Influence of Climate Variability on the Dynamics of Malaria Transmission among Children in Bangui, Health Challenges in Central African Republic ()
1. Introduction
Climate change is now one of the most significant challenges facing our Planet. The global temperature has risen by about 0.6˚C since the end of the 19th century, and the Intergovernmental meeting on Climate Change estimates that the average increase in the earth’s surface temperature by 2100 will range from 0.3˚C to 1.7˚C [1]. Weli noted in a Nigerian study an increase in urban temperature of 3˚C in sixty-five years (1950 to 2014) [2]. The potential influences of these changes on health are multiple and linked. For example, it is estimated that between 2030 and 2050, climate change is expected to generate nearly 300,000 additional deaths per year by increasing child malnutrition and undernutrition, insect-borne diseases, diarrhea, and heat-related stresses [3]. Entomologists are convinced that the expansion of hot and humid areas across the globe would increase tenfold the population of disease-carrying insects [3]. Malaria is one of the most important vector-borne diseases in tropical and subtropical regions. Climate change is already responsible for about 6% of malaria cases worldwide and in some middle-income countries [4]. Pascual et al. noted that mosquito abundance is amplified with global warming, with more than a tenfold increase with each unit (1˚C) increase in temperature [5]. The WHO in its latest 2021 Report noted an increase in malaria cases in the world in 2020 compared to 2019 (241 million against 227 million); that is to say an estimated 14 million more malaria cases in 2020. Most of this increase will be in the countries of the WHO African Region [6]. Relative mortality is estimated at 627,000 worldwide, of which 384,000 will be in the WHO African Region in 2020 [7]. Children under 5 years old continue to pay the highest burden with 80% of all malaria deaths. Of the 5.30 million deaths in children under 5 in 2019, malaria accounted for 0.42 million [8]. In the Central African Republic, malaria is the leading cause of child morbidity and mortality. It was responsible for 23% of hospital deaths in 2005 compared to 16.95% in 2017 [9] and 24.24% in 2019 [10]. It affects 32.2% of children under 5 years of age, who constitute with pregnant women the most vulnerable group [11]. In Bangui, several studies have been conducted in the fight against malaria [9] [10], but none of them deal with the effect of climate on health, nor do public health campaigns give much importance to climate, yet the deepening of climatic knowledge of the Central African Republic is of fundamental importance to address the problem of malaria today at the public health level. This study was based on the hypothesis that climate influences malaria morbidity and mortality in children in Bangui. The objective of this study was to assess the relationship between climate and malaria epidemiology in children under 5 years old in Bangui.
2. Patients and Methods
2.1. Study Site
The capital of Central African Republic, located in the southwest of the country and bathed by the Oubangui River, served as the setting for the study. It extends between 4˚20'50'' and 4˚25'21'' north latitude and 18˚31'41'' and 18˚38'00'' of longitude. The area of this zone covers 94 km2 in 2010, with an estimated population of 1,145,280 inhabitants in 2015.
2.2. Data Collection and Study Variables
Data collection was done prospectively and retrospectively over a 12-year period from January 1, 2004 to December 31, 2015. Health data were obtained from the database of the Bangui Pediatric Hospital and from the Bangui Health Region N˚7 (HR7). We included children under five years of age with malaria (simple or severe form) confirmed by parasitological examination (blood smear and thick drop). For each child, we recorded the age, the period of the malaria episode (month and year), the place of residence, and the outcome of the disease (alive or death). The climatic data used were related to rainfall, humidity (hygrometric degree) and temperature provided by the meteorological station of Bangui M’poko (ASECNA) and the National Delegation of Meteorology of Bangui. Demographic data were collected from the United Nations Population Fund (UNFPA) and the Central African Institute of Statistics, Economic and Social Studies (ICASEES). They covered the annual population of children under five years of age in HR7. The dependent variable was malaria-related morbidity and mortality. The independent variables refer to community and household characteristics (household wastewater management, household waste management, illegal dumping of garbage in the markets of the different districts, the presence of piles of garbage in public places, tall grass, stagnation of wastewater and pollution, blocked drainage channels, anarchic construction of housing; the existence of latrines and their maintenance). The standard of living variable is created from the comfort of the dwelling and the possession of certain goods by the household. At the end of the survey, the districts were classified as very vulnerable, medium vulnerable, low vulnerable and very low vulnerable.
