Urinary Tract Infection among Adults Seeking Medicare at Kiambu Level 5 Hospital, Kenya: Prevalence, Diversity, Antimicrobial Susceptibility Profiles and Possible Risk Factors ()
1. Introduction
Urinary tract infections are still among the most prevalent extra-intestinal infections reported globally [1] [2]. Although these infections are not life-threatening, the high incidences significantly increase healthcare costs and negatively impact patients’ quality of life [3]. UTIs complicate the clinical welfare of affected patients and consequently create substantial economic and social burdens [4] [5] [6]. If not promptly diagnosed, left unattended or mis-diagnosed, the infections further lead to severe health impacts like renal damage. However, sound knowledge of UTIs and associated risk factors allow timely intervention to quickly bring the disease under control [7].
The prevalence of UTIs among adults varies, but globally females are more prone, with an estimated prevalence of about 25% being reported [8]. This has been attributed to women having a shorter urethra that is closer to the anal opening than men [9]. Other predisposing factors making women more prone to urinary tract infections are; voiding, wiping technique, wearing of tight pants or undergarments and vaginal douching [10]. The prevalence of UTIs among males aged under 50 years is low compared to that of adult women of the same age bracket, who are thirty more times likely to develop a UTI [11]. Evidence from previously conducted studies across the globe also ascertains that UTI prevalence rates vary widely because of different factors like: poverty, literacy, sanitation infrastructures that come into place [12]. For instance, a study in the USA that involved over 10.8 million patients reported a prevalence rate of 16.7% [13]. Almost similar prevalence rates (11.2%) were also reported in Asia [14] a clear indication that UTI prevalence rates differ across the globe. In Africa, related studies among adults have also revealed novel evidence that proves UTIs are an actual health burden [15] [16] [17] [18]. Recognizing these reported UTI prevalence trends and many more means that more research needs to be done to evaluate the prevalence, incidence and risk associated factors of urinary tract infections among adults.
The most prevalent etiological agents of urinary tract infections are bacteria [19]. This undeniable reality calls for more attentive investigations to understand and curb the menace. Among the bacteria known to cause UTIs, E. coli in particular has been documented to be the leading etiological agent [10] [20] [21]. Other Gram-negative bacteria that cause UTI include: Klebsiellapneumoniae, Proteus mirabilis and Pseudomonas aeruginosa [22]. Gram-positive bacteria that invade the urinary tract include:Staphylococcus,Streptococcus andEnterococcus species [23]. However, non-bacterial UTI etiological agents like Fungi, Viruses and Parasites have also been recorded in past related UTI studies [24]. Fundamentally, communities need to be enlightened on how to embrace all measures of UTI prevention and control. Furthermore, the larger spectrum of bacteriuria uropathogens and associated-risk factors remain under-investigated. Some of UTI risk factors reported in related studies include: Health conditions, Gender, Sexual activity, Pregnancy, Menopause, Age, Past history of UTI, Contraceptives and Social-economic status [12] [17].
Prompt UTI diagnosis and timely intervention is therefore very critical to halt pathogen establishment. Indeed, it is regrettable that most Kenyan health facilities that perform urine tests rely on rapid dipstick and direct wet microscopy urinalysis tests to diagnose UTI as they give immediate results and as such, urine culture is rarely done [25]. However, these tests have poor negative and positive predictive values to detect the presence of bacteriuria, especially in asymptomatic individuals [26]. Furthermore, the results of these tests are inadequate to inform the most probable drug of choice. Results of this study indicate that due to lack of microbial analysis, misdiagnosis may be a significant drive of UTI treatment failure. Again, considering that clinicians in most of these Kenyan facilities use empirical treatment to manage UTI. Prescription of antibiotics without relevant microbial findings, more so susceptibility patterns may be influencing the rising antimicrobial resistance. Culture and antimicrobial sensitivity tests are therefore the gold standard method of UTI diagnosis and as such should be embraced to inform management. However, innovation of new therapeutic breakthroughs and updating of the current UTI management policies is indispensable. This study’s main objective was therefore to investigate and determine the prevalence of bacterial urinary tract infection, antimicrobial susceptibility profiles, and UTI associated risk factors among adults attending Kiambu level 5 Hospital.
2. Materials and Methods
2.1. Study Design, Site and Ethical Approval
This cross-sectional study was done in Kiambu level 5 Hospital, Kenya. Study ethical approval was sought from the Kenyatta National Hospital-University of Nairobi ethical research committee (Reference no: KNH-ERC/A/470; Supplementary data S1) and National Commission for Science, Technology, and Innovation (NACOSTI) (Reference no: 619853; Supplementary data S2).
