though people with Down syndrome might act and look similar, each person has different abilities. People with Down syndrome usually have an IQ (a measure of intelligence) in the mildly-to-moderately low range and are slower to speak than other children (Fletcher-Janzen, 2007).
4. Characteristics of Children with Down Syndrome
4.1. Physical Fairies
People with Down syndrome often have a characteristic facial appearance that includes a flattened appearance to the face, outside corners of the eyes that point upward, small ears, a short neck, and a tongue that tends to stick out of the mouth. Affected individuals may have a variety of birth defects. Many people with Down syndrome have small hands and feet and a single crease across the palms of the hands (Howard, 2013).
Face and extremities: a flat and wide face, (Kausik, 2013) a short neck, excessive joint flexibility, extra space between big toe and second toe, abnormal patterns on the fingertips and short fingers (David, 2013). Instability of the joint occurs in about 20% and may lead to spinal cord injury in 1% - 2%. Hip dislocations may occur without trauma in up to a third of people with Down syndrome.
Weight and height: Weight and height are affected in children with Down syndrome, where their birth weight is less than normal Natural, Growth in height is slower, resulting in adults who tend to have short stature: the average height for men is 154 cm (5 ft 1 in) and for women is 142 cm (4 ft 8 in). Individuals with Down syndrome are at increased risk for obesity as they age. Growth charts have been developed specifically for children with Down syndrome (Kliegma, 2011).
4.2. Neurological Characteristics
This syndrome causes about a third of cases of intellectual disability (Hammer, 2010). Many developmental milestones are delayed with the ability to crawl typically occurring around 8 months rather than 5 months and the ability to walk independently typically occurring around 21 months rather than 14 months (Rondal & Quartino, 2007). Most individuals with Down syndrome have mild (IQ: 50 - 69) or moderate (IQ: 35 - 50) intellectual disability with some cases having severe (IQ: 20 - 35) difficulties (Weijerman & de Winter, 2010). Those with mosaic Down syndrome typically have IQ scores 10 - 30 points higher than that (Batshaw, 2005). As they age, people with Down syndrome typically perform worse than their same-age peers (Reilly, 2012). Commonly, individuals with Down syndrome have better language understanding than ability to speak (Graber et al., 2012). Between 10% and 45% have either a stutter or rapid and irregular speech, making it difficult to understand them (Patterson, 2013). After reaching 30 years of age, some may lose their ability to speak (Malt et al., 2013). They typically do fairly well with social skills (Kent & Vorperian, 2013). Behavior problems are not generally as great an issue as in other syndromes associated with intellectual disability. In children with Down syndrome, mental illness occurs in nearly 30% with autism occurring in 5% - 10% (William, 2012). People with Down syndrome experience a wide range of emotions. (Margulies, 2007). While people with Down syndrome are generally happy (McGuire & Chicoine, 2006), symptoms of depression and anxiety may develop in early adulthood. Children and adults with Down syndrome are at increased risk of epileptic seizures, which occur in 5% - 10% of children and up to 50% of adults (CDC, 2013). This includes an increased risk of a specific type of seizure called infantile spasms. Many (15%) who live 40 years or longer develop Alzheimer’s disease. In those who reach 60 years of age, 50% - 70% have the disease (Rodman & Pine, 2012).