2.3. Ethical Considerations
During this study, we collected meteorological, demographic and health data. For this purpose, an ethical clearance was obtained from the local ethics committee, which allowed us to access the data from each institution. The protocol included a protection protocol that described potential risks during the survey life cycle and management strategies to mitigate them. Data collection, entry, and analysis of general and health-specific data were confidentially conducted.
2.4. Statistical Data Processing Methods
Several statistical methods were used to collect and analyze the data:
The highlighting of climatic trends in the study area and its seasonal variations was done by the monthly rainfall coefficient d’Alfred Angot: Cm = 12Pm/P, with aridity index of Gaussen P = 2t.
The malaria spread index by rounding was calculated using the mathematical formula of Macdonald:
.
The establishment of the relationship was done by Pearson’s linear correlation coefficient (r), showing the intensity and meaning of the relationship:
. With a correlation coefficient varying between −1 and +1, 0 reflecting a zero relationship between the two variables, a negative value (negative correlation) meaning that when one of the variables increases, the other decreases; while a positive value (positive correlation) indicates that the two variables vary together in the same direction.
3. Results
3.1. Average Monthly Umbrothermal Diagram of Bangui from 2004 to 2015
The average umbrathermic diagram of Bangui (Figure 1) shows that the amount of monthly rainfall is changing at the same rate as temperatures. The month of October, which recorded 202.28 mm of water, has a temperature equal to
![]()
Figure 1. Average umbrathermic diagram of Bangui.
27.51˚C compared to the months of January to May where temperatures oscillate from 27.17˚C to 28.53˚C.
3.2. Anomalies in Annual Rainfall Trends in Bangui, 2004 to 2015
The analysis of anomalies of Bangui’s annual rainfall trends from 2004 to 2015, counts 8 years in surplus against 4 years in deficit, a difference of 685.7% (Figure 2). The annual precipitation was 1545.8 mm.
3.3. Anomalies of Annual Humidity Indices in Bangui, 2004 to 2015
The anomalies of annual humidity indices in Bangui from 2004 to 2015 show 7 years of surplus against 5 years of deficit, which is an annual difference of 74% of the total series studied, which justifies the trend equation
that the city of Bangui is well and truly located in the humid tropical zone. The year 2013 is considered the most deficient and wettest year in the time series studied, while 2008 is the most surplus year or the value of the series is above average (Figure 3).
3.4. Anomalies of Thermal Trends in Bangui, 2004 to 2015
The centered and reduced anomalies of the average thermal trends of Bangui, from 2004 to 2015 count 4 surplus years against 8 deficit years. The average annual temperature of our series is 26.27˚C (Figure 4).
![]()
Figure 2. Anomalies in annual rainfall trends in Bangui.
![]()
Figure 3. Anomalies of annual hygrometric indices in Bangui.
![]()
Figure 4. Centered and reduced anomalies of the average thermal trends.
3.5. Level of Vulnerability by Borough and Malaria
The distribution of cases by borough according to the level of vulnerability noted that the 8th borough had a very high level of vulnerability, followed by the 3rd and 6th borough with a high level of vulnerability, the 5th and 7th borough had a medium level of vulnerability, the 4th and 2nd borough had a low level of vulnerability, and the first borough had a very low level of vulnerability.