2.2. Sample Size and Sample Collection
A purposive sampling technique was applied to recruit patients until the study sample size of 206 was achieved. The sample size was determined using the formula by Lwanga and Lemeshow’s 1991 using a UTI prevalence rate of13.3% reported by Kabugo et al. 2016 [18].
N = 1.962 × PQ/D2
N = Desired minimal sample size.
Z = Standard normal deviation (1.96 from the tailed normal table).
P = Prevalence of the condition under study.
Q = 1 – P.
D = Precision required for the study at 95% confidence level (0.05).
Calculation of the sample size
P = 13.3Q = 1 − 0.133D = 0.05N = 1.962× PQ/D2
N = 1.962 × (0.133 × 0.867/0.052)
N = 177
However, two hundred and six (206) midstream urine samples were collected which are above the 177 required (206; women—77.6% & men—22.3%).
Using well-structured questionnaires, participants’ social demographic, clinical and lifestyle information was collected after giving consent to participate. Participants were given explicit instruction on the proper approach in collecting a midstream sample in a sterile collection tube [1] [27].
2.3. Urine Sample Analysis
2.3.1. Macroscopic, Dipstick and Microscopic Urine Analysis
All 206 participant’s urine samples were subjected to macroscopy observation to test various pathological parameters. Dipstick analysis using the 10-parameter chemical reagent urine strip and microscopic examination was performed as previously documented [15] [18]. Briefly, 10 ml of the urine sample was centrifuged at 2000 - 3000 rounds per minute (rpm) for 5 minutes. The supernatant after centrifugation was poured and a drop of the deposit placed on a glass microscope slide, covered with a cover slip and examined using a compound microscope (OLYMPUS CX23, JAPAN) under 10× objective len. This was followed by examination under 40× objectives. This was to determine the presence of pus cells, white blood cells, bacteria or yeast, casts, crystals and red blood cells in urine [28]. Any bacteria presence detected (1 - 4 per high power field) was considered as bacteriuria. In contrast, the presence of pus cells/leucocytes ≥ 10 in a single high-power field (HPF) was treated as pyuria case [15].
2.3.2. Bacterial Isolates Identification
1) Urine Culture
Urine culturing was done using previously established protocols [27]. Participant’s 5 µl urine samples that met the urine microscopy threshold of pus cells/leucocytes ≥10 in a single high-power field were cultured using surface streaking technique on Cysteine Lactose Electrolyte Deficient (CLED) and MacConkey agar plates (Oxoid, UK). The cultures were then aerobically incubated at 37˚C for 18 to 24 hours as done before [29]. Later the isolated cultures were subsequently sub-cultured on Mueller Hinton agar (Oxoid, UK) to obtain pure cultures that were used for Gram stain reaction and a series of biochemical test recommended for enteric and Staphylococcus species identification. Both the significant (≥105 CFU/mL) and the non-significant (≤105 CFU/mL) bacterial growth were concurrently investigated, and their profiles analysed. S. aureus (ATCC-25923), E. coli (ATCC-25922) and Pseudomonas aeruginosa (ATCC-27853) were used as quality control strains (QC). All protocols were done independently of each other as per previously used techniques [22] [27] [30].
2)Colony morphology
Though bacterial colony morphologies differ on various culture media, this study colonial morphology on CLED culture plates were determined based on; Pigmentation—color of the colony, Size—pinpoint, small, moderate, or large, Form—circular, irregular, or rhizoid, Elevation—flat, raised, convex, or umbonate and Margin—entire, lobate, undulate, serrate or, filamentous.S. aureus (ATCC-25923), E. coli (ATCC-25922) and Pseudomonas aeruginosa (ATCC-27853) were used as quality control strains (QC) (Supplementary data S3a, S3b, S3c). All protocols were done as per previously used techniques [22] [27] [30].
3).Colony forming units
Bacterial colonies on the primary CLED plate were counted to determine the yielded colony-forming units. Bacterial growth yielding colony-forming units of ≥100,000 CFU/ml (105) and above were assumed to have met the threshold/cut off point of UTI positive and were considered significant. Those yielding lower growth below ≤100,000 CFU/ml were deemed as non-significant growth/contaminants.
