PreEMPT (Preterm Infant Early Intervention for Movement and Participation Trial): The Feasibility of a Novel, Participation-Focused Early Physiotherapy Intervention Supported by Telehealth in Regional Australia—A Protocol ()
1. Background
Preterm infants, those who are born prior to 37 weeks completed gestation, experience a higher risk of neurodevelopmental delay and disability in motor developmental domains compared to their term-born peers [1]. As such, early intervention is often recommended to improve outcomes [2] [3], however, many infants do not receive this early intervention. There are many gaps in the literature regarding the design, dosage and delivery models for early physiotherapy intervention for preterm infants. In terms of the design of content for early intervention, we are particularly interested in investigating whether a novel participation-focused early physiotherapy intervention is feasible for preterm infants and their families as there is evidence for the use of participation-focused goals to support the participation of older children [4]. Furthermore, while research in the area of early physiotherapy intervention for preterm infants has primarily centred around those living in metropolitan cities, there is a paucity of research that investigates delivery models using telehealth for preterm infants residing in regional or rural locations.
Each year, approximately 24,000 infants are born prematurely in Australia, with approximately 3500 of these infants residing in regional and remote locations [5] and there is evidence to suggest that these preterm infants differ compared to their metropolitan counterparts in terms of rates and access to services. The rate of preterm birth is higher for infants born in rural and remote Queensland, Australia (7.3 - 8.3/100 live births) compared to those born in major cities (6.5/100 live births) [6]. Many previous studies examining the efficacy of early physiotherapy intervention for motor outcomes have recruited infants primarily from metropolitan areas, however, preterm infants residing in regional Australia may face additional stressors when it comes to accessing medical and therapeutic services than their metropolitan counterparts [7], and consequently may require a tailored approach to their early intervention. Mahoney and colleagues (2017) [8] found that while there was no significant difference in moderate/ severe functional disability between infants born in obstetric hospitals with tertiary NICUs and those born elsewhere, including those infants whose mother’s usual place of residence was a rural or regional town, infants not born in NICUs were far more likely to be lost to be follow-up (23.3% vs. 42.9%). Therefore, it is reasonable to assume that we do not yet know whether preterm infants who reside in regional Australia are more likely to experience neurodevelopmental delay or disability than their metropolitan counterparts due to loss to follow-up. This study further highlighted the need for high quality follow-up and early intervention for rural and regional preterm infants in their local communities to pre-emptively develop connections between families with preterm infants and health services.
Early intervention programs for preterm infants have demonstrated a small positive influence on motor and cognitive outcomes during infancy, with improvements in cognitive outcomes sustained until preschool age [3]. The key ingredients to successful early intervention programs include: interventions aimed at improving both the infant’s development and interventions supporting the infant/parent dyad [2] [3] [9]. One way to further categorise the target outcomes of this research into early intervention for preterm infants is to consider them in reference to the International Classification of Functioning, Disability and Health (ICF). The World Health Organisation (2001) created the ICF framework to describe an individual’s health status as a complex interplay between their Body Functions and Structure, performance in Activities, and Participation in meaningful life situations within a context of Environmental and Personal factors. Overlaying the ICF on the key ingredients for early intervention for preterm infants, the primary focus for interventions has been to improve outcomes at the Body Functions and Structures and/or Activities level. Interventions supporting the infant-parent dyad could be viewed as targeting Environmental contextual factor of Support and Relationships. The ICF domain that has yet to be both explicitly targeted and evaluated for preterm infants is Participation.
Well described by Imms and colleagues in 2017, participation is the attendance and involvement in life situations. Participation in meaningful life situations has appropriately gained importance over the last ten years for goal-setting [10], outcomes [11] and has itself been a focus of intervention for older children and adolescents [4] [12]. Little is known about what infant participation looks like, how it is influenced or changes over time, and whether it could be the foundation of an early intervention approach to a population of infants known to benefit from early intervention: preterm infants. No studies to our knowledge have investigated the feasibility of a participation goal-based approach to support preterm infant motor and participation outcomes.
In addition to the research gaps relating to participation outcomes and the unique needs of regional preterm infants, there are further factors that require attention when planning early intervention research. It is important that research into early intervention programs for preterm infants residing in regional areas should be conscious of the “real world” service parameters experienced by clinicians working in government health services. For example, in the government service Queensland Health, physiotherapists provide outpatient follow-up services for preterm infants and their families in a clinic setting, with little scope available for home visiting. It makes sense then to conduct research within these parameters, and to trial novel approaches such as telehealth as an adjunct to face-to-face appointments to support preterm infants and their families in their home environments.