3.6. Climate Trends and Malaria Trends in Bangui
During the 12 years of the study, 236,166 children under the age of 5 were treated in the health facilities of RS7. The year 2015 had recorded the highest prevalence 15.56% (n = 36,768); followed by the year 2012 (10.2%; n = 24,066); 2013 (9.85%; n = 23,268), 2009 (9.46%; n = 22,324); 2011 (8.62%; n = 20,348); 2014 (8.34%; n = 19,685); 2010 (7.86%; n = 18,578); 2008 (7.42%; n = 17,501); 2007 (7.3%; n = 17,250). The lowest prevalence were noted in 2004, 2005 and 2006 respectively 4.97% (n = 11,755); 4.62% (n = 10,931) and 5.8% (n = 13,692). The pediatric university hospital of Bangui treated 30.62% (n = 72,318) of all malaria cases during the 12 years of the study, of which 68.43% (n = 49,488) were severe malaria cases and 31.56% (n = 22,830) simple malaria cases. The distribution of cases by year is shown in Figure 5.
During the study period, malaria infection was more recorded during the rainy season (May to October) with an incidence of 61.11% (n = 44,193) versus 38.89% (n = 28,125) for the dry season (November to April). The monthly peak in malaria incidence was observed at the end of the rainy season (September and October) with an incidence of 11.38% (n = 8236) cases and 9.28% (6715). The distribution of malaria incidence by month is shown in Figure 6.
During the twelve years of the study, among the 49,488 children under 5 years of age hospitalized at the CHUPB for severe malaria, 2357 died, i.e., a mortality rate of 4.76% (n = 2357) and 3.25% (2357/72,318) of all malaria cases managed at the CHUPB. This in-hospital mortality was 12.64% (n = 298) in 2004 – 11.67% (n = 275) in 2006 – 10.31% (n = 243) in 2007 – 9.93% (n = 234) in 2010 – 9.42% (n = 222) in 2011 – 8.61% (n = 203) in 2005 – 8.53% (n = 201) in 2008 – 8.36% (n = 197) in 2012 – 7.42% (n = 175) in 2009 – 6.66% (n = 157) in 2015 – 4.07% (n = 96) in 2014 et 2.38% (n = 56) in 2013. The average peak of deaths
![]()
Figure 5. Distribution of severe malaria and simple malaria by year in children < 5 years.
![]()
Figure 6. Distribution of malaria cases by month in Bangui.
among children under 5 years of age hospitalized at CHUPB during the study period was noted in September 12.21% (n = 288).
3.7. Correlation between Rainfall and Malaria in Children under 5 Years of Age in Bangui
The correlation coefficient between rainfall and malaria is 0.51. This correlation is positive and strong. The R2 is 0.2271, or 22.71%, indicating a statistically significant relationship between rainfall and malaria in Bangui (Figure 7).
3.8. Correlation between Humidity and Malaria in Bangui
The correlation coefficient between humidity and malaria morbidity R2 = 0.213 (statistically significant relationship between humidity and malaria) (Figure 8).
3.9. Level of Vulnerability by District and Malaria in Bangui
The distribution of malaria cases by arrondissement according to the level of vulnerability and the number of malaria cases recorded showed that the 8th borough with a very high level of vulnerability had the highest incidence of malaria, with 64,748 cases, followed by the 3rd and 6th Arrondissements with a high level of vulnerability, which recorded 51,590 cases and 33,101 cases of malaria respectively. The 5th and 7th Arrdt with medium vulnerability level recorded 23,147 cases and 20,136 cases. In the 4th and 2nd borough, the level of vulnerability was low and the number of malaria cases recorded was 16,684 and 15,358
![]()
Figure 7. Correlation between rainfall and malaria in children under 5 years old.
![]()
Figure 8. Correlation between humidity and malaria in children under 5 years old.
cases. Finally, the first district with 11,502 cases of malaria had a very low level of vulnerability.