4) Gram staining
Gram staining was conducted prior to biochemical tests to classify and provide preliminary results of the isolates, this identified the isolates into either Gram-positive or negative by use of established protocol [19]. The prepared smears were left to air dry after staining awaiting observation under oil immersion (100×) using a compound microscope.S. aureus (ATCC-25923), E. coli (ATCC-25922) and Pseudomonas aeruginosa (ATCC-27853) were used as quality control strains (QC). Procedure was done as per previously used techniques [22] [27] [30].
5) Biochemical tests
Biochemical tests were conducted as per previously protocol to profile the isolates according to standard bacterial classification to the species level [31]. The following biochemical tests were performed; Sulfur Indole Motility, Urea utilization, Citrate utilization, Triple sugar iron, Catalase, and Coagulase test [32]. Standard reference strains: S. aureus (ATCC-25923) and E. coli (ATCC-25922) were included to validate the study findings. All these tests were carried out independently of each other.
2.4. Bioassays
Susceptibility Testing
Antimicrobial susceptibility testing of isolates was performed according to the Kirby-Bauer disc diffusion method [33] on Mueller Hinton agar (Oxoid, United Kingdom). Test drugs were antimicrobials routinely used in management of both Gram-positive and Gram-negative bacteria infections. They included Ampicillin (AMP 10 µg), Amoxicillin-clavulanic acid (AMC, 20/10 µg), Ceftriaxone (CRO, 30 µg), Nitrofurantoin (NIT, 300 µg), Gentamin (GEN, 10 µg), Cefoxitin (FOX, 30 µg), Erythromycin (ERY, 15 µg), Ciprofloxacin (CIP, 5 µg), Cefepime (FEP, 30 µg), Rifampicin (RIF, 15 µg), Nalidixic acid (NAL, 30 µg), Ceftazidime (CAZ, 30 µg), Cefotaxime (CTX, 30 µg), Sulfamethoxazole (SMX, 23.75 µg), Trimethoprim (TMP, 1.25 µg), Chloramphenicol (CHL, 30 µg), Tetracycline (TCY, 30 µg), Linezolid (LNZ, 30 µg), Vancomycin (VAN, 30 µg), Aztreonam (ATM, 30 µg). Comparable resistance patterns of the Gram-positive and Gram-negative isolates were done to determine the sensitivity trends against most of the study test antibiotics [34]. A double-disk synergy test to detect the likelihood of isolates carriage of ESBLs was performed using disks of 3rd generation Cephalosporins and Cephalosporin-inhibitor (Clavulanic acid) antimicrobial disk [35] [36].
All tests were done independently of each other. Standard reference Staphylococcus aureus (ATCC-25923), Escherichia coli (ATCC-25922) and Pseudomonas aeruginosa (ATCC-27853) were used as controls to ensure the potency performance of the antibiotic discs and the quality of the media was assured.
2.5. Data Analysis
The study UTI prevalence rate was determined by dividing UTI positive cases with the total number of urine cultures done and expressed as a percentage. Antimicrobial inhibition zones were interpreted using the clinical and laboratory standard institute (CLSI) standards and expressed as either sensitive(S), intermediate (I) or resistance (R) as documented before [35]. The study findings were later entered into excels spreadsheets for analysis using statistical package for social sciences (SPSS) version 15. Chi-square test analysis was applied to determine the association between socio-demographic factors and probable UTI risk associated factors. Binary logistic regression analysis was carried out to generate the adjusted odds ratio with a 95% confidence interval. An alpha of less than 0.05 (P < 0.05) was considered statistically significant.
3. Results
3.1. Study Population
The study involved adult patients seeking medicare at Kiambu level 5 Hospital; outpatient 174 (84.5%) and inpatient 32 (15.5%). The overall age mean among study participants was 31.8 years.
3.2. Bacterial Identification
Biochemical Tests Results
According to the study biochemical finding a variety of bacterial genera was responsible for UTI among the study population (Table 1). The commonest isolated bacteria was E. coli at (38.5%), followed by Staphylococcus aureus (21%) and Klebsiellapneumonia (19.3%) respectively. Other bacterial etiological agents isolated included:Proteus mirabilis (10.5%),Staphylococcus saprophyticus (8.7%) and Enterococcus faecalis (1.7%). Data among the non-significant growths revealed Staphylococcus aureus and E. coli as the most prevalent bacteria accounting for 24.1% each. Klebsiellapneumoniae and Enterococcus faecalis followed at 17.2%, and at 13.7% respectively. While Staphylococcus saprophyticus and Proteus mirabilis were the least isolated bacteria at 10.3% each.