Telehealth, the use of video calls between clinicians and families, has so far been used more extensively by allied health professionals in the assessment of and treatment for adults than in paediatric populations. For example, telehealth has shown promise in the physiotherapy assessment and treatment of adults with musculoskeletal conditions [13] and adults undergoing neurorehabilitation [14]. In terms of the utilisation of telehealth programs for children and their families, there is a broad spectrum of research on various populations, delivery models and purposes. Some examples include the assessment of infant gross motor development via video recordings [15] [16] or via real time video call [17], training for parents of children with Autism Spectrum Disorder [18], and evaluating parental experience of telehealth from parents with children with complex disabilities [19]. A recent systematic review of the diversity of telehealth practices in children with disabilities [20] identified that effective interventions tended to be “targeted at parents, centred around an exercise program, used a coaching approach, focused on improving children’s behavioural functioning, lasted at least >8 weeks and were offered at least once per week”. No studies to date have explored the effectiveness of telehealth in the assessment of and intervention for preterm infants.
Taking into consideration the limitations of previous research relating to participation and preterm infants and the needs of preterm infants who reside in regional areas, we developed PreEMPT. The content of the PreEMPT intervention was not specifically developed in reference to the needs of preterm infants residing in regional Australia, however, was derived from previous research for preterm infants more generally and emerging participation-related research in older children. Key ingredients of successful early intervention approaches identified in the literature include a. early intervention programs aimed to improve infant development and b. interventions supporting the infant-parent dyad [3]. There is also evidence to suggest physiotherapy intervention can improve the participation outcomes of older children with physical disabilities [4] [12] [21] including evidence for participation in meaningful activities effecting changes to a child’s body structure and function [22]. PreEMPT drew upon this previous research and extended it by centring an infant’s participation in meaningful life situations as the foundation from which related infant developmental activities, body structure and functions and environmental factors are addressed.
When considered collectively, there are two aspects of early physiotherapy intervention for preterm infants that require investigation: 1) the feasibility of using telehealth as an adjunct to face to face physiotherapy sessions for preterm infants; and 2) the feasibility of a participation-focussed early physiotherapy intervention to improve both a known outcome (motor performance) and unknown to date outcome (participation).
2. Study Aims and Hypotheses
The aim of this study is to conduct a randomised controlled trial to determine the feasibility of a novel, participation-focused early physiotherapy intervention for preterm infants (called PreEMPT) compared with Usual Physiotherapy Care (UPC) in a regional Australian hospital outpatient context.
To determine feasibility, Bowen et al. (2009) [23] proposed eight areas of focus for feasibility studies including: acceptability, demand, implementation, practicality, adaptation, integration, expansion and limited efficacy testing. Feasibility in this study will be determined according to five factors. Acceptability will be examined by parent reported satisfaction with: their participation in the study; individual aspects of the study such as the PreEMPT or UPC intervention; and the use of tele-health. Demand and practicality will be examined by recruitment rate, and the number of telehealth sessions that ran smoothly versus telehealth sessions with challenges. Implementation will be examined by attendance at assessment appointments (including follow-up rate) and attendance at treatment appointment. Limited efficacy testing will be examined by comparing PreEMPT to UPC on preterm infant motor performance, general development, participation, and parental wellbeing.
We hypothesise that:
• 75% of infants eligible for the study will consent and participate;
• Infants and their parents will attend 80% of assessment appointments;
• Infants and their parents will attend 80% of their treatment appointments;
• Parents will report high levels of satisfaction and perceived benefit from PreEMPT sessions.
3. Method
3.1. Study Sample and Recruitment
Twenty-six preterm born infants will be recruited prior to term corrected age from a Special Care Nursery in a large regional hospital in Queensland Australia, or if eligible infants (see Inclusion criteria) have completed their neonatal care at another hospital, infants may also be recruited from the Paediatric Physiotherapy Outpatient Department of the same hospital.
Parents of eligible infants will be provided an information sheet about the purpose and design of the study during their SCN admission or receive it via mail if their infant has been discharged prior to receiving it as an inpatient. Parents will then receive follow-up contact (in person or via phone) by the chief investigator (CM) to answer questions about the study and establish interest in consenting for the study. Parents who do not consent to be in the study will be offered standard physiotherapy care at the regional hospital.
The Human Research and Ethics Committees for Children’s Health Queensland Hospital and Health Service and The University of Queensland have approved this study (approval numbers: HREC/17/QRCH/165 and HREC/2017001924/QRCH/165). This study has been prospectively registered on Australian and New Zealand Clinical Trial Registry (ANZCTR number ACTRN12618000119291).
Inclusion criteria
Eligible participants in the study will be infants born preterm ≤ 34 weeks and 6 days gestation, who:
• Reside within the health service catchment area and are eligible for Paediatric Medical Outpatient follow-up from the hospital.
• Can attend face-to-face sessions at the hospital over the 8 months of the trial
• Have access to an internet service either in-home or in an appropriate local setting to enable potential telehealth sessions.
• Have at least one care-giver who is able to understand and communicate in English well enough to enable telehealth provision.
Exclusion criteria
Infants diagnosed with a medical or behavioural condition known to impact motor development over and above being born pre-term (e.g. a genetic syndrome such as Down Syndrome) will not be eligible for the study.
Criteria for withdrawal from the study
Parents of infants can elect to withdraw from the study at any time without having to provide a reason. Intention to treat analysis will be completed regardless of how many proposed sessions an infant does not attend. Families will be contacted to reschedule missed appointments.
