Impact of Surgical Treatment of Patella Tendon Rupture Regarding Return to Sports in Yaounde ()
1. Introduction
Patella tendon rupture (PTR) is a solution of continuity of the patella tendon or an interruption of the extensor transmission chain of the leg against the thigh. It can be located at the body of the tendon, an avulsion of the tibia tuberosity, or a patella apex avulsion [1]. They represent about 5% of all lesions of the extensor apparatus [2]. It principally occurs in young athletes with a mean age of 39 years and with a male predominance (83%) [3] [4]. It can be associated with conditions such as gout, diabetes, corticosteroid infiltration, and certain chronic renal diseases [5] [6] [7] [8]. It is present clinically with pain, limited (or impossible) extension, patella alta is observed, active extension, and hemarthrosis [2]. It affects mostly athletes of outdoor games (44% volleyball players, 31% basketballers and 5% - 10% footballers) [9]. The carrier of athletes can be compromised. Surgery remains the goal standard and aims at rapidly restoring the function of the extensor apparatus and that of the entire limb [3]. The aim here is to obtain a solid repair that could permit the early start of the rehabilitation of the limb. Surgery is either by direct tendon suturing or transosseous re-insertion with/without reinforcement by a protection band wire.
The use of a protection band wire by many orthopaedic surgeons permits patients to obtain a solid suture, early mobilization, and an elevated rate of return to sports to a similar level of sporting activity. Similar findings can be gotten from Boublick et al. in 2011 in the USA, and Béranger et al. in 2020 in France who had a return to sports rate of 100% and 95% respectively [2] [10]. In a resource-limited setting like in our context, the use of a protection band wire obliges the patient to undergo a second surgery for band wire removal. This is why we decided to develop in our service, a tendon suturing technique associated with the placement of a rigid removable knee brace. These permitted tendon healing and return to sports in an adequate time.
The scarcity of studies regarding this topic in Africa motivated us to carry out this study. The objective of this study was to evaluate walking and return to sports following surgical repair of a patella tendon and factors influencing them in resource-limited settings.
Our research hypothesis was that; the surgical repair of patella tendon rupture in athletes permits a quick return to sporting activities in an appropriate time frame.
2. Patients and Methods
1) Procedure
We carried out a retrospective cohort study with a descriptive and analytic pattern. This study was conducted in orthopaedic and trauma units of 3 Hospitals in Yaounde (General Hospital, Military Hospital, and Yaounde Emergency Centre). It was a 5-year study from January 2016 to April 2021.
Our study population was patients aged between 18 to 65 years who were operated on for a patella tendon rupture that occurred during sports. The diagnosis of PTR was made following lower limb extension deficit, patella alta with an underneath patella notch, and confirm by standard radiography of the knee (patella alta) and/or an ultrasound result.
We excluded patients with an anterior tibial tuberosity (ATT) avulsion, an associated fracture, a patella tendon rupture of more than 3 weeks, and patients who did not respond to a follow-up. Data collection was done in two steps. The first step was a retrospective phase. It was done by collecting records from the emergency unit, traumatology consultation room, and post-operative notes from the theatre, and hospitalisation unit. This information helped us to collect files of patients from the hospital archive and filled in questionnaires. In the prospective phase, patients were contacted by phone calls to report to the hospital for radio-clinical evaluation. Questionnaires were filled during this visit. The following parameters of the study were considered:
Epidemiology: Age, sex, profession, circumstances of occurrence of the accident, time to admission at the hospital, patient past history, type of sport, level of competition, sports performance before the injury.
Clinical: Past history of tendinopathy, comorbidities, the context of trauma, affected side, initial clinical findings, state of lesions, and associated lesions.
Therapeutic: Time to surgery, surgical technique, protection band wiring, immobilisation, physiotherapy, and healing.
Complications: Immediate and late complications.
2) Pre-operative findings and surgical techniques
The surgical technique varies with respect to the side of the lesion. When the rupture occurs at the body of the tendon, a lacing suturing technique using a vicryl® size 2 after resecting the non-viable tendon edges. However, for ruptures occurring at the patella apex, a U-trans osseous suture and lacing at the body of the tendon is made with Vicryl® size 2. The patellofemoral ligaments were repaired with similar sutures went it was torn. Surgical closure was done in two layers: the subcutaneous layer with a Vicryl® 2/0 and the skin with a non-absorbable Ethicon® 2/0. A suction drain was placed underneath. In the immediate post-operative period, a rigid knee splint was in place, and weight-bearing was authorised with a single forearm crush. Physiotherapy was initiated immediately and consisted of isometric contractions. Knee mobilisation was not authorised until the removal of the splint on the 60th day after surgery.
3) Post-operative evaluation
During the prospective phase, our target was to evaluate patients with PTR to determine the amount, the level, and the time to return to sporting activities. The evaluation was objective by measuring the level of satisfaction using the VISA-P functional score [11] and the LYSHOLM score [12]. The VISA-P functional score assessed return to sport or physical activities after surgery on the knee. The LYSHOLM score had as aim to assess knee function after knee surgery. During this objective evaluation, the clinical assessment aimed at finding: limping, muscle wasting, and ranges of movement. The radiologic aspect was aimed at assessing pre-operatively the Cathon and Deschamps index [13] which permits us to determine the position of the patella (high, normal, or low).