4.3. Sensory Properties
Hearing and vision disorders occur in more than half of people with Down syndrome. Vision problems occur in 38% to 80%. Between 20% and 50% have strabismus, in which the two eyes do not move together (Goldstein, 2011). Cataracts (cloudiness of the lens of the eye) occur in 15% (Fay, 2009), and may be present at birth (Melmed et al., 2011). (a thin, cone-shaped cornea) and glaucoma (increased eye pressure) are also more common (Weijerman & de Winter, 2010), as are refractive errors requiring glasses or contacts (Malt et al., 2013). Burchfield spots (small white or grayish/brown spots on the outer part of the iris) are present in 38% to 85% of individuals (Patterson, 2013). Hearing problems are found in 50% - 90% of children with Down syndrome. This is often the result of otitis media with effusion which occurs in 50% - 70% and chronic ear infections which occur in 40% to 60% (Fay, 2009). Ear infections often begin in the first year of life and are partly due to poor Eustachian tube function (Epstein, 2007). Excessive ear wax can also cause hearing loss due to obstruction of the outer ear canal (Mai et al., 2019). Even a mild degree of hearing loss can have negative consequences for speech, language understanding, and academics. It is important to rule out hearing loss as a factor in social and cognitive deterioration (Domino, 2007). Age-related hearing loss of the sensor neural type occurs at a much earlier age and affects 10% - 70% of people with Down syndrome (Kliegma, 2011).
4.4. Cardiac Problems
The rate of congenital heart disease in newborns with Down syndrome is around 40%. Of those with heart disease, about 80% have an atrioventricular septal defect or ventricular septal defect with the former being more common. Mitral valve problems become common as people age, even in those without heart problems at birth (Malt et al., 2013). Other problems that may occur include tetra logy of Fallout and patent ducts arteriosus. People with Down syndrome have a lower risk of hardening of the arteries (Goldstein, 2011).
4.5. Blood Cancers
Leukemia is 10 to 15 times more common in children with Down syndrome (Hickey et al., 2012). In particular, acute lymphoblastic leukemia is 20 times more common and the megakaryoblastic form of acute myeloid leukemia (acute megakaryoblastic leukemia), is 500 times more common. Acute megakaryoblastic leukemia (AMKL) is a leukemia of megakaryoblasts, the precursors cells to megakaryocytic which form blood platelets. Acute lymphoblastic leukemia in Down syndrome accounts for 1% - 3% of all childhood cases of ALL. It occurs most often in those older than nine years or having a white blood cell count greater than 50,000 per micro liter and is rare in those younger than one year old. ALL in Down syndrome tends to have poorer outcomes than other cases of ALL in people without Down syndrome (Hammer, 2010). Down syndrome, AMKL is typically preceded by transient myeloproliferative disease (TMD), a disorder of blood cell production in which non-cancerous megakaryoblasts with a mutation in the GATA1 gene rapidly divide during the later period of pregnancy. The condition affects 3% - 10% of babies with Down. While it often spontaneously resolves within three months of birth, it can cause serious blood, liver, or other complications. In about 10% of cases, TMD progresses to AMKL during the three months to five years following its resolution (Batshaw, 2005).
4.6. Endocrine
Problems of the thyroid gland occur in 20% - 50% of individuals with Down syndrome. Low thyroid is the most common form, occurring in almost half of all individuals. Thyroid problems can be due to a poorly or nonfunctioning thyroid at birth (known as congenital hypothyroidism) which occurs in 1% (Hickey et al., 2012) or can develop later due to an attack on the thyroid by the immune system resulting in Graves’ disease or autoimmune hypothyroidism. Type 1 diabetes mellitus is also more common. Thyroid problems can be due to a poorly or nonfunctioning thyroid at birth (known as congenital hypothyroidism) which occurs in 1% (Weijerman & de Winter, 2010) or can develop later due to an attack on the thyroid by the immune system resulting in Graves’ disease or autoimmune hypothyroidism. Type 1 diabetes mellitus is also more common (Batshaw 2005).
5. Mental Health
Depressive illness is more common in people with Down’s syndrome, and mental health problems generally are more common in people with learning disability. Mental health assessment may be required if the patient presents with changes in behavior or mood, or loss of skills. Recognize a range of associated psychological and physical conditions, some of which may profoundly affect a person’s capacity for self-care, mobility or communication Identify, monitor and review all patients who have difficulties with communication, social relationships and managing their own affairs; this may require additional skills in diagnosis, examination and consultation, and an understanding of legislation and guidance on mental capacity Carry out annual health checks for people with intellectual disability. Be aware of the effects of intellectual disability on the life history of the patient and family. Signpost patients and their families to appropriate resources, knowing when and where to seek specialist help. Support people transitioning from paediatric to adult services. Advocate for people with intellectual and social disabilities; promote fairness and equity in the community, including equal access to health care children with Down syndrome. Pediatrics 128: 393-4.