Sample size
To determine the sample size for this feasibility study, we estimate that the number of infants born in the catchment area in a six-month period who will be eligible for the study will be 35 - 40 infants based on data from previous years available from the hospital. We anticipate a recruitment rate of 75%, therefore suggesting a sample size of 26 - 30 will be possible.
3.2. Baseline Assessments, Randomisation and Allocation Concealment
Baseline assessments
Following determination of eligibility and gaining informed consent, infants will complete baseline assessments relating to their Body Function and Structure and motor performance using the Test of Infant Motor Performance (TIMP) and General Movements Assessment (GMA). The outcomes of these assessments will be used to stratify infants prior to randomisation according to the categories below. This will be performed to promote more even distribution of baseline motor abilities of infants between the UPC and PreEMPT intervention groups.
• High risk for motor difficulties: Infants who demonstrate “abnormal” writhing movements on the GMA AND/OR score less than the 16th centile (−1 Standard Deviation) on the TIMP at baseline (term corrected age).
• Low risk for motor difficulties: Infants who demonstrate “normal” writhing movements on the GMA AND who score between the 16th and 100th centiles on the TIMP at baseline (term corrected age).
After stratification, infants will be randomly assigned to intervention arms. Infants who are part of a multiple birth group (i.e. twins or triplets) will be randomised to the same intervention arm as the oldest sibling due to the nature of the intervention being impossible for the parent to implement home practice ideas differently without interference or cross over between intervention groups.
Randomisation
Infants will be randomised to an intervention arm using pre-prepared sealed opaque envelopes containing randomly generated numbers (1, 2) to represent UPC or PreEMPT intervention groups. At the time of randomisation, CI Mobbs will contact a researcher in the Children’s Motor Control Research Collaboration Group at The University of Queensland who not involved in the study design, assessment or treatment of infants in the study to select an envelope. Infants will then proceed to take part in the study in the allocated treatment arm and at no time will the assessing physiotherapist/s have any knowledge of treatment group allocation.
Allocation concealment
Assessors (trained physiotherapists) blinded to group allocation will complete post intervention assessments at four-, six- and eight-months corrected age (CA). If a second opinion on a GMA video is required, a researcher blinded to group allocation and not involved in randomisation will review the video assessment remotely.
While families will not be explicitly told which group they are allocated to, it is not possible for parents to be blinded to group allocation as the information they receive via the information sheet prior to giving consent describes a difference in treatment session frequency.
3.3. Intervention
The intervention period of the study will be between two- and 15-weeks CA (Figure 1).
PreEMPT
![]()
Figure 1. Timetable of PreEMPT and usual physiotherapy care intervention sessions.
Preterm infant Early intervention for Movement and Participation Trial (PreEMPT) is a novel, participation-focused early physiotherapy intervention for preterm infants aimed at improving motor performance and participation in meaningful life situations. Outlined below are the two components of the PreEMPT intervention: 1) the content of the intervention and 2) the model of service delivery and dose. Following this, the program and individual session structure will be described.
Content of intervention
The three tenets of PreEMPT are:
1) Participation-focused goal setting, and using participation in meaningful life situations to guide treatment strategy selection
2) Life situation task analysis to drill down to the contributing body structures and functions, activities and environmental enhancers and barriers to attendance and involvement in the identified life situation
3) Strengths-based parent enablement using family-centred principles to build the parents’ capacity in identifying meaningful life situations their infant participates in and supporting their confidence and competence to maximise their infant’s participation attendance and involvement.
3.4. Participation-Focused Goal Setting
Theoretical underpinnings
Participation is the attendance and involvement in life situations [24] and could be considered the ultimate health outcome in the field of childhood disability [10] [25]. Improving the participation of older children with disabilities has become increasingly targeted in research and practice, however, has not traditionally been the focus of early intervention for preterm infants. Given the holistic importance of participation as an outcome, PreEMPT uses participation frameworks from the International Classification of Functioning, Disability and Health (ICF) [25] and the family of Participation Related Constructs [24] to both guide goal setting and measurement of outcome.
PreEMPT focuses on participation by: 1) Using life situations generated by parents (with and without the support of visual guides to spark parents’ choices) as goals to construct the therapy intervention around and 2) Using the ICF as a framework, supporting parents to gain knowledge in how an infant’s body structure and function, ability to perform different activities, and the different personal and environmental factors may impact an infant’s participation.
Practical applications in the context of PreEMPT
Parents in the PreEMPT group will be invited to set participation-related goals from a selection of cards with photos of infants participating in various life situations (see Appendix 1). The photos were selected to depict the various life situations might participate in based on life situations from measures identified in a systematic review on infant participation measures (Mobbs et al., 2020 submitted: under review). Parents will be asked to select three cards depicting what they feel they would like their infant to participate in and/or what they feel their infant is ready to participate in next. These cards will represent the goals for the infant over the next 2 - 4 weeks. The goals have the option to be updated multiple times over the intervention period to reflect the changing nature of the infant’s and parent’s activity competence, preferences, and emerging sense of self during this period of rapid developmental growth.
