1. Introduction
Polygonum multiflorum (brand name Fo-Ti), also known as “he shou wu, HSW” is a climbing plant that grows natively in China, Taiwan and Japan [1]. HSW is gaining popularity and is promoted to be an antioxidant, antiaging, and neuroprotective herb that may prevent hair graying, and maintain liver and kidney health. Historically, hill tribes of Sumatra used the juice of Polygonum species to treat wounds [2]. However, HSW has been previously shown to cause acute liver injury and failure that at times requires liver transplantation, and has even led to death [3] [4].
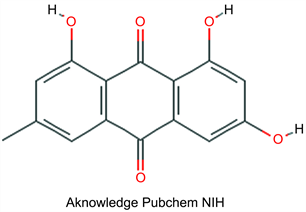
Two main chemical compounds have been identified in HSW: 2,3,4',5-tetrahydroxystilbene 2-O-β-D-glucoside, and emodin. The amount of each compound present in a supplement depends on the form of HSW form—whether it is processed or unprocessed—and whether or not the supplement is contaminated with other herbs. It has been reported that after processing of raw HSW prior to its sale, the content of 2,3,4',5-tetrahydroxystilbene 2-O-β-D-glucoside decreases by 55.8%, whereas the content of emodin increases by 34.0% [5], which may reduce the potential for liver injury as demonstrated in previous animal studies.
Emodin (1,3,8-trihydroxy-6-methylanthraquinone), an anthraquinone derivative found in HSW, is the active ingredient in many other traditional Chinese medicines (TCM). Emodin has many potential medical applications as an anti-cancer, neuroprotective, anti-infection and antidiabetic agent. However, many previously published reports have indicated that emodin may also be associated with liver, kidney and reproductive toxicity [4].
The mechanism by which emodin induces liver injury is proposed to be through glutathione depletion and fatty acid metabolism. To our knowledge, there is little evidence in the literature on the effectiveness of N-Acetyl cysteine as a sole therapy to treat drug-induced liver injury (DILI) associated with HSW. In this case report, we describe the use of N-acetylcysteine (NAC) in the treatment of a case of HSW induced liver injury.
2. Case Report
A 23-year-old previously healthy man presented with yellowish sclera, epigastric discomfort, acid reflux feeling, fatigue and darkening of urine of one-week duration. He reported the use of a Chinese herb named Fo-Ti (Polygonum multiflorum) 625 mg twice daily (1.25 g grams/day) for two months before presentation for its antioxidant and health benefits as was recommended by a medical doctor on a television channel (Appendix 1). He reported occasional alcohol intake but denied any history of recent travel or illicit drug use. Several of the patient’s family members had also used the same supplement but stopped after one month, and on subsequent testing, all had normal liver function tests (LFT).
Physical examination revealed jaundice, with no stigmata of chronic liver disease.
Initially, his laboratory results showed markedly elevated transaminases (Table 1) and to a lesser extent an increase in total and direct bilirubin, a profile consistent with acute hepatocellular injury. Testing for infectious and autoimmune causes was unremarkable. Hepatitis viruses (A, B, C), cytomegalovirus and Epstein-Barr virus serology were negative. Autoimmune markers including Anti-Nuclear Antibody, Anti-Smooth Muscle Antibody, and Anti-liver-kidney microsomal antibodies were not detected. Acetaminophen level was <5 mcg/mL. His electrolytes, coagulation and renal profiles were within normal limits. Abdominal ultrasound demonstrated an increase in periportal echoes, suggestive of hepatitis.
The patient was admitted to the hospital. Fo-Ti was stopped, and he was started on a loading dose of 140 mg/kg of oral N-acetylcysteine (NAC) then maintained on 70 mg/kg every 4 hours. On the fourth day, the patient was clinically well, and his liver enzymes were decreasing (Table 1). He was discharged home on esomeprazole for suspected concomitant GERD and oral NAC. However, he returned on the two days after discharge with worsening jaundice and minimal elevation of liver enzymes since discharge (Table 1). He was readmitted, and esomeprazole was stopped due to concern it may be contributing to his transaminitis. The patient denied re-consumption of Fo-Ti or any other medications. An abdominal MRI was consistent with hepatitis without other additional findings. Gas-chromatography-mass spectrometry (GC/MS) of herbal product (FO-TI) confirmed the presence of emodin as listed on the supplement label. Oral NAC was continued, and his liver enzymes normalized after the fifth week (Table 1 and Figure 1).
![]()
Figure 1. Potential association between the initiation of NAC and LFT improvement.
![]()
Table 1. LFT trending in association with NAC initiation and time factor.
3. Discussion
This case highlights the potential benefit of NAC as a treatment for DILI associated with Polygonum multiflorum. The mechanism of emodin-induced hepatotoxicity is unclear. It has been proposed that the disruption of glutathione (GSH) synthesis and disturbance of fatty acid oxidation metabolism in human liver cells by emodin may lead to hepatotoxicity [6]. Emodin binds cysteine, an essential precursor in glutathione synthesis, and forms cysteine adducts. Depletion of cysteine leads to a reduction of glutathione (GSH) leading to decreased cell protection from oxidative stress. The peak time of emodin-induced hepatotoxicity is directly correlated with the cumulative dose and longer duration of emodin consumption [7]. Decreased functional glutathione—due to the formation of emodin-cysteine adducts—could explain the favorable response of this patient to NAC due to replenished intracellular glutathione. Other proposed mechanisms of emodin toxicity include direct cytotoxicity, hepatic cell apoptosis due to interference with mitochondrial functioning [8], and idiosyncratic hepatotoxicity [9].
Intravenous NAC improves transplant-free survival in patients with early-stage non-acetaminophen hepatic encephalopathy grade I and II [10], and speeds hepatic recovery.
Since this patient improved during NAC therapy, the mechanism of therapeutic benefit due to NAC therapy in Polygonum multiflorum induce liver injury needs further studies.
The duration of HSW intake previously described to cause DILI ranges from one to 180 days [11]. Our patient had clinical manifestations after two months of HSW consumption. The duration of our patient’s hepatotoxicity is prolonged, consistent with previous reports that described a mean hospital length of stay of 29.5 days [12]. Esomeprazole is metabolized to toxic metabolites (hydroxy, 5-O-desmethyl, and sulfone metabolites) through P450 enzymes and it is unclear if esomeprazole directly caused hepatotoxicity [13] [14], or if there is a synergistic effect of hepatotoxicity with emodin that eventually worsened our patient’s transaminitis.
As the use of supplements and other purported health aids is on the rise, the documentation of adverse clinical effects related to their use is crucial. Among U.S. adults aged 18 and over in 2002, 2007, and 2012, the percentage who used any complementary health approach in the past 12 months ranged from 32.3% in 2002 to 35.5% in 2007 and was most recently 33.2% in 2012 [15]. Matching of CAM use to values, beliefs and philosophical orientation toward health and life of users are the main predictors of use [16]. Many users of complementary and alternative therapies believe that if a product is “natural” (rather than a traditional pharmaceutical agent) this must mean it is safe to use. This belief regarding the effects of CAM is deceptive and may lead to severe adverse health outcomes [17]. Therefore, public health awareness programs based on scientific evidence that seeks to educate the public regarding the potential risk of Polygonum multiflorum and other herbal products are crucial.
4. Conclusion
Polygonum multiflorum is associated with severe and prolonged DILI. Oral NAC therapy could be considered for the treatment of these patients due to the favorable risk-benefit ratio and the relatively extended duration of the illness.
Appendix 1