New Classification and Visual Analysis of the Patella Cartilage during Total Knee Replacement ()
1. Introduction
The management of the patellar articular surface at the time of primary total knee replacement (TKR) is controversial. According to many surgeons the main reason for not resurfacing was normal cartilage. The need of primary patellar resurfacing could be judged based on the intraoperative findings regarding the severity of patella femoral disease.
Commonly accepted indications for patellar resurfacing are rheumatoid arthritis, patellar cysts, Loss of congruence between the patella and prosthesis design and severity deformity.
Femoropatellar osteoarthritis is commonly diagnosed and monitored with radiography. The reliability of radiographic classification systems is poor or moderate. The preoperative radiographs underestimate the severity of knee osteoarthritis.
Arthroscopy is considered the most valid method for evaluation of cartilage lesions but the best way for grading, measure and dimension is direct visualisation. The true extent of articular cartilage damage can be better appreciated intraoperatively.
The aim of this prospective study is to evaluate how much damage the patellar cartilage presents during a total knee replacement.
2. Methods
After the ethics committee approved this study, we examined 320 patients between January 2019 and December 2020 who submitted to a TKR. As 34 patients underwent these procedures bilaterally, we collected data for 354 primary TKRs. All patients in the study had a primary diagnosis of osteoarthritis.
All cases of revision knee replacement, previous bone surgery around the knee and infection history were excluded. In all cases, we used prevision surgery images: plain standardised radiographs were taken in the following views: anteroposterior, lateral and skyline of the patella.
A full-length weight-bearing roentgenogram of the lower extremity was also included.
During the surgical procedure, after exposure and eversion, damage to the articular surface of the patella was analysed by visual inspection and photographs.
The damage to the articular patellar surface was analysed macroscopically by the surgeon and three assistants, who consensually graded the degree of lesion in a new classification:
Group I: signs of softening or fibrillation of the patellar cartilage.
Group II: fissure and fragmentation of less 50% of the diameter of the patellar cartilage.
Group III: erosion exposing the subchondral bone of less than 50% of the diameter of the patellar cartilage.
Group IV: subchondral bone exposing more than 50% of the diameter of the patellar cartilage.
Group V: complete subchondral bone exposure, flattening or inversion of the patellar triangle.
In spite of cartilage damage, in no cases did we replace the patella.
When necessary, osteophyte resection was achieved for articular surface regularisation and anatomical reestablishment.
Electrocautery denervation of the edges was performed circumferentially in all cases [1] [2] [3] [4].
The age of the patients ranged from 50 to 93 years, with a mean and standard deviation of 70.7 ± 7.6 years.
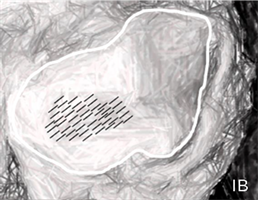

Group I. Signs of softening or fibrilation of the cartilage. (IA) Photograph of the patelar cartilage damage (Group I); (IB) Schematic drawing showing cartilage fribilation.

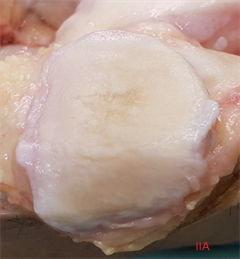
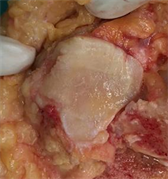

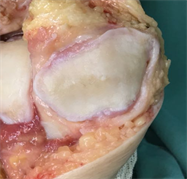
Group II. Fissure and fragmentation without subcondral bone exposing. (IIA) Photograph of the patelar cartilage damage (Group II); (IIB) Schematic drawing showing cartilage fragmentation. Three photos of different cases belonging to the Group II showing fissure and fragmentation without subcondral bone exposing.