6. Emerging Issues
All mainstream services should offer patients with intellectual disabilities professional resources and facilities that are appropriate and tailored to their needs. The GP may be the only significant medical practitioner in their lives. GPs need to address issues facing people with intellectual disability; this must also include awareness of the needs of people with social and adaptive problems. Difficulties include poor social functioning, employment issues, mental health problems and lack of support from mainstream services (e.g. learning disability teams).
7. The Causes of Down Syndrome
The cause of the extra full or partial chromosome is still unknown (Prasher, 2009). Most of the time, Down syndrome is caused by a random mistake in cell division during early development of the fetus, but not inherited, (Tamblyn et al., 2016) and no scientific research shows that environmental factors or the parents’ activities contribute to Down syndrome. The only factor that has been linked to the increased chance of having a baby with Down syndrome is maternal age (Seewald et al., 2012). Karyotypes for trisomy Down syndrome: notice the three copies of chromosome 21. Down syndrome is caused by having three copies of the genes on chromosome 21, rather than the usual two (Lee et al., 2016). The parents of the affected individual are typically genetically normal (Gamis & Smith, 2012). Those who have one child with Down syndrome have about a 1% possibility of having a second child with the syndrome, if both parents are found to have normal karyotypes. The extra chromosome content can arise through several different ways. The most common cause (about 92% - 95% of cases) is a complete extra copy of chromosome 21, resulting in trisomy 21 (Tintinalli, 2010). In 1.0 to 2.5% of cases, some of the cells in the body are normal and others have trisomy 21, known as mosaic Down syndrome (National Down Syndrome society, 2022; Mayo clinic). The other common mechanisms that can give rise to Down syndrome include: a Robertsonian translocation, isochromosome, or ring chromosome. These contain additional material from chromosome 21 and occur in about 2.5% of cases. An isochromosome results when the two long arms of a chromosome separate together rather than the long and short arm separating together during egg or sperm development (Lana et al., 2011).
8. Types of Down Syndrome
8.1. Trisomy 21
Trisomy 21 (also known by the karyotypes 47, XX, +21 for females and 47, XY, +21 for males) (Menkes & Sarnat, 2005) is caused by a failure of the 21st chromosome to separate during egg or sperm development (nondisjunction) (Tintinalli, 2010). As a result, a sperm or egg cell is produced with an extra copy of chromosome 21; this cell thus has 24 chromosomes. When combined with a normal cell from the other parent, the baby has 47 chromosomes, with three copies of chromosome 21 (Bhatnagar et al., 2016). About 88% of cases of trisomy 21 result from nonseparation of the chromosomes in the mother, 8% from nonseparation in the father, and 3% after the egg and sperm have merged (National Down Syndrome Society, 2022).
8.2. Mosaicism
Mosaicism is diagnosed when there is a mixture of two types of cells: some cells have three copies of chromosome 21 but some cells have the typical two copies of chromosome 21. Mosaicism is the least common form of Down syndrome and accounts for only about 1% of all cases of Down syndrome (CDC, 2021). Children with mosaic Down syndrome may have the same features as other children with Down syndrome. However, they may have fewer characteristics of the condition due to the presence of some (or many) cells with a typical number of chromosomes (Patterson, 2009).