3.3. Prevalence of Urinary Tract Infection
This study overall UTI prevalence was 27.6%. UTI prevalence rate based on department category revealed most cases from the outpatient department at 73.6% (42) to inpatient 26.3% (15). In addition, female participants in the out-patient department had 88.3% UTI positive cases to men 11.6%. However, a relatively high UTI prevalence rate was revealed among the female cohort attending antenatal clinic at 34% when matched to the rest of the outpatient sets of participants. In the inpatient department, a UTI prevalence rate of 66.6% (10/15) was revealed among women compared to men’s 33.3% (5/15). Even so, UTIs prevalence rates based on lifestyle factors and socio-demographic characteristics also seemed to heighten among the different sets of participants. The noted UTI prevalence rate amongst women participants of 80.7% was high than that amongst men of 19.2%.
![]()
Table 1. Biochemical test findings.
Key: positive test result (+), negative test result (−). E. coli ATCC-25922 used as Gram-negative control, S. aureus ATCC-25923 used as Gram-positive control.
Possible Lifestyle Factors and Socio-Demographic Characteristics
1)Urinary tract infections in relation to patients’age
Several possible lifestyle factors and socio-demographic characteristics were scrutinized to determine their association with UTI contraction. UTI occurrence among the study population based on age revealed participants between the ages of 18 to 50 years had a prevalence of 24.4% (43/176). This was lower when matched to that among participants within the age range of 21 - 30 years of 28.2%. However, those aged between the ages of 41 - 50 had the highest UTI prevalence rate of 42.9% compared to the rest of the age cohorts (Table 2).
![]()
Table 2. Urinary tract infections in relation to patients’ age
Key: Age in years; ≤18 - 20, 21 - 30, 31 - 40, 41 - 50, >50. Marital status as; single, married, divorced, widowed.
2)Urinary tract infections in relation to sexual activities
Sexual activities among the study participants were scrutinized to determine any relation with UTI occurrence. A urinary tract infection prevalence rate of 30.4% was revealed among participants with multiple sexual partners, higher than that of 27.6% among the cohort who had only one partner. Participants who had sexual intercourse more than twice weekly had UTI prevalence rate of 32.2%, almost double that of 16.2% reported among participants who had sexual activities once weekly. Nevertheless, participants with no partners at all had the least urinary tract prevalence rate at 21.1% (Table 3).
![]()
Table 3. Urinary tract infections in relation to sexual activities.
Key: Frequency of sexual activity on daily basis presented as; either once, twice, >2 and none. No. of sexual partners presented as; one, multiple or none.
3)Urinary tract infections in relation to personal hygiene
Finding on poor personal hygiene had some high UTI prevalence rates revealed. For instance, the prevalence rate of UTI in participants who changed their undergarments once daily was 29.4%, lower than that of 34% reported in the cohort that did change undergarments twice daily. But almost similar UTI prevalence finding was reported among participants who changed their sanitary towels twice daily during menses of 28.9%. It was only among women who changed their sanitary towels once daily during menses that a high UTI prevalence rate of 76.6% was noted (Table 4).
4)Urinary tract infections in relation to other demographic factors
Urinary tract infection occurrences based on education background revealed a prevalence rate of 43.5% among the set of participants with primary education background. That urinary tract infection prevalence rate is high if matched to that of 28.6% and 24.6% among participants’ with secondary and tertiary education backgrounds. The UTI prevalence rate among those with high blood pressure recording of 36.1% was also high than that of 25.1% amongst those with low blood pressure (Table 5).
3.4. Antimicrobial Susceptibility Profiles
3.4.1. Antimicrobial Susceptibility Profiles of Gram-Positives
Comparative analysis of Gram-positive antimicrobial resistance phenotypes from significant growths and non-significant growths unveiled resemblance. Staphylococcus aureus displayed resistance against Nitrofurantoin and Ceftriaxone at 18% and 29% respectively. The resistance of S. saprophyticus isolates against Ceftriaxone, Erythromycin and Ampicillin was at a range of 20% to 60%. However, considering resistance profile findings of the study Gram-positive isolates against Nalidixic acid, Sulfamethoxazole and Erythromycin at a range of 60% to 100%, then these drugs can no longer be used as drugs of choice for empirical treatment (Table 6).