4) Statistical analysis
Data collected on data collection forms were introduced in Microsoft Excel 2016 and then imported and analysed using SPSS (Statistical Package for Social Sciences) software version 20.0. Results gotten were reported as tables and figures. Qualitative variables were represented in terms of proportions and frequencies. Quantitative variables were represented in terms of median and range. Ni In order to compare quantitative variables we used the Mann-Whitney-U test since these data were non-parametric. We used Chi-Square or Fisher exact test, for qualitative variables. We considered p < 0.05 to be statistically significant. Multivariate analysis by logistic regression could not be used to identify prognostic factors related to return to sport.
3. Results
1) Series
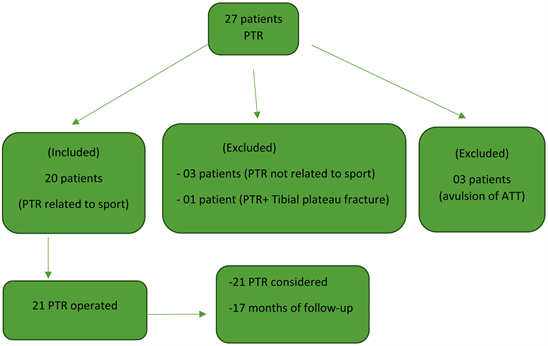
We had a total of twenty-seven patients who presented with patella tendon rupture. Seven patients did not respect the inclusion criteria. A total of twenty patients with 21 patella tendon ruptures were considered.
The median age was 36 years with ranges between 18 years and 63 years.
Sex: All patients were males (20 patients).
Level of education: Ten patients (50%) attended a secondary school as the highest level of education, 7 (35%) university, and 3 (15%) primary school.
Circumstances and mechanisms of injury: All injuries occurred during sports. The mechanism of injury was exclusively indirect by brutal contraction of the quadriceps, with a flexed knee while taking off or landing. While taking off during a jump in ten patients (50%), following landing during a jump in 9 patients (45%), and during a football kick in one patient (5%).
Type of sports practice: among the 21 ruptures related to sports, 9 (42.9%) occurred during a football match, 8 (38.1%) during a basketball match, 4 (19%) during other sports disciplines (Figure 1).
Level of competition: Fifteen (75%) practice recreational sports and (25%) patients practice professional sports.
2) Evaluation of return to sport
The proportion of return to sport was 85% (17 patients). This was noted while taking off. The median time to return to sport was 6 months (5 - 11 months) (Table 1).
The proportion of return to sport at a similar level of sporting activities was 45% (9 patients) within a median timing of 7.5 months (6 - 13 months).
Factors influencing return to sport
According to our results, low BMI was a factor influencing return to sport (p = 0.011) for patients who return to sports at the end of follow-up (Table 2). Whereas, age, past history of tendinopathies, and the use of a metallic protection band wire were not factors influencing the return to the sport. When comparing patients who returned to the sport and those who did not return to sport we discovered that there was no associative factor (Table 3).
![]()
Figure 1. Sporting activities practice and patella tendon rupture.
![]()
Table 2. Comparing return to sports with BMI and age (Mann-Whitney-U Test).
BMI: Body Mass Index.
![]()
Table 3. Presentation of factors associated to return to sports (Fisher exact test).
N = Number of cases; ATT = Anterior tibial tuberosity.
3) Evaluation of the functional results of patients
The median VISA-P functional score was 90/100 (25 - 100) and the median Lysholm score was 98/100 (40 - 100). The median range of movement for knee flexion was 120˚ (100 - 145).
The level of satisfaction was excellent for 6 (28.6%) patients, very good for 9 (42.9%) patients, good for 5 (23.8%) patients, and poor for 1 (4.8%) patient (Figure 2).
4) Radiologic analysis
Pre and post-operative radiographic analyses identified a modification in the
Caton and Deschamps index with a mean value changing from 1.2 (1.3 - 1.9) to 1.0 (0.8 - 1.1).
Pre-operative radiographs of two patients who presented mechanical pain at 6 months before trauma; one of them had signs of osteoarthritis type II of Sazaki.
5) Complications
Complications were found in 5 (25%) patients among which 2 (40%) patients had chronic pain, 2 others had quadriceps wasting (40%) and 1 patient (20%) had knee stiffness. Chronic knee pain was seen in a single patient who had osteoarthritis of the knee before PTR. There were no cases of infection nor rupture reoccurrence.
4. Discussion
The occurrence of tendon rupture during sport thrills us to evaluate their surgical repair together with their functional result and having as good index the return to sporting activities. This topic concerns the evaluation of various surgical techniques used to repair PTR related to sports over a period of 5 years in the town of Yaounde.