8.3. Translocation
The extra chromosome 21 material may also occur due to a Robertsonian translocation in 2% - 4% of cases (Zhang, 2008, National Down syndrome society, 2022). In this situation, the long arm of chromosome 21 is attached to another chromosome, often chromosome 14. (Mayo clinic 2022) In a male affected with Down syndrome, it results in a karyotypes of 46XY, t(14q21q). This may be a new mutation or previously present in one of the parents. The parent with such a translocation is usually normal physically and mentally; (Nelson, 2011) however, during production of egg or sperm cells, a higher chance of creating reproductive cells with extra chromosome 21 material exists (Strauss & Barbieri, 2009). This results in a 15% chance of having a child with Down syndrome when the mother is affected and a less than 5% probability if the father is affected (Michael, 2013). The probability of this type of Down syndrome is not related to the mother’s age. Some children without Down syndrome may inherit the translocation and have a higher probability of having children of their own with Down syndrome (Bull, 2011). In this case it is sometimes known as familial Down syndrome (Gardner et al., 2011).
9. Materials and Working Methods
(Materials) Prepare a questionnaire as follows:
1) What is the gender of a person with Down’s syndrome?
2) How old is Down’s syndrome?
3) When has Down’s syndrome been detected?
4) Was the mother taking medication during pregnancy?
5) If the answer to the previous question is yes, what is the name of the drug?
6) Was the mother suffering from an illness during pregnancy?
7) If the answer to the previous question is yes, what is the name of the disease?
8) Was the mother malnourished during pregnancy?
9) Was the mother performing periodic examinations during pregnancy?
10) Is the father a relative of the mother?
11) Did the mother have another child with the same syndrome?
12) Has the same syndrome been recorded in the history of the father’s family?
13) Has the same syndrome been recorded in the history of the mother’s family?
14) Does Down’s syndrome have another disability?
15) If the answer to the previous question is yes, what kind of disability?
16) Does the patient have hearing or vision problems?
17) Does the patient have heart problems?
18) Does the patient have digestive problems?
19) Does the patient have respiratory problems?
20) Was the child presented to doctors when his postpartum qualities were observed?
21) Is the patient still being shown to doctors?
22) Has the patient been enrolled in rehabilitation, education and development centers?
23) Is the patient hidden from sight?
24) Is the patient differentiated in treatment and attention from the rest of the family?
25) If the answer to the previous question is yes or sometimes, what kind of distinction in terms of increase or shortage?
26) Are you having difficulty caring for and dealing with the infected?
27) Do you support the idea of integrating them with ordinary schools
28) Do you support the condition being described as Down’s syndrome instead of Mongolian?
29) Do you see marriage as a right of persons with Down’s syndrome and should be made available to them?
30) Do you support preventing people with Down’s syndrome from and procreating?
31) Did the father play a role in raising Down’s syndrome?
32) Do you spend time with your child with Down’s syndrome for their education and development?
33) Are the rest of the children ashamed that their brother has Down’s syndrome?
34) Have the patient’s brothers been made aware of the importance of not diminishing their brother and that he is equal to them
35) Was the mother blamed by relatives and society for being the cause of her child’s Down’s syndrome?
36) Have you been given priority in government departments, hospitals and public facilities due to the presence of someone with Down’s syndrome in the family?
37) How satisfied are you with services for Down’s syndrome?
In your opinion, what do Down’s patients need in Syria?
10. Method
Distribution of identification:
A number of questionnaires were distributed to a number of people from Down’s syndrome through centers and associations with special needs. These are: The Beit Al-Eila Association, Damascus-Shipyard Association, The center of my different footprint & Supporting pages for Down’s syndrome via Facebook.
11. Collection of Questionnaires
The questionnaires were collected and took up to three weeks to compile Statistical analysis of the questionnaire. Analyze the data for the messages in the questionnaire by finding the percentage. For each question, represent them in a graph and then interpret and discuss the results. The percentage is found using the following equation: Percentage for each question = ×100.