Following the goal selection, the physiotherapist will ask the family to set up their infant to participate in one of the life situations. If this cannot be adequately replicated in the clinic environment, the next telehealth session will provide the opportunity to assess the infant in its natural context. The process for unpacking the contributing factors to the infant’s participation will be described in the next Section 2. Life situation task analysis.
3.5. Life Situation Task Analysis for Treatment Strategy Selection
Theoretical underpinnings
Characterised as a “top down” approach, PreEMPT uses the life situation identified by the parent as the starting point for treatment strategy selection. Participation attendance and involvement of an infant in certain life situations are analysed to identify factors in the infant’s body function and structure, activity and contextual domains that influence the infant’s participation. Similar to the task analysis used in other rehabilitation approaches [26] [27] [28], the PreEMPT physiotherapist both acts as a facilitator and “knowledge resource” for the parent to help identify factors in the ICF domains that might contribute to the infant’s participation attendance and involvement in the chosen life situation.
Practical applications in the context of PreEMPT
Following goal setting and assessment of the infant in the chosen life situation, the physiotherapist will use the ICF domains to identify the relative strengths and challenges for the infant in this life situation across body, structure and function, activity, environment, and personal factors. Where challenges are noted in a particular domain, parents are supported using strategies in the next section (3. Strengths-based parent enablement) to consider strategies to try to address any environmental barriers, activity limitations, and body function and structure impairments identified.
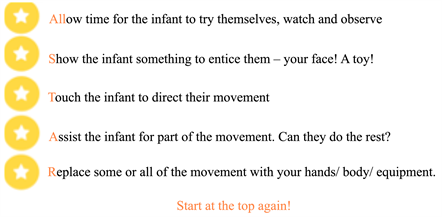
Where an activity limitation is identified as potentially influencing an infant’s participation, we developed the AllSTAR framework to help parents trial an intervention strategy at the “just right” level for their infant to produce a portion of self-initiated movement. Some examples of the hands-on facilitation to increase their attendance or involvement in the chosen life situation include: providing tactile cueing; proprioceptive information relating to weight-shift or muscle activation; and postural stabilisation of trunk or limbs for stability or boundary during movement. Hands-on facilitation is faded as soon as the infant is able to contribute more self-initiated movement towards the life situation at hand.
A further detailed example is provided in Appendix 2.
3.6. Strengths-Based Parent Enablement
Infants depend upon, learn from and form the strongest attachment with their parents or caregivers. It would come as no surprise to then consider that infants should not be treated in isolation, but rather approached as part of a strong, influential dynamic with their parent. The infant-parent dyad or relationship is at the foundation of PreEMPT intervention. Understanding this unique dyad for each and every family is vital to building a successful therapeutic relationship. To support the infant-parent dyad, PreEMPT draws upon the following frameworks to enhance competence, confidence and self-efficacy in parents of preterm infants:
• Family-centred practice: Family-centred practice or care is an approach to working with families in the field of childhood disability [29]. Working from a family-centred perspective encourages clinicians to consider each family as unique, with their own strengths and needs, and place the family at the centre of the therapeutic relationship [30]. It promotes collaboration between families and therapists, and values the expertise families hold about their infant’s abilities, needs and the unique circumstances of their family.
PreEMPT is founded upon family-centred care as it has been designed to place the family at the centre of all interactions, treats each family as unique, values the expertise that each family brings about themselves and their baby and offers the therapist’s knowledge like a resource for the family to draw upon as they wish.
• Occupational Performance Coaching (OPC): OPC is an approach to supporting individuals with occupational performance challenges that is founded on family-centred and strengths-based values [31]. The “coaching” aspect of OPC refers to the clinician utilising a goal-focussed conversation to guide the parent or individual to identify meaningful areas of daily performance they would like to change and identify and select treatment strategies that work best for that family. Three enabling domains are utilised by the therapist during sessions: Emotional support (verbal and non-verbal strategies to help the parent move from problem-focused to solution focused frame of the identified issue); Information exchange (guiding parent to draw upon existing knowledge and help highlight gaps in knowledge) and a structured process (a process the therapist to uses to gauge a parent’s perception of their child’s performance in a certain task, what the parent would prefer the performance to look like, explore enablers and barriers to that change in performance and the child’s needs in implementing changes to performance) [32]. The therapist may demonstrate hands-on or facilitation strategies to enable the parent to choose which strategies they would like to implement with their child [31].
Practical applications in the context of PreEMPT
Each family is considered the expert on their infant, and the PreEMPT physiotherapist offers themselves as a resource that a family may access to support their infant. PreEMPT utilises OPC strategies such as emotional support with open-ended, solution-focused questions during goal-setting, reflection about performance and selecting treatment strategies; information exchange to understand a parent’s knowledge and perception of their infant’s performance, and to identify gaps in a parent’s knowledge to then offer strategies that might be of use for a parent to then consider; and shares a parallel with the OPC structured process to guide the parent through goal setting, identification of potential factors that would help or hinder their infant’s performance and trialling and offering strategies for the parent to select to support their infant’s attendance and involvement in life situations. For further examples regarding the types and style of questions, see Appendix 2.
