Mechanical Eye Trauma Epidemiology, Prognostic Factors, and Management Controversies—An Update ()
1. Introduction
Ocular trauma is a common, preventable cause of visual impairment. From developing to developed countries, eye injury causes a social burden to the community. The treating of eye injuries is both problematic and debatable [1]. There are controversies regarding classification system, treatment plan, management complication, need for multiple surgeries etc. when it comes to ocular trauma. The Beaver Dam Eye Study finds that the lifetime frequency of ocular trauma is 14.4 - 19.8 per cent [2]. Mechanical eye injuries affect the eye in many ways ranging from mild to severe morbidity. The burden of blindness is related to both its unavoidable impact on quality of life and the subsequent loss of production in these persons. Ocular trauma affects up to 6 million children worldwide each year, with a quarter-million requiring hospitalization [3]. The causative factors are widely variable and have a direct impact on visual outcome. Several questions like cause of the trauma, extent of the trauma, initial visual acuity, time of starting treatment, need of multiple surgery, association of endophthalmitis, counselling and realistic outcome of the management will be discussed. The management of ocular injuries in the paediatric age group differs significantly from adults. Over the last 30 years, developments in our understanding of the pathogenesis and management of ocular trauma, together with advances in ocular surgery apparatus and procedures, have enhanced the success of the final visual outcome. Mechanical eye injuries have a deep impact on the patient’s life as well as to the family and society. But it can be avoidable with social awareness and some protective measure. This review article will focus on the measure, that should be taken to avoid mechanical eye trauma, and we believe it will give the trauma surgeons overall guidance.
2. Methods of Literature Search
The following flow chart in Figure 1 explains the literature review process.
3. Epidemiology of Ocular Trauma
There is a wide range of demographic variations in the epidemiology of ocular
trauma. The mean age is in between the second to the fourth decade [4] [5]. The highest rate of eye trauma is between 15 - 20 years. (11.5 per cent) [6]. Males were more prone to injuries than females mentioned by different authors 84.6% [5], 74% [6] and 87.6% [7]. It is a primary cause of monocular blindness, accounting for approximately 60% of cases, particularly among children. [8] [9] [10]. Open globe injuries (OGI) are more common than closed globe injuries (CGI), with a proportion of approximately 60% vs 40% [3] [11] [12]. Sharp items were responsible for more than half of all injuries. The most prevalent cause was work-related injuries, followed by falls [10]. For children, the most prevalent location of the injury is the home [13]. Penetrating corneal injury was the most common type among open globe injuries, followed by rupture globe, perforation, and Intra-ocular foreign body [11] [14]. Among the closed globe injuries, contusion was most common, followed by laceration [14] [15].
4. Clinical Classification of Mechanical Trauma of the Eye
Open globe injury (OGI) and closed globe injury (CGI) are two types of mechanical eye injuries (CGI). Birmingham Eye Trauma Terminology (BETT) is a widely used ocular trauma terminology system. It provides a precise definition for each injury type and a comprehensive framework for the injury type (Table 1 & Box 1). Although BETT exclusively addresses mechanical ocular injuries [15] in terms of OGI, but avoids any ambiguity in communication. As a result, BETT cannot classify orbital and ocular adnexa injuries, and various categorization systems have been proposed [15]. Grant and colleagues demonstrated the importance of lid and adnexal laceration in predicting the ultimate visual outcome in the Classification and Regression Tree analysis model (CART) [16]. Agrawal et al. [16] also recommended to include orbital and adnexal trauma. They suggested that anatomical landmarks such as the spiral of Tillux or the annulus of Zinn can be used to separate two zones and be included in future prognostic models [1] [17].
![]()
Table 1. The terminology used in BETT.
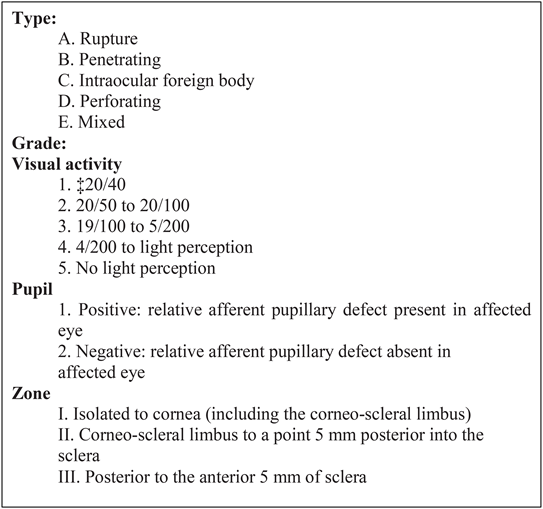
Box 1. Open globe injury classification.