4. Discussion
Malaria remains a major challenge in sub-Saharan Africa. It is the leading cause of morbidity and mortality in children, despite the great efforts made at the global level and by the governments of the countries concerned [12]. The risk of severe malaria is primarily for children who have not yet been infected (the disease is immunizing) and for travelers to endemic regions for the first time [12]. Debates on the explanatory factors of malaria and on control policies continue to grow, despite the work already done in various disciplines [13]. The means of prevention, control and even eradication are now well known. These include preventing the proliferation of the vectors of the disease in the living environment, protecting oneself from the bites of female Anopheles that promote the transmission of the pathogen to individuals, and taking appropriate antimalarial medication. Regular household use of long-lasting insecticide-treated nets and indoor residual spraying reduce malaria transmission by targeting adult mosquito vectors [12]. However, mosquito numbers can also be reduced through breeding site management, which targets mosquito larvae as they develop into adult insects in aquatic habitats. This can be accomplished by permanently or temporarily reducing the availability of larval habitats (habitat modification and habitat manipulation), or by adding chemicals to standing water that either kill larvae or inhibit their development [13]. In spite of the free distribution campaigns of mosquito nets, it seems that their use is not the only variable to be taken into account in the prevention of malaria, and this observation suggests the need to look for other determining variables in the explanation of malaria in children. A Cameroonian study has shown that the high use of impregnated mosquito nets by most households does not prevent a high occurrence of malaria in children under 5 years [12]. The authors of this study recommended that consideration be given to improving the living environment and educating households on the use of malaria preventive measures, such as how best to protect children outside of sleeping hours, and on the possibility of free access to these preventive measures for the entire vulnerable population [12]. Indeed, mechanisms remain to be understood in order to try to curb this major public health issue for sub-Saharan countries. In particular, it is necessary to find out how to overcome the resistance of mosquitoes to insecticides and the impact of climatic determinants and their challenges on vulnerable children in the city of Bangui. This question of the impact of climate change on malaria is at the heart of current public, scientific, political and economic debates given the importance of the problem [14] [15]. Climatic factors such as temperature and rainfall determine the presence and relative frequency of vector species [16] [17]. Climate change is already responsible for about 6% of malaria cases worldwide and in some middle-income countries [4] [14]. The emergence of adult Anopheles from breeding sites is the primary determinant of the presence and abundance of malaria vectors [18]. Without water, the life cycle of the mosquito would be interrupted. However, the water cycle is affected by climate change through the occurrence of extreme events such as floods and severe droughts [18]. During our study, the average annual temperature in Bangui from 2004 to 2015 was 26.27˚C versus 26˚C before 2004, which is an average temperature increase of about 0.27˚C in 12 years [19]. Furthermore, in our series, the average monthly umbrothermal diagram for Bangui shows that the amount of monthly rainfall evolves at the same rate as temperatures. These climatic factors (temperature and rainfall) are the key parameters determining malaria transmission. The increase in temperature in Bangui as observed in our series is in line with the Intergovernmental Panel on Climate Change, which estimates that the global temperature has risen by about 0.6˚C since the end of the 19th century [1]. This global warming in Bangui can be explained by the rapid urbanization of Bangui and the surrounding areas, which has increased the excessive consumption of firewood and charcoal as the main source of domestic energy [1]. This has led to a loss of biodiversity, atmospheric pollution and climatic disturbances, resulting in a rise in temperature [20] (Plate 1).
It should be noted that urbanization, as a social phenomenon and a physical transformation of landscapes, is the most powerful, irreversible and visible human transformation on earth [21]. The galloping urbanization in the world will be one of the great challenges of human well-being and a healthy living environment [22]. It leads to increased poverty, pollution, disease, political instability and social inequality in developing countries. This context shows the difficult relationship between population growth and spatial expansion in Bangui, as it

Plate 1. Deforestation in the Central African Republic.