Model of service delivery and dose
The model of service delivery used in the PreEMPT intervention was informed by the local clinical context and exploring whether telehealth may be a beneficial adjunct to face-to-face appointments. While most research studies on early physiotherapy intervention for preterm infants have been delivered in the home environment [3], many Australian state government health services only provide clinic-based appointments. It was vitally important to allow for this service reality in the development of PreEMPT, so in order to add elements of ease, accessibility and the ability to be able to provide therapeutic strategies related to an infant’s home context, telehealth sessions were selected as an adjunct to face-to-face appointments.
PreEMPT will be delivered via alternating weekly face-to-face sessions in an outpatient clinic and telehealth sessions. Sessions will commence at two weeks CA and cease at 15 weeks CA, with infants receiving a maximum of seven face-to-face clinic appointments of 45 minutes duration each and seven telehealth appointments of between 20 - 45 minutes duration each.
PreEMPT program structure
In this study, PreEMPT will be evaluated over a 14 week period. During this time, the PreEMPT therapist will gradually build the capacity of the parent to identify meaningful life situations for their infant to participate in, expose the parent to language regarding participation (such as using the phrase “life situation” when taking about a participation “activity”), how to read their infant’s cues relating to involvement in a life situation, and identify, trial and select treatment strategies. This is achieved in four distinct phases (see Figure 2) and each PreEMPT face-to-face session following the format in Figure 3.
At the end of the first session, the PreEMPT physiotherapist will ensure that the family has downloaded and trialled the tele-health app PEXIP prior to leaving.
Tele-health sessions enable the therapist to provide support for participation in life situations at home, and supporting practice of strategies trialled during
![]()
Figure 2. The four phases of the PreEMPT program structure.
therapy sessions. Tele-health sessions follow the same structure, though the duration may be less than 45 mins, depending on the needs of the family.
PreEMPT fidelity
Two experienced physiotherapists (CM and HB) will deliver the PreEMPT intervention sessions. CM devised the PreEMPT intervention, and created a training manual to enhance fidelity. A training program to train the second physiotherapist (HB) will be conducted consisting of education regarding theoretical background (four hours), observation of a session via video with educational commentary and discussion (two hours), in person observation of a face-to-face and telehealth session with education discussion after (two hours) and finally opportunity for the second therapist to lead a face-to-face and video session with observation and feedback from CM (two hours). Standardised PreEMPT resources, including templates for session plans and parent handouts, will be used by the PreEMPT therapist throughout the study. Sessions will be recorded to code for content and analyse fidelity. A review of chart notes at random will also be conducted by CM to evaluate the consistency of using the PreEMPT approach across the two therapists, and feedback will be provided to HB where necessary.
Usual Physiotherapy Care (UPC)
Usual Physiotherapy Care (UPC) is the physiotherapy care usually delivered by physiotherapists at the regional hospital for preterm infants in the first four months post term CA. To reduce bias, the content and dose of UPC will be thoroughly reported on through chart note review and video analysis coding at the completion of the study so as to not cue the physiotherapist providing UPC to modify their usual care based on their participation in the study. The following is a description of what is currently known about UPC at the regional hospital.
1) Content of intervention
UPC usually involves two to three physiotherapy appointments to examine motor development using the GMA at ages known to be predictive of later motor outcomes: i.e. two to four weeks CA, 11 - 12 weeks CA, with an optional assessment at 13 - 14 weeks if an infant is identified as being at-risk (has absent or abnormal “fidgety movements”) (Figure 1). Other motor assessments (such as the TIMP or AIMS) or components of neuro-developmental assessments (such as the NSMDA) are also used to assess the neurodevelopment of preterm infants to guide follow-up trajectories. Based on the findings of these assessments, the UPC physiotherapist will demonstrate some sensorimotor activities to support the infant’s development. A short physiotherapy home program may also be provided for parents to deliver.
2) Model of service delivery and dose
UPC is delivered via outpatient clinic appointments at the regional hospital. Preterm infants usually receive two to three physiotherapy appointments in the first four months CA (see above), with each appointment lasting 20 - 40 minutes.
UPC fidelity
Physiotherapists delivering UPC will have a minimum of two years’ experience working with infants.
Conditions applicable to both PreEMPT and UPC
Physiotherapists providing intervention (i.e. in UPC or PreEMPT) will be blinded to baseline assessment outcomes of the infant and parent.
Parents of infants in both groups will be provided with a notebook at the first session to record the amount of home practice undertaken to more accurately gauge dose of the intervention and note other appointments they attend in during the intervention period.
4. Outcome Measures
The feasibility of PreEMPT will be evaluated as per the criteria outlined under Study aims and hypotheses. To evaluate the assessment processes and sample size calculations for outcome measures for future iterations of PreEMPT, the following outline is provided regarding chosen outcome measures.