5. Causology
There are several causative factors responsible for mechanical eye trauma. Among them, road traffic accident (RTA) is commonest in adult [18]. Sports-related injury is more common in children [19]. Other common causes are occupational injury, chemical burn, bomb blast, particle related injury, especially iron particle, blow to the eye like stone, fist or stick.
6. Prognostic Indicators for Ultimate Visual Outcome
The CART (Figure 2) [15] [16] and the ocular trauma score (OTS) (Table 2)
![]()
Figure 2. Classification and regression tree model for open globe injury: visual survival (light perception or better) vs no visual survival. H.M.: Hand moment; L.P.: Light perception; NPL: No light perception; RAPD: Relative afferent pupillary defect.
![]()
Table 2. Summation of raw points of ocular trauma score (OTS).
[18] are two techniques for determining future visual prognosis following OGI.
The Ocular Trauma Classification Group defines wound location [20]. The OTS is computed by allocating numerical raw points to six variables: initial vision, an RAPD, perforating injury, rupture globe, endophthalmitis, and retinal detachment. These six prognostic factors are significantly related to the final visual outcome. The ratings are divided into five groups based on the likelihood of achieving a range of post-injury visual acuities (Table 2). The higher the OTS score, the more favourable the prognosis. The existence of an RAPD and poor initial visual acuity is the most predictive of vision loss in the CART classification tree; the presence of a laceration on the lid and the posterior position of the wound further predicted a poor visual outcome. According to Wai and Steel [19], while comparing OTS and CART models in the Management of OGI, the OTS had superior predictive accuracy. OTS is a helpful tool for patient counselling and care [21]. OTS has been verified in various series [16] and provides trauma patients and families with evidence-based predictive outcomes. On the U.S. Eye Injury website, one may also compute the OTS score [22].
7. Initial Evaluation of Ocular Trauma
7.1. History
The processes, timing, and circumstances surrounding the injury should be meticulously documented, as they may become essential pieces of medicolegal evidence in the future. Any history of treatment, including medicine, surgery, or amblyopia, should be recorded. Type, place, timing, causative factors of the injury should be evaluated.
7.2. Systemic Evaluation
Any life-threatening damage should be ruled out before approaching any patient with ocular trauma in emergency settings. Basic and advanced life support are the primary goals in severe injuries until the patient’s stabilization. Any defect in the pupil needs a complete evaluation of the posterior segment, including the retina, choroid, and optic nerve. Eyeshield should be placed over the eye immediately, and any pressure or eye drop should be avoided. Tetanus toxoid is recommended to prevent tetanus.
7.3. Assessment of Vision
The visual status of the patient should be recorded in each eye by a standard vision chart. Any counting finger, hand movement, accurate projection in all quadrants, and perception of light (P.L.) should be appropriately recorded. The absence of light perception is not an indication for enucleation, and the globe may be salvageable [23].
7.4. Preoperative Ophthalmic Evaluation
Firstly, a thorough assessment of the mechanical injury is done. The primary management needs a complete ophthalmic examination, emphasizing the possibility of eye penetration and incorporating gonioscopy and dilated fundoscopy [24]. If the study of the globe is challenging, computed tomography (C.T) can help. Due to management and medicolegal considerations, it is critical to record visual acuity as the initial step in approaching a patient with ocular damage. In all situations, photographic evidence or a diagrammatic depiction of the kind and degree of the damage should be made (Figure 3). Mechanical OGI should be classified according to the international classification system [20] to prevent further ambiguity among the team. An anaesthetic examination is recommended to rule out globe disintegrate when OGI is suspected, but a thorough examination is not feasible (e.g., pediatric trauma).
8. Ophthalmic Manifestations of Ocular Trauma
1) Eye Lid and Adnexa: Edema, ecchymosis, and panda eyes, laceration, canaliculi injury and lid margin involvement
2) Extraocular muscle: Ocular motility should be tested in all positions of gaze in suspected orbital or cranial nerve injury with caution.
3) Orbit: Proptosis or enophthalmos. Crepitus on palpation, discomfort on palpation of bony orbital edge to rule out an orbital fracture. In pediatric orbital trauma, white eye orbital fracture should be checked carefully.