Out of this study, it is noted that return to sport in the town of Yaounde following surgery is effective at 6 months and has an elevated proportion as regards to literature. However, return to sport is influenced by BMI, but does not depend on the size, site of rupture or surgical technique. Studies with a wider sample size could clarify and better assess these variables.
We had a series of 20 patients with 21 PTR (one patient had bilateral PTR). All patients were male. Male predominance is seen in literature by several authors such as Beranger and Roudet, with a male predominance of 91% and 89% respectively [2] [10]. The median age was 36 years (18 - 63) which is relatively low as compared to Roudet et al. with 42.6 ± 9.9 years and Beranger et al. with 41.8 (24 - 68) with a total population ranging from 23 to 81 years [2] [14]. This difference could be due to the fact that the Cameroonian athletic population is mainly youths rather than old individuals who practice sporting activities at a similar baseline. Our study confirms that eccentric weight-bearing to the extension apparatus is the most frequent mechanism of PTE during sport (100% in our study). The result of El Anbari et al. is similar to 16 PTR related to sport; all caused by a similar mechanism. In addition, the study confirms PTR’s occurrence with patella tendinopathies [15]. A total of 66% of athletes in our study declared having patella tendinopathy symptoms before PTR.
The proportion of patients returning to sports after surgical repair of PTR at Yaounde was 85% within a median timeframe of 6 months after an assessment of over one and a half years. Our hypothesis was then confirmed. Surgical repair of PTR heals good results regarding the proportion and the time to return to sport what so ever the surgical technique used. This proportion is similar to that gotten by Roudet et al. in 2014 [1] and Jonathan D et al. in 2020 [16] who found proportions of 87% and 88.9% respectively. Better results were gotten from Boublick et al. with a 100% return to sports for athletes of high standard [6]. West et al. and Beranger et al. had a proportion of 100% and 95% respectively [2] [10] [17]. These could be explained by the fact that most of our study population practiced recreational sports (76%). It is well known that the level of training was described by many authors as an associated factor for early return to sport [2] [17].
The timing to return to sports varies from 6 to 12 months even thought is rare that they still practice at a similar competitive level [5] [18]. In our study, a period of 6 months was necessary to start running and 7.5 (6 - 15) months to return to sport at a similar level as before the injury. This is similar to the result of West et al. who reported a return to sport to a similar competitive level as before to be 100% at 6 months and a Lysholm score of 92 (Table 4).
Meanwhile, return to sports could also be influenced by other parameters like functional score, BMI, and age.
VISA-P functional score had a median value in our study to be 90 (25 - 100) and 98 (40 - 100) for the Lysholm score. The median knee flexion range of motion was 120˚ (100 - 145) which is instead good went comparing to those from the
literature. Boublik et al. identified for American footballers that there was a correlation between the timing to return to sport and the patient’s competitive level before rupture [10]. Patents of high competitive levels always return to sport rapidly. We could not assess this finding in our setting because most of our patients practiced a recreational sport. Other associated factors found in the literature were age (<40 years) and BMI < 25 Kg/m2; they ameliorate significantly VISA-P and Lysholm score [2]. The median BMI of our study was 26.8 Kg/m2 with ranges (23.7 - 31.6) Kg/m2. This is superior from that gotten by Roudet et al. (25.7 ± 2.66 kg/m2 (17.5 - 32.7)) and Béranger et al. (26.5 (21.8 - 36.3)). This difference could be the reason why the proportion of return is inferior in our study. In our study, we found a statistical significance between return to sports and low BMI (p = 0.011) as described by Béranger. Age was not an associated risk factor in our series. The absence of an association between various variables could be explained by the fact that the group of patients who returned to the sport was more than those who did not return to sport. Our small sample size could also be the cause.
Radiologic findings identified knee arthritis in one patient who had a past history of chronic pain. In fact, this patent had bilateral genu valgum before rupture. The patella was well placed following surgery (Caton et Deschamps index). This is different from certain authors who report a case of patella alta without any functional incidence on the patient [14] [17] [18] [19].
As concerns complications, we found chronic knee pain and wasting. This could be due to a prolonged immobilisation for 45 days before flexing the knee. This complication was reported by Siwek et al. [20] but it was a necessity to preserve our tendinous suture in our environment where physiotherapists are not always specialised.
After reporting that the distribution of PTR offers good results, this study bears the merits of haven analyse the surgical techniques and anatomical forms of the lesion. Nevertheless, it had some limitations; related to the small sample size and a retrospective study type.
5. Conclusions
Patella tendon rupture is a potentially disabling pathology for athletes because it alters the functional prognosis of the limb and hence their athletic carrier. Football is the main sport responsible for these ruptures in Yaounde.
Early surgical management associated with appropriate physiotherapy curbs the level of return to sports in our environment. The use of a removable knee brace rather than a metallic protection band wire is an interesting alternative in our context in the sense that, it is the patient who pays all hospital bills by himself. Therefore, leading to a return to sports at 85% for all patients and 53% for patients who could regain their initial level of sporting activity.