4.1. Participant Characteristics
Perinatal data from medical records, including any results from developmental assessments performed during the preterm period, as well as socio-demographic information will be collected following consent.
4.2. Outcome Measures
Outcome measures will be administered by a physiotherapist with at least two years working with infants, who are trained and experienced in performing all assessments. The assessing physiotherapist will be blinded to treatment allocation and previous assessment data.
Assessments will be performed at five time points (see Figure 4): T1 - Baseline
![]()
Figure 4. Timeline of assessments for PreEMPT study. TIMP: Test of Infant Motor Performance, GMA: General Movements Assessment, AIMS: Alberta Infant Motor Scale, NSMDA: Neurosensory Motor Developmental Assessment, Bayley: Bayley Scales of Infant and Toddler Development, 3rd Edition, DAIS: Daily Activities of Infants Scale, Survey: Custom Infant Participation Survey, PSOC: Parental Sense of Competence Scale, HADS: Hospital Anxiety and Depression Scale, Satisfaction: Custom Satisfaction Survey.
(term CA); T2a: Fidgety age General Movements Assessment (three months CA); T2b: Immediate post intervention (four months CA); T3: Two months post intervention (six months CA) and T4: Four months post intervention (eight months CA).
4.2.1. Infant Outcome Measures
1) Body Function and Structure and Activity measures
Test of Infant Motor Performance (TIMP)
With 59 items (28 observed and 31 elicited), the TIMP assesses motor performance of infants between 34 weeks post conception age and four months CA. The TIMP has high test-retest (r = 0.89) and intra-rater reliability (ICC = 0.98 - 0.99) [33] and is able to evaluate clinically meaningful change pre and post intervention and is predictive of later developmental outcome [34]. While the minimal clinically significant change has not been determined in research, preterm infants randomised to an intervention group in an RCT performed significantly better on the 4 months CA TIMP assessment than those who received standard care [35]. A clinically meaningful change of 0.5 SD has been advised (Personal communication with TIMP author Professor Suzann Campbell, 2017).
The TIMP will be used in this study to assess infant motor performance at baseline (T1) and then again immediately post intervention at 4 months CA (T2b).
General Movements (GMA)
The GMA is used to examine an infant’s spontaneous movement in the preterm and early post-term period. Assessments are conducted in the “writhing” phase (preterm through to 6 weeks post term) and “fidgety” phase (10 weeks to 17 weeks post term age). The GMA at 3 months CA has excellent predictive validity for a subsequent diagnosis of cerebral palsy [36] and has good validity and reliability (kappa = 0.85 - 0.94 intra-rater reliability) [34]. More recently, the GMs assessment has been used at 3 months corrected age to evaluate outcomes from intervention [37] [38]. The GMA will be used in this study to give an indication of the risk for future motor impairment for this sample. The assessing physiotherapist capture a video of each infant at baseline and the intervention physiotherapist on the arm the infant is allocated to will capture video at three months CA. Videos will then be stored via a secure cloud-based database and scored by the blinded assessor and Investigator Spittle.
Alberta Infant Motor Scale (AIMS)
The AIMS is a norm referenced assessment of gross motor abilities for infants between the ages of 0 and 19 months [39], allowing for longer follow up than the TIMP. During the AIMS assessment, the infant is observed in supine, prone, sitting and standing and their responses observed in these positions are rated. The AIMS has high internal consistency (r2 = 0.99), intra-rater reliability (ICC = 0.98 - 0.99) and has good construct, content and predictive validity [34]. Scores less than the 10th centile at 4 months and 5th centile at 8 months have been shown to be correlated with abnormal development at 18 months [40]. Infants in this study will be assessed using the AIMS at T2b, T3 and T4 (i.e. 4-, 6- and 8-months CA).
Neuro-Sensory Motor Developmental Assessment (NSMDA)
The NSMDA is a criterion referenced, standardised assessment of motor development for children aged 1 month to 6 years [41]. The NSMDA assesses six domains of development (gross motor, fine motor, neurological, infant patterns of movement, postural development and sensory motor function) and infants are given a functional grade based on these assessments to classify their performance as normal, minimal, mild, moderate or severe dysfunction. The NSMDA is a criterion referenced tool with good ability to predict abnormal neurodevelopmental outcome at 8 months (sensitivity 82% and specificity 83% 95%CI) [41]. Infants in this study will be assessed using the NSMDA at 4- and 8-months CA.
Bayley Scales of Infant and Toddler Development 3rd Edition (BSID-III)
The BSITD-III is a set of normative value referenced assessments designed to evaluate the developmental progress of infants and children between the ages of 1 - 42 months [42]. Among the most commonly used developmental assessments in the preterm population, the BSITD-III contains cognitive, language, motor, social-emotional and adaptive behaviour scales. The examiner commences testing at the corrected age of the infant and then progresses or regresses through the assessment items based on whether an infant achieves a “passed” or “not passed” score on consecutive items [42]. This enables a developmental age for each dimension to be obtained. The BSITD-III has good psychometric properties, with good to excellent inter-rater reliability (0.85 - 0.99) and is moderately predictive of later motor function r = 0.32 (95%CI 0.26 - 0.42) [43]. In this study, infants will be assessed using the BSITD-III at T4 (8 months CA).