Group III. Erosion exposing the suchondral bone of less than 50% of the diameter of the cartilage. (IIIA) Photograph of the patelar cartilage damage (Group III); (IIIB) Schematic drawing showing erosion exposing subcondral bone less than 50% of the diameter of the cartilage; Three fotos belonging of Group III showing differents lesions less than 50%.
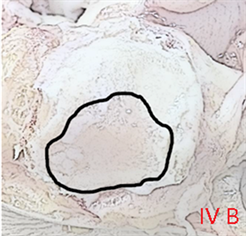
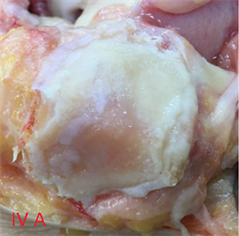



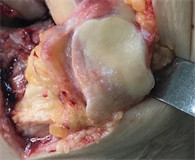
Group IV. Subchondral bone exposing more than 50% of the diameter of the patellar cartilage. (IVA) Photograph of the patelar cartilage damage (Group IV); (IVB) Schematic drawing showing subchondral bone exposing more than 50% of the diameter of patellar cartilage. Three fotos belonging of Group IV showing differents lesions more than 50% of the diameter of patellar cartilage.
In total, 251 patients (78.5%) were female and 69 (21.5%) were male.
The right knee was compromised in 193 cases (54.5%) and the left knee in 161 (45.5%).
The body mass index (BMI) ranged from 18.2 to 50.4 kg/m2 with a mean of 30.5 ± 4.7 kg/m2.
Only 34 cases (9.6%) were considered normal based on BMI (18 - 24.9 kg/m2).
BMI data were: overweight (25 - 29.9 kg/m2) in 136 cases (38.4%), obese (30 - 34.9 kg/m2) in 134 cases (37.8%) and severely obese (>35 kg/m2) in 50 cases (14.2%).
To radiographically grade osteoarthritis, the Kellgren–Lawrence scale was used [5].