3.4.2. Antimicrobial Susceptibility Profiles of Gram-Negatives
Gram-negatives isolates were the most prevalent, with Escherichia coli being the most frequent bacteria isolate. Although most Gram-negative isolates displayed resistance patterns, Escherichia coli isolates were exemplary, exhibiting antimicrobial and multidrug resistance trends. Most Gram-negative isolates had high resistances towards Sulfamethoxazole, Nalidixic acid and Ampicillin of 64%, 50% and 27% respectively. However, reassuring observation was that most of these Gram-negatives isolates still exhibited low resistance to Cefepime 9%, Cefoxitime 10% and Nitrofurantoin 14% suggesting that these drugs are still suitable for treatment. About 40% of Klebsiella pneumoniae and Proteus mirabilis isolates showed resistance patterns against Ampicillin at a range of 17% to 67%, Sulfurmethoxazole 40% to 80% and Nalidixic acid 60% to 100% respectively (Table 7).
![]()
Table 4. Urinary tract infections in relation to personal hygiene.
Key: Frequency of changing undergarments, frequency of taking a shower daily, frequency of changing sanitary towel during your menses presented as; either once, twice or > 2. Undergarment material presented as; either cotton or other fabrics.
![]()
Table 5. Urinary tract infections in relation to other demographic factors.
Key: Occupation presented as; either employed or unemployed. Education presented as; primary, secondary, tertiary or none. Blood pressure readings presented as; normal, high or low.
![]()
Table 6. Resistance profiles of Gram-negative isolated bacteria pathogens.
3.4.3. Resistance Profiles of Isolated Bacterial Pathogens Based on Department Category
Most of the bacteria isolates were obtained from the outpatient department 42/174 (73.7%) to inpatient 15/32 (26.3%). Resistance patterns based on department category revealed a 33% resistance trend by E.coli isolates from the inpatient against Ampicillin, Amoxicillin-clavulanic acid, Ciprofloxacin and Cefepime. In addition, Enterococcus species and S.saprophyticus isolates obtained from the outpatient department, exhibited relatively high resistance patterns towards Trimethoprim, Sulfamethoxazole and Nalidixic acid at range of 60% to 80% (Table 8).
![]()
Table 7. Resistance profiles of Gram-positive isolated bacteria pathogens.
Key: Antimicrobial susceptibility patterns of both significant and non-significant (contaminants) isolates from the study participants. The ranges to determine where the isolates were sensitive (S), intermediate (I) or resistance (R) were done as documented before [33]. Zero % (0%) means no resistance noted. Antibiotics routinely used in UTI management of both gram-positive and gram-negative bacteria: Ampicillin (AMP), Amoxicillin-clavulanic acid(AMC), Ceftriaxone (CRO), Nitrofurantoin (NIT), Gentamin (GEN), Cefoxitin (FOX), Erythromycin (ERY), Ciprofloxacin (CIP), Cefepime (FEP), Rifampicin (RIF), Nalidixic acid (NAL), Ceftazidime (CAZ), Cefotaxime (CTX), Sulfamethoxazole (SMX), Trimethoprim (TMP), Chloramphenicol (CHL), Tetracycline (TCY), Linezolid (LNZ), Vancomycin (VAN), Aztreonam (ATM).
![]()
Table 8. Resistance profiles of isolated bacteria pathogens based on department category.
Key: Antimicrobial susceptibility patterns of isolates from the study participants. The ranges to determine where the isolates were sensitive (S), intermediate (I) or resistance (R) were done as documented before [33]. Zero % (0%) means no resistance noted. Antibiotics routinely used in UTI management of both Gram-positive and Gram-negative bacteria: Ampicillin (AMP), Amoxicillin-clavulanic acid(AMC), Ceftriaxone (CRO), Nitrofurantoin (NIT), Gentamin (GEN), Cefoxitin (FOX), Erythromycin (ERY), Ciprofloxacin (CIP), Cefepime (FEP), Rifampicin (RIF), Nalidixic acid (NAL), Ceftazidime (CAZ), Cefotaxime (CTX), Sulfamethoxazole (SMX), Trimethoprim (TMP), Chloramphenicol (CHL), Tetracycline (TCY), Linezolid (LNZ), Vancomycin (VAN), Aztreonam (ATM).