raises the question of irrational occupation of the urban territory, which hinders the pleasant expansion of the city. It is in this context that Forbes magazine ranks Bangui 6th out of the 15 dirtiest cities on the African continent and 13th out of the 25 dirtiest cities in the world [23]. The lack of urban planning means that housing is built anarchically in these fragile areas or areas subject to water invasion and dramatizes. In these neighborhoods, a high population density (more than 200 inhabitants∙km2) leads to numerous problems, notably flooding due to rain runoff, poor access to drinking water and basic sanitation services (evacuation of domestic waste and human excreta), rainwater drainage, urban roads, etc. In addition, Bangui’s districts are essentially marshy and floodable [24]. The highest growth rates (68% to 87%) are noted in the 6th, 4th and 8th boroughs of Bangui, the average rate is recorded in the 5th (34%) and the lowest rates are noted in the 1st, 3rd, and 2nd boroughs (15% to 24%) [24]. The first group of districts (6th, 4th and 8th) is determined by strong demographic dynamics and refers to the densely populated peripheral neighborhoods was the most unhealthy of our series. The second district, distinguished by low demographic dynamics in urbanized neighborhoods, was less unhealthy. The living conditions of households in the 6th, 4th and 8th boroughs of Bangui, which have no infrastructure, are not satisfactory: use of polluted water from traditional wells; latrines are open pits; uncontrolled dumping of liquid and solid waste; dampness of swampy land; promiscuity, resulting in flooding (see Plate 2).
All of this uncontrolled urbanization coupled with abusive deforestation has contributed to global warming in the Central African Republic as evidenced by the results of this study. The increase in temperature and flooding in undeveloped districts has an impact on the malaria rate in children under 5 years old in Bangui. This is justified by a strong positive correlation coefficient between rainfall and malaria in our series with an r2 of 0.2271 indicating a statistically significant association between rainfall and malaria. The high rainfall in Bangui is a factor that promotes the development of malaria through the proliferation of larval sites. Moreover, during the 12 years of observation, malaria infection was more recorded during the rainy season with an incidence of 61.11% (n = 44,193) versus 38.89% (n = 28,125) for the dry season. Our results corroborate those of the study carried out in Abidjan by Eholié et al, who showed that 62% of malaria cases were recorded during the rainy season against 38% for the dry season [25]. Diallo et al. in a Senegalese study came to the same conclusion [26]. A Mauritanian
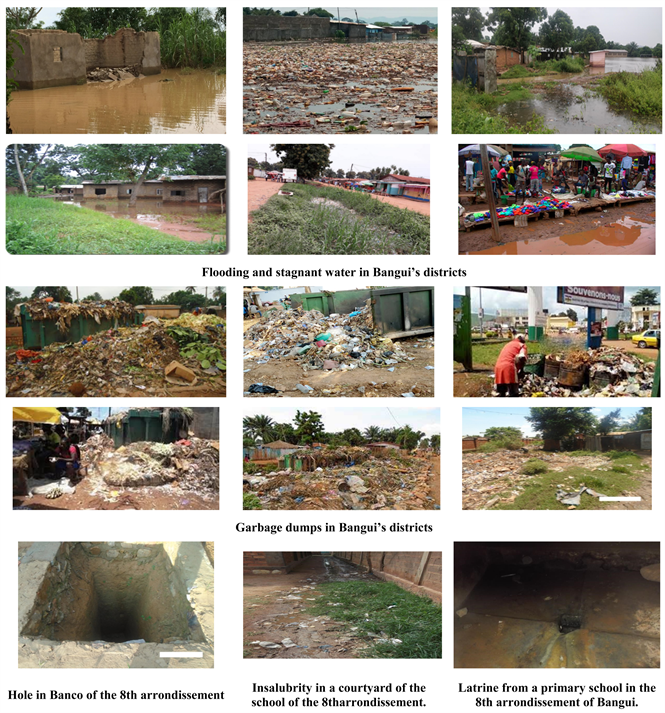
Plate 2. Illustration of the breeding grounds of the Bangui district (Source: Author 2019).