![]()
![]()
![]()
![]()
Group V. Complete subchondral bone exposure, flattening or inversion of the patellar triangle. (VA) Photograph of the patellar cartilage damage (Group V); (VB) Schematic drawing showing complete subchondral bone exposure. Three fotos belonging of Group V: showing complete disappearance of patellar cartilage.
No knees were classified as grade I or II, but 35 were considered grade III (9.8%) and 319 were grade IV (90.2%).
For the measurement of axial deviation, the method described by Hsu et al. [6] was used.
Only 3 cases were considered norm axis (0.8%), 95 had genu-valgus (26.8%) and 256 had genu-varus (72.4%).
Mean valgus deviation was 15.6˚ ± 5.1˚.
Mean varus deviation was 10.1˚ ± 4.8˚.
When 354 articular patellar surfaces were analysed according to this classification, we found the following distribution: Group I: 2 cases (0.6%); Group II: 23 cases (6.5%); Group III: 55 cases (15.5%); Group IV: 175 cases (49.4%); and Group V: 99 cases (28.0%).
When we divided cases into 2 groups according to subchondral bone exposure: Groups I-III (exposure subchondral bone less than 50% of cartilage diameter) included 80 cases (22.6%) and while Group IV and Group V (exposure more than 50%) accounted for 274 cases (77.4%).
Statistical analysis was performed using SPSS (version 21) and Fisher’s exact test and Spearman’s correlation coefficient where necessary.
Sociodemographic and clinical characteristics are summarized in Table 1.
3. Results
We found patellar cartilage damage in all cases where a total knee replacement was performed (354/354).
There was no evidence of an association between patellar arthrosis and gender (p = 0.896).
![]()
Table 1. Sociodemographic and clinical characteristics.
There was no evidence of an association between patellar arthrosis and side (p = 0.850).
For the analysis of age, weight and deformity, cases were divided into two groups: less severe (80/354) (Groups I-III) and more severe (Group IV and Group V) (274/354). In the second group, there was more than 50% of the subchondral bone exposed.
Spearman’s correlation coefficient did not show any correlation between age and grade of arthrosis (p = 0.318).
The same was true when divided into groups: mean age of the lower severity group (70.5 years) and higher severity group (71.5 years).
When analysing all 354 knees, there was no evidence of an association between weight and arthrosis (p = 0.207); however, we found a significant correlation between obesity (BMI > 30) and more severe cases (p = 0.021) (184/354).
When analysing arthrosis with deformity in two groups, we found of more severe cases, 201/256 (78.5%) were varus and 77/95 (76.8%) were valgus.
No statistical association was found (p = 0177).
4. Discussion
Osteoarthritis of the knee affects millions of people worldwide. It is a disabling disease resulting in pain, diminished function, and restricted motion.
The diagnosis and monitoring were performed by radiographic, tomography and magnetic resonance imaging.
Many radiographic classification systems were used in an attempt to confirm articular degenerative cartilage lesion with reliability.
The most widely used system for osteoarthritic knees are: kellgren-Lawrence [5], Ahlbäck [7], Fairbank [8], Brandt [9] and IKDC (international knee documentation committee) [10].
For analysis of only the femoropatellar joint, the Iwano [11] and Merchant [12] systems are the most commonly used.
Until now, none of the studied osteoarthritis grade classifications showed acceptable reliability [13] - [21].
The most commonly used scale for femoropatellar evaluation is the Outerbridge classification [22]. This is very simplistic and unrealistic because the worst grade (IV) only reported the subchondral bone being exposed.
Analysing this correlation with cartilage status assessed arthroscopically, they show only poor and moderate interobserver reliability [23] - [33].
Cameron [34], in a cadaver-based study, concluded: “the Outerbridge classification was moderately accurate when used to grade chondral lesions arthroscopically”. Brismar [35], in a videotape study, concluded: “the arthroscopic grading of early osteoarthritic lesions in inexact”. Razak [36] found a weak correlation between radiographic and arthroscopic findings in Asian osteoarthritic knees. Spahn [37], in a multicentre survey with 301 highly experienced arthroscopists, concluded that arthroscopy was not perceived to be as reliable as a “gold standard” for the diagnosis of cartilage lesions.
Replacement or non-replacement the patellar joint during total knee replacement remains controversial [38] [39] [40] [41] [42]. This new classification could help orthopaedic clinicians with their decision.
In this study, we found patellar cartilage lesions in all patients. Only 25 (7.1%) were free of subchondral bone exposure.
In 329 (92.0%), the subchondral bone was exposed to different degrees. In 274 (77.4%), from Group IV and Group V, there was more than 50% of the subchondral bone exposed. This means that three in four patients have severe cartilage lesions. Should there be a replacement?
In 2019, we published a similar classification with 6 groups, but this has now been decreased to five [43].
Kijowski [44] correlated the radiographic findings of osteoarthritis and the arthroscopic findings of articular cartilage degeneration within the patella-femoral joint. They analysed the sensitivity for the presence of osteophytes, joint-space narrowing, subchondral sclerosis and subchondral cysts. The conclusion was that “marginal osteophytes were the most sensitive radiographic feature for the detection of articular degeneration”. Osteoarthritis rarely occurred in the absence of osteophyte formation.
For this reason, in the past we included osteophyte formation in the classification. When trying to reproduce interobserver reliability testing in our orthopaedic staff and residents, the presence of osteophytes was confusing and debatable. For this reason, we now only need to know the status of the cartilage.
No relationship was found between the degree of arthrosis and gender, side, age, or deformity.
In the last paper published [43] analysing 176 total knee arthroplasties, we found an association between varus deformity and patellar arthrosis (p = 0.019); the same was only seen for BMI (p = 0.010). In the present study, we only found statistical correlation in patients with a higher BMI (30 kg/m2) and more severe cases (Group IV and Group V).
5. Conclusion
By visually analysing and photographing 354 patellar articular surfaces trans- operatively, using this classification, we concluded:
1) Articular cartilage was damaged in all cases (100%).
2) Important subchondral bone exposure (more than 50% of the patellar articular surface diameter) occurred in 274 knees (77.4%) in Group IV and Group V.
3) Obese patients (BMI higher than 30 kg/m2) had more severe patellar osteoarthritis (Group IV and Group V). Obesity is an important risk factor of patellofemoral arthrosis.