3.4.4. Resistance Profiles of Isolated Bacterial Pathogens Based on Gender
Resistance patterns based on gender revealed that isolates obtained from the female gender exhibited drug and multi-drug resistance to most of the study drugs. For instance, the resistance patterns noted among E. coli isolates from the female cohort against Ampicillin, Ciprofloxacin and Nitrofurantoin were at a range of 20% to 40%. The obtained E. coli isolates among the male gender were all sensitive towards Amoxicillin-clavulanic acid, Ceftriaxone and Cefepime a complete opposite to E. coli isolates from the female gender that showed 20%, 24% and 20% resistance patterns respectively (Table 9).
4. Discussion
Urinary tract infections continue to be more prevalent in the hospital setting globally. In Africa, for instance, a study conducted at Okada in Nigeria reported an overall prevalence rate of 39.69% [15]. However, in this study the overall UTI prevalence rate was 27.6%, which is still high although falls within the global range of 13% - 33% [22], an almost similar UTI prevalence rate was also reported in Ismailia City, at 29% [2]. Even so, a more UTI prevalence variation of 90.1% was noted in a study conducted at Shashemene referral hospital, Ethiopia [15] an indication that these infections vary globally. Regionally at Mulago Hospital, Uganda, a UTI prevalence rate of 13.3% was reported [17]. Much of the same prevalence findings of 24%, was reported at the Aga Khan University Hospital, Nairobi, Kenya [18] and going by these aforementioned regional prevalence rates, there is a positive sign that implies that locally urinary tract infection management policies are moderately adhered to but the literature to enlighten the public domain is still limited. This study data analysis disclosed that majority
![]()
Table 9. Resistance profiles of isolated bacterial pathogens based on gender.
Key: Antimicrobial susceptibility patterns of isolates from the study participants. The ranges to determine where the isolates were sensitive (S), intermediate (I) or resistance (R) were done as documented before [33]. Zero % (0%) means no resistance noted. Antibiotics routinely used in UTI management of both Gram-positive and Gram-negative bacteria: Ampicillin (AMP), Amoxicillin-clavulanic acid (AMC), Ceftriaxone (CRO), Nitrofurantoin (NIT), Gentamin (GEN), Cefoxitin (FOX), Erythromycin (ERY), Ciprofloxacin (CIP), Cefepime (FEP), Rifampicin (RIF), Nalidixic acid (NAL), Ceftazidime (CAZ), Cefotaxime (CTX), Sulfamethoxazole (SMX), Trimethoprim (TMP), Chloramphenicol (CHL), Tetracycline (TCY), Linezolid (LNZ), Vancomycin (VAN), Aztreonam (ATM).
of UTIs cases were still among women at 80.7% compared to men 19.2%. The finding supports that females continue to be more vulnerable to contracting UTI due to their basic anatomy, whereby their urethra is closer to the anal opening and shorter than men’s [8] [10] [11] [22]. Again, women’s hormonal fluctuations across the menstrual cycle and the thought of a genetic factor that tends to run in families may also be fuelling their vulnerability [8] [20] [22] [27].
Further considerations of the reported urinary tract infection prevalence rates among the different participants’ cohorts suggested that UTI occurrences may be influenced by the various social demographic characteristics and life style factors that came into place (Tables 2-5). Past related studies have also reported different factors that seem to heighten UTI contraction. Amongst such factors included; individuals changing their social habits, age, social economic status and health conditions [1]. In this study the possible linkage and associated risk factors that partially seemed to fuel contraction of UTI were investigated. How informed the study participants were about urinary tract infection was also considered, with a significantly low number of participants (14%) having no idea. Based on the study socio-demographic characteristics data, the prevalence rate of urinary tract infection in relation to age was at 29.2% among those aged between 21 - 30 years. This was low compared to that among those aged between 41 - 50 years of 42.9%. However, those aged above 50 years had a UTI prevalence rate of 27.3%, which was afflicted to most of them having other underlying co-morbidities like diabetic and indwelling catheters (Table 2). The UTI prevalence among those over 50 years did concur to the finding reported in Nigeria by Anuli et al. 2016 where most of the elderly participants’ also had an increased risk of developing UTI due to factors such as kidney stones, hormonal changes or prostrate problems [1].