2) Participation measures infant outcomes rated by caregivers
In this study, we will explore the relationship between motor performance and participation in order to see whether PreEMPT Physiotherapy has more impact on infant participation in everyday activities than UPC.
To identify appropriate measures of participation for infants, we performed a systematic review (Mobbs, Spittle, Johnston, under review). Our results showed a paucity of measures to evaluate all participation dimensions for infants aged birth to 12 months. Therefore, we will be collecting this data from a combination of two parent questionnaires. Parent responses will be obtained firstly from the Daily Activities of Infants Scale (DAIS) and secondly from a custom designed questionnaire for participation dimensions not covered by other scales.
Daily Activities of Infants Scale (DAIS)
The DAIS was developed to measure antigravity postural control in infants aged between 4 - 11 months [44], however the nature of data obtained also enables examination of an infant’s frequency and diversity of participation attendance and level of independence across everyday life situations such as feeding, self-care and play. The DAIS has good test-retest reliability (ICC = 0.77) and inter-rater reliability (ICC = 0.76) [44]. The DAIS will be administered via parent report at T1 and T4 (4 and 8 months CA) to explore changes within and between groups.
Custom infant participation questionnaire
In addition to the DAIS, a custom questionnaire has been designed to explore infant participation in daily self-care, leisure and productivity situations that are not addressed by other published measures at this time. For each item, caregivers will be asked to rate whether their infant is present during an activity (e.g. family mealtimes, shopping), and if so, how often, where it takes place, who they participate with, how involved their infant is, and who chooses the life situation. These questions are similar in nature to those in the Children’s Assessment of Participation and Enjoyment [45], a measure designed for children aged 5 years and older. The questions capture the important constructs of participation of attendance (measures of participation frequency and diversity) and involvement (enjoyment, persistence), and participation-related constructs of preferences for participation. This questionnaire will be completed by parents at T1, T2b, T3 and T4 (term, 4-, 6- and 8-months CA).
4.2.2. Parent Outcome Measures
Parenting Sense of Competence Scale (PSOC)
Parental self-efficacy is essential to enable parents to support the development of their preterm born infant. It has been linked with positive maternal mental health and child development outcomes, and may play a protective role for maternal symptoms of depression [46]. The PSOC has been chosen to measure this attribute in parents in this study and to compare the relative influence of PreEMPT, which is based around a parent enablement model, with UPC. The PSOC is a 17-item scale, with each item rated on a six-point scale of “strongly disagree” to “strongly agree”. The PSOC has been validated for use with mothers of newborn infants and was found to have adequate internal consistency (Cronbach’s alpha 0.78) and construct validity through negative correlation with depressive symptoms [47]. In this study, the PSOC will be completed by caregivers at T1, T2 and T4 (term, 4- and 8-months CA).
Hospital Anxiety and Depression Scale (HADS)
Anxiety and depression symptoms are commonly reported in parents of preterm infants at higher rates than parents of term born infants. Studies investigating early physiotherapy and psychology intervention for mothers of preterm infants has shown a positive sustained effect on reducing reported depression symptoms up to eight years post intervention [48] The HADS is a 14-item self-report measure that assesses clinically significant states of anxiety and depression in a general hospital population [49]. Scores of 0 - 7 are considered “normal”, with scores of 8 - 11 “mild case” and greater than 11 as “definitive”. In the current study, the HADS will be completed by caregivers at T1, T2b and T4 (term, 4- and 8-months CA).
Custom satisfaction questionnaire
Satisfaction with physiotherapy intervention, including aspects about face-to-face interactions provided through Standard Physiotherapy Care and additional utility of the telehealth component of the PreEMPT group, will be collected via a parent reported survey at T2 (4 months CA). Questions will be based on the Measure of Processes of Care [50] to capture important elements related to the delivery of a family-centred service, and expanded upon to better survey parents of young infants.
4.3. Adverse Events
Any adverse events will be recorded by the treating physiotherapist at the completion of the session. They will be classified as Mild: parent reports a sign or symptom that is not interfering with the infant’s usual activity; Moderate: parent reports a sign or symptom that interferes with the infant’s usual activity or Severe: parent reports a sign or symptom that prevents the infant from completing usual activity. Queensland Health’s standard response to clinical incidents and follow up where appropriate will occur based in the severity of the adverse event.
With respect to collecting information relating to parent mental health, parents/ care givers who score in the range of clinical depression and/or anxiety will be offered referral to their general practitioner or Early Intervention Parenting Service at the hospital.