4) Conjunctiva: Injection, chemosis, haemorrhage, emphysema, pigmentation suggestive of uveal tissue involvement.
5) Cornea: Penetrating corneal injury with an extension of the wound, iris/ uveal prolapse, IOFB. In suspected self-sealing wounds, Siedel’s test is recommended.
6) Limbus: It acts as a landmark. Limbus can be involved in the lacerated injury of cornea, or sclera or sclera-corneal injury as well.
7) Sclera: Rupture globe or penetrating scleral injury with or without posterior extension, prolapse of intraocular content like choroid, vitreous, retinal etc.
8) Anterior chamber (A.C.): Depth of A.C., cells, hyphema, hypopyon, fibrin, membrane, lens particle, vitreous, IOFB.
9) Iris: Sphincter tear, iridodialysis, iris prolapse with loss of viability, aniridia,
![]()
Figure 3. Pictorial demonstration of corneal injury.
angle recession, cyclodialysis cleft, iritis, iris atrophy, short miosis, traumatic dilatation of the pupil.
10) Crystalline Lens: Traumatic cataract, anterior capsule injury, posterior capsule rupture (PCR), zonular dehiscence, subluxation, dislocation, Vossius ring.
11) Vitreous: Haemorrhage, posterior vitreous detachment, IOFB
12) Retina: Retinal tear, subhyaloid or intraretinal haemorrhage, IOFB, retinal detachment, choroidal detachment, choroidal rupture, macular hole, Berlin’s oedema, traumatic endophthalmitis.
13) Intraocular pressure (IOP): IOP should be checked by non-contact tonometry in all cases if the patient allows it. It should not, however, be done if a globe rupture is suspected
14) Gonioscopy: In all trauma cases, a gonioscopy should be performed, especially following the absorption of hyphema, to check any angle recession or IOFB or pigmentation. It should not be attempted in cases when OGI is suspected.
9. Role of Imaging in the Management of Ocular Trauma
Radiography, ultrasonography (USG), MRI, and C.T. are all widely used imaging technologies for the orbit and eye. In cloudy media, B-scan USG can be highly effective. In OGI, a gentle B Scan is recommended. C.T. Scan is commonly used in pinpointing the exact location of an IOFB or orbital damage. Zhang et al. [25] reported that C.T. could fail to detect metal fragments <0.5 mm. If a metallic intraocular or intraorbital foreign body is suspected, an MRI is not recommended.
10. The Management Approach for Mechanical Eye Trauma
The fundamental goal of primary globe repair is to restore anatomical integrity while optimizing visual potential.
The four-pronged method for open-world injury management should include general principles for risk avoidance and outcome optimization.
1) Reduce the risk of further trauma;
2) Reduce the risk of infection;
3) Reduce the trauma victim’s and his family’s psychological trauma and
4) Control the legal problems.
11. Preoperative Planning
11.1. Surgery Timetable
Unless prohibited by any other medical condition, primary globe repair should be performed as soon as possible, preferably within the first 24 hours.
11.2. Consent and Counseling
The ophthalmologist must adequately inform the patient and family about the status of the eye, the surgical plan, costing and its complications. This should include that multiple surgeries may be needed, and primary repair is only the first step. The patient should be told of the OGI’s guarded prognosis before surgery to ensure reasonable expectations.
11.3. Anaesthesia
Although the choice of anaesthetic medication, particularly in OGI, is debatable, general anaesthesia is advised for ocular injuries. We have performed repair under peribulbar anaesthesia in our unpublished data, with an excellent postoperative outcome (Figure 4).
12. Surgical Approach of Mechanical Trauma
12.1. Exposure of the Eye
The eye should be adequately exposed. If lid damage or a periorbital hematoma is hampering the view, it should be addressed initially.
12.2. Cornea & Sclera
Foreign debris and membrane should be removed during the initial exploratory operation. 360 degree conjunctival peritomy is ideal. Peroperative assessment of the injury with extension and meticulous planning is essential. Limbus should be secured first, followed by sclera and cornea. Usually, 10-0 monofilament Nylon is used for cornea, 8-0 Vicryl for sclera and 8-0 silk for conjunctiva. Corneal sutures should be placed radially and neither be too tight to distort the cornea nor too loose, leading to wound dehiscence. Corneal sutures should be shorter in the centre of the cornea than in the peripheral cornea (Figure 5). Experienced surgeons should perform the repair to reduce the mal handling of the delicate cornea and optimize the outcome. Stellate corneal laceration should be repaired using purse-string sutures.