Sexual activities, wearing non-cotton underwear and poor personal hygiene have previously been documented to be key factors that influence contraction of UTI [18]. Much of the same findings were revealed by the data analysis reports in relation to frequent sexual activity, wearing non-cotton underpants, and poor personal hygiene (Table 2). Study participants within the cohort of ≤30 years had UTI positivity rate of 31% and agreed to be sexually active more than twice a week. This finding is in tandem and supported the views documented in prior research studies on how during sexual intercourse, thrusting could introduce bacteria up the urethra and into the bladder, increasing the risk of UTI contraction [12] [28]. Again, the finding on the poor personal hygiene also seconds that such conditions create a suitable environment for pathogens to thrive (Table 4). Therefore there is the need to enlighten individuals on optimum personal hygiene to halt UTI contraction. In addition, knowing the individual’s knowledge and population-specific UTI-associated risk factors may help tailor prophylactic strategies to curb contraction UTIs [37].
The outpatient department shows antenatal participants recording the highest UTI prevalence rate of (34%). This is in agreement with the finding of a study by Dimetry et al. 2007 where high UTI prevalence rate was reported among pregnant women [38]. Again, the reported urinary tract infection prevalence among pregnant women in this study compared to that of 29% reported at Ismailia city, Egypt [2] and that of 15.7% reported at Pumwani, Kenya [25] is higher and signals a worrying health concern that needs a prudent solution. More clinical and laboratory investigations to determine the factors that may be by far be influencing UTI occurrence in pregnancy must be embraced. Furthermore, the American pregnancy association did record that the uterus sits on top of the bladder, and during pregnancy as the uterus grows; the increase in weight blocks the drainage of the urine from the bladder causing an infection. In addition, the high sugar and protein levels in the urine of pregnant mothers may fuel the contraction of UTI [8] [20] [22]. However, according to the study data analysis there was no significant association of UTI contraction with demographic characteristics such as: marital status, level of education, occupation, social economic status, and blood pressure readings (Table 2 and Table 5).
Quite a number of bacterial etiological agents were isolated as responsible for UTI among the study population (Table 1). This finding is not unique to this study and is in tandem to other previous UTI studies [11] [15] [18] [25]. E. coli was the commonest isolated bacteria pathogen at (38.5%), followed by Staphylococcus aureus (21%) and Klebsiellapneumonia (19.3%) respectively. Analysis of the isolate’s data provided crucial information which revealed drug and multi-drug resistance patterns amongst both Gram-positive and Gram-negative bacteria (Table 6 and Table 7). The noted resistance patterns may be attributed to various captured factors amongst the participants. These included purchasing of antibiotics over the counter without proper prescription that leads to drug misuse and promotes antimicrobial resistance trends since there is no relevant laboratory investigation to reveal drug susceptibility. Again, study participants admitted to the use of antibiotics as a prophylactic measure, and delay to seek medical attention on time, a situation that may be fuelling treatment failure. Considering all these aforementioned factors and the revealed resistance findings endorses that antimicrobial resistance is on an exponential stage. E. coli and Staphylococcus aureus specifically exhibited the highest resistance trends at a range of 33% to 75% towards Ampicillin, Tetracycline and Sulfamethoxazole (Table 6 and Table 7). These findings concur with other related studies from the regional that documented E. coli being resistant to most of the studies test antibiotics [7] [18] [39].
The susceptibility profile of Staphylococcus aureus against Ceftriaxone was at 25%, similar to that noted at Gondar Teaching Hospital, Ethiopia [22] but different to that of 37% reported at Agha Khan University Hospital [18]. This is an encouraging observation that indicates that with prudent antimicrobial stewardship, antimicrobial resistance trends can be halted. However, going by the resistance patterns of Klebsiella pneumoniae isolates of 27% compared to that of E. coli at 14% against Nitrofurantoin there is still a huge gap that requires to be addressed. Again, the demonstrated resistance trends against Sulfurmethoxazole and Nalidixic acid by most of the study isolates between 60% to 80% does concur with the findings by Masika et al. 2017 [39]. It is therefore plausible that pathogens from this region may have developed other survival mechanisms to enable their resistance development to commonly used antibiotics over the years.