5. Analyses
Feasibility will be reported in terms of descriptive statistics (frequencies, means and 95% confidence intervals) relating to recruitment rate, percentage of assessment and treatment sessions attended, and parent reported satisfaction. As this study is a feasibility study and thus not adequately powered to detect between group differences, limited efficacy testing will be conducted as per Bowen et al. 2009 [23] to determine trends for future powered studies. Paired T-tests comparing the outcomes of infants in PreEMPT with those receiving UPC will be conducted, with the Test of Infant Motor Performance the main outcome of interest at 4-months CA to assess for trends in differences between groups. Models will be fitted using generalised estimating equations (GEEs) with exchangeable correlations structure and robust standard errors to allow for correlations between twins in the study for infant outcomes. Subsequent limited efficacy testing related to PreEMPT’s influence on infant motor performance, neurosensory motor performance, general development and parental mental well-being and self-efficacy will be also be conducted. As no previous research has explored the impact of early physiotherapy intervention on infant participation, descriptive statistics will be used to describe the participation of infants within groups over time as well as between groups.
6. Conclusion
This paper outlines the theoretical background and design for a feasibility study of an assessor-blind RCT comparing a novel early participation-focussed physiotherapy intervention (PreEMPT) for preterm infants with usual physiotherapy care in a regional Australian context.
Appendix 1
Picture cards depicting various life situations that an infant might participate in used in the Custom Participation Questionnaire (both intervention groups) and to prompt goal setting (PreEMPT group only).

Appendix 2
Example session for PreEMPT
1) Support parent to identify life situation they would like their infant to be able to participate in.
Example questions:
• What is something you would like your infant to participate in? You can use these cards if you like to help get you thinking about different life situations, or you might also have something in mind.
• What is something you feel your infant is ready to participate in next?
• What is something you have tried to help your infant participate in, but it may not be working as you hoped?
(Key: language at this point is participation focussed, not activity competence)
2) Parent identifies 1 - 3 life situations from the cards they would like support with
Example questions:
• Tell me what this looks like for you at (insert context – home, when you are out, in the car etc)?
• How would you like it to look different?
• What do you think might help your infant participate?
3) Parent identifies e.g. interaction and building relationships
• Assess infant in the life situation
• Use ICF domains to identify the relative strengths and challenges for the infant in this life situation across body, structure and function, activity, environment, personal factors.
• Comment on the infant/parent strengths e.g. “I notice how you wait for your baby to look at you, that is such a lovely way to show that you are ready to interact with them and allows them to interact with you on their terms”
4) With the parent, identify the challenges for the infant participating in the life situation.
If there are environmental barriers:
Ask questions such as
• “Have you had any thoughts about what changes could happen in how we have set this up for your baby” first; then wait for parent to invite you to comment/offer thoughts “Some other families have found that by changing (set up/equipment), it has helped their infant participate in this. How does that sound for you? Is that something you would like to try?”
If there are limitations in an infant’s activity competence:
Identify posture and movement behaviours impacting and associated body, structure and functions. E.g. infant unable to achieve midline head position independently to be able to gaze at parent to interact.
Use AllSTAR to guide parents through a process to find the most appropriate level of support to achieve participation.
The rationale behind each step is as follows:
Allow time for the infant to try it for themselves. Watch and observe.
Infant self-initiated movement
E.g. Ask the parent to set up how they might interact with their infant for the life situation of interacting and building relationships. Parent sets up with infant on the floor and parent above them. The infant might be unable to interact with them as they have their head rotated to the side and are arching.
Show the infant something to entice them. Your face! A toy!
Vision/auditory cue for movement
E.g. Parent moves their face in front of the infant and talks to them. Infant is not able to rotate their head to look at them.
Touch/tactile cue for the infant to direct their movement
E.g. Parent brushes their infant’s cheek
Assist the infant for part of the movement
Scaffolding (Motor Learning principle)
E.g. Roll the infant into side lying, then using handling near shoulder girdle and head/neck, rotate them back towards supine, seeing if the infant can assist with some of the head/neck rotation to midline
Proprioceptive cue
E.g. Provide direction of pressure diagonally across from ribcage to pelvis to elicit weight shift and head on body righting reaction to bring head into midline
Replace some or all of the movement
Enabling infant to participate without activity competence being a barrier
E.g. Position infant on parent’s lap in crook sitting to elevate head and create a well for the infant’s head to rest in midline between their thighs.
Continue to reassess and use a “curious” stance to help guide parents to watch and observe their infant’s cues. Where possible reduce the amount of support provided to the infant to enable moving “up” the AllSTAR framework to options that are less supportive. Build the parent’s capacity by inviting them to describe what their infant is doing, how involved they think they are (and how they can tell) and whether they think their infant is ready for less support.
5) Parents are invited (through similar questions used as examples in 1. and 2.) to trial intervention strategies. The physiotherapist will offer strategies in a way that acknowledges the parent’s effort, and guide the parent through how to facilitate their infant’s movement so that the parent has the opportunity to practice, seek feedback and become confident in supporting their infant’s participation in meaningful life situations.
6) Parents are provided with ideas to take home. The strategies are ones that they have trialled during the session, and framed in the AllSTAR frame work to enable parents to see ahead to what “less support” might look like so they can trial with their infant if they feel they are ready between sessions.