study carried out in 2019 noted results contrary to ours with a lower incidence in the rainy season. The authors explain this low incidence of malaria in the rainy season, compared to the dry season, by the absence of rainfall at the time of the investigation (late arrival of the rains compared to the season) [27]. In our study the presence of a slightly high incidence 7.50% (n = 5431) at the beginning of the dry season (November) could be explained by the “non-destruction” of the breeding sites by rain during the months of heavy rains, because the abundance of rainwater can sweep away the breeding sites. Kovasts et al. demonstrated that heavy rainfall would wash away mosquito eggs and larvae, thereby decreasing vector populations [28]. Global warming as described by Pascual in his study would increase mosquito numbers by more than ten times for each unit (1˚C) increase in temperature [3]. Another study conducted in Kenya, in 2015 by Githeko et al. showed that anomalies in climate variability were responsible for 26% of the anomalies in the number of hospitalizations [29]. This is because heat allows mosquitoes to grow faster, while humidity allows them to live longer and reproduce more [29] [30]. The correlation coefficient between humidity and malaria morbidity was 0.46 with r2 at 21.31% indicating a strong statistical link between humidity and malaria in Bangui. This correlation also reflects a moderate degree of dependence. In other words, malaria is influenced by humidity. By studying the seasonal occurrence of malaria in the Central African Republic and Bangui, it was concluded that the upsurge of malaria is related to the intensification of air humidity where water vapors are often saturated in clouds during rainy seasons. Our results corroborate those from Kenya, which showed that meteorological factors were associated with high malaria incidence, with temperature having the greatest effect with a direct correlation between increased temperature in the region and increased malaria cases [31]. On the other hand, in Benin, Houssou et al. showed that increasing the ambient temperature to 37˚C caused the death of plasmodiums in the body of the Anopheles and consequently a decrease in the number of malaria cases [32]. Our study noted that high levels of insalubrity in certain arrondissements of Bangui amplified malaria transmission among children under 5 years of age in Bangui. In fact, we found that the districts of Bangui with a high level of vulnerability had the highest malaria rates, such as the 8th district, which recorded the highest number of malaria cases (64.748 cases), as opposed to the first district with a very low level of vulnerability (1.1502 cases of malaria). This correlation between malaria and climate parameters at different lags highlighted in our series supports the findings of the study by Lindsay et al. who estimated that 260 to 320 million additional people will be affected by malaria by 2080 due to new transmission zones [33]. Some authors warn against attributing malaria dynamics to climate change alone and emphasize the uncertainties of malaria epidemiological forecasting at national and local levels [34]. Indeed, the difficulties in identifying, quantifying, and predicting the health effects of climate change relate to the characteristics of “exposure” and the development of often complex and indirect causal relationships operating at different spatio-temporal scales [35]. Data on the individual positivity and productivity of Anopheles larval sites only allow us to establish benchmarks for aquatic control, but without being able to predict future vector dynamics. Larval positivity does not always explain the abundance of mosquitoes because positive sites do not have the same capacity to produce adults [36]. Immature stages of mosquitoes are potentially important targets for vector control [37]. Source reduction through breeding site modification has been an important tool for malaria control in the United States, Israel, and Italy. The Sahelian drought, which has had a lasting effect on West Africa, has also been responsible for a decisive decline in malaria in West Africa [38]. The Central African Republic should address the larval breeding sites to reduce the incidence of malaria in children under 5 years of age. This study of the impact of climate on malaria transmission in Bangui has allowed us to highlight the key role of rainfall, which controls the risk of malaria through the distribution of water over the Central African territory. The results we have acquired allow us to propose practical recommendations for the environmental monitoring of malaria in the high-risk malaria transmission districts of Bangui, in a context of global climate change in general, and local climate change in particular.
5. Conclusion
The present study showed that the average annual temperature of Bangui increased by 0.27˚C between 2004 and 2015 with an average annual rainfall of 1545.8 mm of water. Statistical analyses showed that there was a statistically significant relationship between humidity and malaria. The same relationship existed between rainfall and malaria in Bangui. Thus, an increase in rainfall and/or temperature favored an increase in malaria cases among children under 5 years of age in Bangui. Ultimately, climatic trends have a negative impact on the evolution of malaria in Bangui. The consequences are a high number of malaria cases and related deaths in children under 5 years old. The role of the climate in the occurrence of malaria, which is characteristic of an annual evolution, has been demonstrated. This relationship between climate and malaria is far from causal and is also inherent in the unhealthy environmental conditions in Bangui. Efforts have been made but are insufficient to solve the malaria problem in Bangui. Therefore, malaria still remains a public health influence in Bangui.