The noticed antimicrobial resistance (AMR) and multiple drug resistance (MDR) findings can also be attributed to long-term empirical prescription of most of the study drugs over the years. For instance, going by the noted resistance trends, Sulfurmethoxazole and Ampicillin are no longer potent enough to be prescribed as 1st line antibiotics in empirical management. Therefore, due to this increased AMR and MDR, more alternative antibiotic breakthroughs are awaited with many optimizations worldwide. Campaigning for the enlightenment of the public domain to discourage the use of antibiotics in a prophylactic measure rather than a therapeutic measure will be very essential to retain efficacy of the drugs that remain. However, there is also the need to periodically revise the country’s UTI treatment guidelines to ensure that some antibiotics are reserved only for the very critical established infections. Holistic scientific research to unearth uropathogens genotypic carriage of ESBLs resistance genes that may be mediating resistance against antibiotics is also indispensable [40]. This will assist in obtaining phylogeny data that will shed light on the genetic relatedness of bacterial isolates and explain whether any major clones are circulating in the population, fueling treatment failure. Additionally, crucial information on whether uropathogens have developed traits that may negatively impact antibiotics’ cidal actions will be achieved. The developments of vaccines and drug sensitivity rapid diagnostic kits as future prospect are also firmly recommended since this will help minimise the turnaround time for culture microbiology results, hamper UTI contraction, and minimise the overreliance of empirical UTI management.
5. Conclusion
According to our findings, UTI is still a very common infection among adults requiring efficient, prompt diagnosis and treatment. The unearthed study UTI prevalence rate certainly justifies the need for further investigations to improve on diagnosis, management and shun recurrence. Again, the finding of scrutinized risk associated factors plainly endorses the need to regularly explain the circumstances that may be by degrees fuelling the contraction of urinary tract infection. Also, it is distinct that management of UTIs without relevant microbial data is prone to inappropriate antibiotic prescription hence the need to embrace urine culture in every UTI management to promote proper antimicrobial stewardship. Furthermore, this will offer support to pharmaceutical industries that have fewer new antibiotics in the pipeline. However, due to the revealed study isolates resistance trends, a long-lasting solution to stagnate uropathogens rising antibiotic resistance is urgent.
Acknowledgements
To the study participants, thank you for agreeing to take part in this study. The authors wish to further express heartfelt gratitude to all KEMRI/CMR (molecular biology) staff members for their invaluable assistance. We are also grateful to the clinicians, laboratory technologists, and the administration Kiambu level 5 Hospital for their guidance and support, which allowed this study to succeed. This study was funded by HATUA (Holistic Approach to Unravel Antimicrobial resistance in East Africa) research funds. The funders had no role in study design, data collection and analysis, decision to publish, or manuscript preparation.
Authors’ Contribution
Fredrick Wanja (FW) was the principal investigator and came up with the study concept with guidance from Dr. Eric Omwenga. FW designed, carried out the lab work, data analysis and drafted the manuscript. John Maina participated in sample collection and drafting of the manuscript. Dr. Caroline Ngugi and Dr. Eric Omwenga assisted in preparation and harmonization of the manuscript. Dr. John Kiiru took part in the study design and supervised the lab bench work. All authors read and endorsed the manuscript.
Authors’ Information
Fredrick Kimunya (FK) is a master’s student in Kenya studying Infectious Diseases and Vaccinology at Jomo Kenyatta University of agriculture and technology. John Maina (JM) is a scientific researcher at the Centre of Microbiology Research, Kenya Medical Research Institute, Nairobi, Kenya. Dr. Caroline Ngugi (CN) is the Chairperson Department of Medical Microbiology, Jomo Kenyatta University of Agriculture and Technology who possesses vast experience in proposal development. Dr. Eric Omwenga (EO) is the Chairperson Department of Microbiology & Parasitological, Kisii University. He assisted in coming up with the study concept and revision of the content of the manuscript. Dr. John Kiiru (JK) took part in the study design and actualization of the content of the manuscript. He is a senior researcher at the Centre of Microbiology Research, Kenya Medical Research Institute, Nairobi, Kenya and the Head of Laboratory Ministry of Health, Nairobi, Kenya who has vast knowledge in infectious diseases and microbiology.
Ethical Approval
Approved (Supplementary Data S1 and Supplementary Data S2).
Supplementary Data S1
Ethical approval from the KNH-UoN ethical research committee
Supplementary Data S2
Ethical approval from National Commission for Science, Technology and Innovation (NACOSTI)
Supplementary Data S3
Examples of study isolates’ colony morphologies

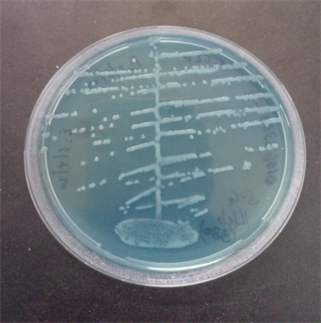
(a) Gram negative (Escherichia coli) (b) Gram-negative (Proteus mirabilis)

(c) Gram-positive (Staphylococcusaureus)