Scleral wounds that extend beyond the rectus insertion are healed as far back
![]()
![]()
Figure 4. Preoperative and Postoperative picture of penetrating corneal injury repair performed under local anaesthesia.
![]()
Figure 5. Diagram of corneal laceration repair with different suture lengths in the centre and mid-periphery.
as feasible. The margin should be free of any uveal tissue. Any prolapsing vitreous should be cleared by anterior vitrectomy to avoid traction on the vitreous and retina.
12.3. Iris
If the iris is viable, should try to preserve it as much as possible. In lacerated iris, pupilloplasty may be needed. In the case of irido-dialysis, a repair can be done by swing technique or modified McCalan suture.
12.4. Lens
Traumatic cataracts can develop due to a breach in the capsule or perforating injury. Zonular dehiscence, anterior and posterior capsular tear, subluxation or dislocation may further compromise the lens status. Cataract extraction with simultaneous repair of the penetrating injury and IOL implantation has been widely recommended [26]. IOL may be inserted in the first sitting, or secondary IOL can be given later on. Biometry of the better eye is widely established in case traumatic eye [27]. Postoperative visual outcome following traumatic cataract correction revealed 31% of eyes had a visual acuity > 20/40, and 61.0 per cent had a visual acuity > 20/200, according to Shah et al. [10] [26]. The secondary IOL implantation and primary IOL implantation shoes similar visual outcomes [28], though secondary IOL implantation allows the affected eye time to heal and the surgeon more time to plan. A separate incision site is recommended for cataract extraction, and cataracts should never be extracted through the site of laceration.
12.5. Vitrectomy
Vitreoretinal surgical techniques allow many poor prognosis eyes to be salvaged [29]. Broadly, indications are R.D. with or without proliferative retinopathy (PVR), IOFB, lens-related problems and others. Scleral buckling also can be considered in traumatic R.D. without vitreous haemorrhage or PVR.
12.6. Intraocular Foreign Body
IOFB injuries are relatively complex eye emergencies, necessitating comprehensive treatments and often serial surgeries [30]. They cause mechanical injury along the track, carry infections, increasing the risk of endophthalmitis, toxic chemical reactions by the retained IOFB, especially with metal IOFBs. Early removal of IOFB is optimal to decrease the risk of endophthalmitis and PVR [31]. However, in a study by Colyer et al. [32], 54.0% of patients achieved good visual outcomes when the IOFB was removed after a median of 21 days after providing adequate cover with a combination of systemic and topical antibiotics.
12.7. Retinal Detachment
Traumatic R.D may occur due to retinal dialysis, flap tears, giant retinal tears, retinal necrosis. Eyes with trauma and retinal tear are at high risk of PVR and likely to undergo vitrectomy. It can be present at the time of injury or develop post-globe repair, and the incidence varies from 2.5% to 39% [33]. Longer wound length (>10 mm), vitreous prolapse, vitreous haemorrhage, rupture injury (vs laceration) and retained IOFB are other factors that cause retinal detachment.
12.8. Traumatic Hyphema
Traumatic hyphema involving more than half of the cornea may cause permanent vision loss due to blood-stained cornea or secondary glaucoma causing optic neuropathy. Reactionary bleeding could lead to permanent vision impairment, especially in patients with sickle cell trait/disease. Walton et al. [34] recommended routine use of topical cycloplegics and corticosteroids, systemic antifibrinolytic agents or corticosteroids and a rigid shield. They also recommend activity restriction (quiet ambulation) and interdiction of non-steroidal anti-inflammatory agents. The presence of corneal blood staining or severely elevated IOP after maximal tolerable medicinal treatment are indications for surgery.
12.9. Traumatic Optic Neuropathy
The optic nerve can be compromised either by direct compression due to inflammatory exudate and volume overload with the orbit or axonal swelling post-traumatic inflammation. Another mechanism can be the direct impingement of bony fragments within the optic canal. High dose steroids or orbital decompression is controversial in improving recovery compared with observation, and there are high rates of spontaneous recovery [35].
13. Management of Infection/Inflammation
13.1. Endophthalmitis
Post-traumatic endophthalmitis comprises 25% - 30% of all endophthalmitis cases, and it occurs in 3% - 10% [36] of patients after penetrating injury. This rate changes to 6% - 30% with the presence of an IOFB [37]. Early surgical repair and prophylactic systemic intravenous antibiotics for 48 h may reduce this incidence to <1% [32]. Risk factors include iron-related injuries, severely lacerated eye, retained IOFB, lens capsule injury, and delayed repair. The treatment comprises prompt recognition, intervention such as vitreous tap or vitrectomy followed by intravitreal injection of antibiotics (e.g., vancomycin plus ceftazidime) and systemic therapy [36]. There is a high incidence of retinal detachment (17% - 58%) and risk of phthisis in eyes with post-traumatic endophthalmitis.