12. Results and Discussion
The current study was conducted based on a questionnaire for people with Down syndrome. It was found through the following questionnaire:
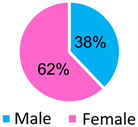
1) Gender of a person with down’s syndrome
2) Age and down syndrome

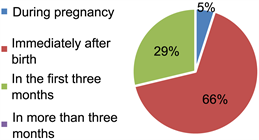
3) Down syndrome detection period
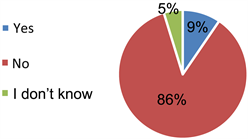
4) Maternal drug use during pregnancy and its relationship to Down syndrome

5) The mother has a certain disease and Down syndrome

6) Did the mother suffer from malnutrition during pregnancy
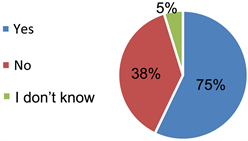
7) Does the mother perform periodic examinations during pregnancy
8) Is the father a relative of the mother?
9) Did the mother have another child with the same syndrome?
10) Have you recorded the same syndrome in the history of the father’s family?
11) Recorded the same syndrome in the history of the mother’s family?
12) Does Down syndrome have another disability?
13) Does the patient have hearing or vision problems?
14) Does the patient have heart problems?
15) Does the patient have digestive problems?
16) Does the patient have respiratory problems?
17) Has the baby been shown to doctors when observing his postpartum qualities?

18) Is the patient still being shown to doctors?
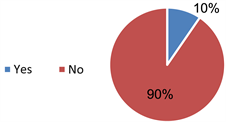
19) Is the patient registered centers for education and development?
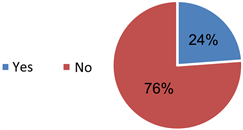
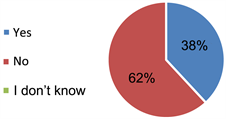
![]()
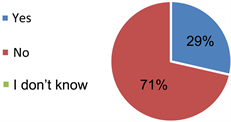
20) Is the patient hidden from view?
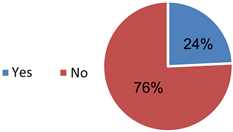
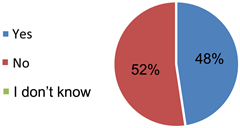
![]()
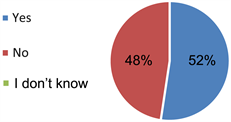
21) Is the patient differentiated in treatment and attention from the rest of the family?
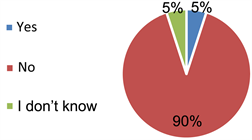
![]()
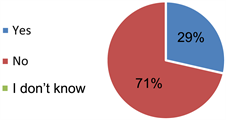
22) Do you find it difficult to deal with and take care of the injured?
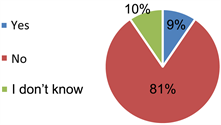
![]()
13. Conclusion
From this research, Down’s syndrome is a chromosomal anomaly leading to features and congenital defects in the organs and functions of the body. Psychological and moral support and independence must be provided and supported in developing themselves and trying to integrate them more into society, focusing on being an active element and being one of the people of determination but needing support and belief because they are different but capable, changing society’s perception of them and securing suitable employment opportunities for them.
14. Case Study
Ghena a successful story (We are different, but we can) A 29-year-old girl from Love Syndrome is different, but she is capable, as she is an actress in the theater and works with soap and perfume. She grew up in a family that did not appreciate her. They did not place hope in her one day. They did not seek to educate her or develop her. They did not support her. Ghena did not believe her family in her and her abilities. She only served her family at home before she reached this stage of success and strength of character. But how did she reach? Ghena joined Beit Al Aila Center when she was 4 years old, and Madame Suhair embraced her, as the rest of the children embraced her, as if she was her real child. Ghena is an example of love syndrome. She has achieved great successes and received many medals, got acquainted with the first lady and received a reward of 100,000 Syrian pounds from her before the crisis in Syria because she was able to dream and able to achieve her dreams, able to work hard, and able to work, able to achieve what he wants in order to produce an integrated educated society with all its members.