13.2. Sympathetic Ophthalmia (SO)
The time from ocular injury to onset of SO varies greatly, ranging from a few days to decades. 80% of the cases occurred within three months after damage to the exciting eye and 90% within one year [38]. Cyclosporine, chlorambucil, cyclophosphamide or azathioprine may also be utilized if the inflammatory reaction cannot be adequately controlled with corticosteroids alone.
14. Postoperative Approach & Follow-Up
Postoperatively, a multidisciplinary approach to management and follow-up is essential for proper surgical rehabilitation of OGI patients [39]. A meticulous follow-up and documentation are necessary for the management of eyes with trauma. Recording of IOP, retina status and lens status and corneal sutures monitoring are all critical components in postoperative care of traumatized globe.
15. Medicolegal Issue
All the clinical and relevant findings and hospital visits should be well documented, timed and dated. This information may stand as substantial evidence in a court of law and in legal cases where compensations are granted against employers, other persons, etc. Proper documentation and decision were taken with the patient’s involvement in general to minimize the risk of future litigations against treating physicians.
16. Controversies Regarding the Management of Ocular Trauma
Ocular trauma is a matter of unsolved controversies, and management techniques for open-globe injuries are constantly changing. The international classification of ocular trauma is old and should be revised to calculate the outcome more precisely. Ocular adnexa and orbit should be involved in the classification. Covering the eye for corneal abrasion, corneal laceration repair, and therapeutic management of hyphema are all issues in anterior segment trauma. Cataract extraction and intraocular lens implantation in the aftermath of trauma are still being argued across the world.
Regarding posterior segment controversies, early versus late vitrectomy, preoperative application of cryotherapy and a scleral buckle, use of intravitreal antibiotic irrespective of infection, the utility of vitrectomy vs vitreous tap in the case of traumatic endophthalmitis are the issues. The significance of intravenous methylprednisolone in traumatic optic neuropathy is always debatable. The pediatric age group needs to be approached by a different protocol due to the risk of amblyopia, intraocular inflammation, and significant vitreoretinal adhesions. The discussion will give suggestions regarding the management of mechanical eye injuries based on existing published research and the writers’ personal experience.
17. Prevention and Protection of the Eye from Injury
According to studies and research, 90% of eye injuries are preventable [19]. Wearing safety glasses or goggles whenever you deal with chemicals or around the metal, glass, or other materials that could fly into your eyes is the safest way to safeguard your eyes. Squash and racquetball players must use eye protection. Protect your eyes with a shield affixed to your helmet if you play baseball or football. The children should be kept monitored. Sharp objects like pencils, pens, scissors should be kept away from the child. Because most eye injuries are preventable, emphasis needs to be placed on preventing rather than curing them. It is essential to raise public awareness about the benefits of wearing protective equipment, which is broadly accessible, which was the primary concern of most of the authors who reported on ocular trauma in the previous year.
18. Key Summarization
1) In ocular trauma, any life-threatening damage should be checked out first.
2) Determine visual acuity in both eyes with ocular injuries at the time of presentation.
3) Document all results legibly using clinical photos or diagrammatic depiction, as some instances may be medicolegal.
4) To avoid misunderstanding in communication, use the worldwide nomenclature and categorization system in ocular trauma eyes.
5) Because counselling is the mainstay of trauma patient care, physicians must provide patients with tools such as the ocular trauma score, which should be utilized regularly in conjunction with standardized nomenclature for ocular trauma.
6) In the management of complicated traumatized eyes, a devoted multidisciplinary team is required.
7) Globe injuries should be handled according to the broad principles of ocular trauma management, and surgical restoration of these eyes should follow the “atraumatic repair” approach.
19. Conclusion
Traumatic mechanical eye injuries can have substantial morphological and functional consequences on ocular tissue structures. Despite advances in diagnostic and surgical methods, globe rupture frequently results in vision loss. A thorough assessment and an appropriate technique are critical for successful treatment and preserving the final visual outcome.
Acknowledgements
We acknowledge Taskin Jamal, PhD. for his active support during the research.