The Potential Sources of Transmitting of Hospital Acquired Infection by Routine Devices in Adult ICU in Alrass General Hospital ()
1. Introduction
Hospital acquired infection (HAI) also refers to nosocomial infections that are acquired from hospitalist patients who are admitted to the hospital for any reason other than the infections. The first infection appeared after 48 hours of hospital admission or within 30 days after the patient discharge [1]. Hospital acquired infections reflect as a major global safety concern for both patients and health-care professionals [2]. These infections could be the form of cross-infection, endogenous infection or environmental Infection [1].
The respiratory system and urinary system are the most systems which might be involved by these infections and around 80% - 87% of hospital acquired infections (HCAIs(: “S. aureus”, “Enterococcus species” (e.g. Faecalis, Faecium), “E. coli”, “coagulase-negative Staphylococci”, “Candida species” (e.g. Albicans, Glabrata), “K. pneumoniae” and “Klebsiella oxytoca”, “P. aeruginosa”, “A. baumannii”, “Enterobacter species”, “Proteus species”, Yeast NOS, Bacteroides species [2]. According to the Centers for Disease Control (CDC) and Prevention in the USA about 1.7 million hospitalized patients annually acquire HAI while being treated for other health issues and that more than 98,000 of these patients die due to the Hospital acquired infection (HAI) [3].
There are many factors can increase the risk of HAI including older age, immunosuppression, longer hospital stays, multiple underlying chronic illnesses. However, nearly 20% of all nosocomial infections occur in the intensive care unit [4]. Most of these infections (over 80%) are related to devices’ utilization needed for patients’ life support as ventilator-associated bloodstream infection (BSI), surgical site infection (SSI), and urinary tract infection (UTI) [5]. The increase of both morbidity and mortality related to hospital acquired infections in the intensive care unit (ICU) is a matter of serious problem. For that we hope this study helps to increase awareness of HAI.
1.1. Research Question
What are the potential sources of transmitting hospital acquired infections by routine devices in adult ICU in Alrass General Hospital?
1.2. Research Objectives
1.2.1. General Objective
To determine the potential sources of transmitting hospital acquired infection by routine devises in adult ICU in Alrass General Hospital.
1.2.2. Specific Objectives
1) Collect 3 swabs from each patient from three different devices including: indwelling urinary catheter, mechanical ventilation device and central venous catheter.
2) Culture these swabs in blood agar and MacConkey agar.
3) Identify microorganisms by performing routine microbiological methods, such as gram stain, colony morphology and standard biochemical tests.
4) Determine the most source contaminated with pathogenic microorganisms.
2. Methodology
2.1. Study Design
This is an observational and cross-sectional study, to identify the microorganism and determine the potential source of transmitting of hospital-acquired infection by routine devices in adult ICU in Alrass General Hospital. The study was conducted during the time period of October to November (2019).
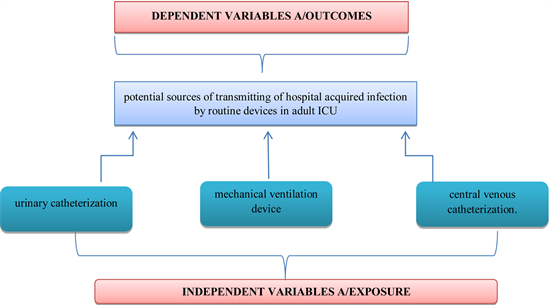
2.2. Conceptual Model of Study
2.3. Materials and Methods
The samples obtained from adult ICU (Intensive care unit) at Alrass General Hospital. Three swabs were taken from the surfaces of an indwelling urinary catheter, mechanical ventilation device and central venous catheter used by every twelve patients in ICU. Other samples are taken per week during October (2019) in the morning period from 10:30-11:30 AM after the cleaning from three patents. The total sample size of swabs is 36.
2.3.1. Isolations of Microorganisms
All swabs were collected by using Amies transport media. Swabs are immediately transported to the laboratory in the same hospital, and streaked on tow media; Blood agar and MacConkey at 37˚C for 24 hrs for colony isolation and morphological identification.
2.3.2. Identification of Organisms
The bacteria isolated and determined by colony morphology with gram-stain. According to gram stain results standard biochemical tests were performed like coagulase, catalase and oxidized [6].
2.3.3. MicroScan WalkAway 96 Pulse
Finally, all samples analyzed by MicroScan WalkAway96 pulse, for further identifications.
MicroScan WalkAway 96 pulse is an automated system which incubates microtiter identification and antimicrobial susceptibility testing panels, interprets biochemical results through the use of a photometric or fluorogenic reader, and generates computerized reports.
3. Ethical Considerations
Ethical approved for this study was obtained from the Regional research ethics Committee of medical education for the research in Alrass Hospital. And also, from the research Revie committee of college of applied medical science, department of medical laboratories in Qassim University.
3.1. Inclusions Criteria
Any adult patients in intensive care unit for more than two days.
3.2. Exclusions Criteria
Patients outside the intensive care unit.
3.3. Data Analysis Plan
Data was entered and analyzed using Microsoft Excel Software. The results were interpreted and presented in Microsoft Word Software using figures, tables and graphs.
3.4. Study Limitations
The study was performed on local hospital and samples size Equal thirty-six.
4. Results
Total of thirty-six swabs were collected from three different devices used by every twelve patients in ICU (Intensive care unit). Bacteria were growth on nineteen plates (52.8%) and six was non-significant count (16.7%). The remaining swabs showed non-bacterial growth (30.5%) From these swabs, nine bacteria were isolated. These organisms include “Klebsiella pneumoniae”, “Acinetobacter baumannii”, “Staphylococcus epidermidis”, “Staphylococcus epidermidis”, “Staphylococcus haemolyticus”, “Escherichia coli”, “Serratia marcescens”, “Pseudomonas luteola”, “Kocurio kristinae” and “Photorhabdus luminscens”.
The most bacteria isolated were “Klebsiella pneumoniae” (18.37%), “Acinetobacter baumannii” (11.48%), “Staphylococcus epidermidis” (4.59%), “Staphylococcus haemolyticus” (4.59%), “E. coli” (4.59%), “sErratia marcescens” (2.3%), “Pseudomonas luteola” (2.3%), “Kocurio kristinae” (2.3%) and “Photorhabdus luminscens” (2.3%) as shown in Table 1.
Total sample: 36 samples, Positive samples: 19 samples.
Proportion of positive samples: 19\36 × 100 = 52.8%.
Table 2 shows that the number of bacteria isolated from the three routine devices used by every twelve patients in ICU. Anyway, the most bacteria isolated were “Klebsiella pneumoniae” followed by “Acinetobacter-baumannii”.
![]()
Table 1. The percentage of bacteria species found in this study.
![]()
Table 2. The isolated bacteria found in routine devices among 12 patients in ICU (intensive care unit).
Figure 1 shows that the indwelling urinary catheter was most contaminated device, twelve bacteria were isolated from nine swabs (75%), tow swabs were non-significant count (16.7%), and only one swab was no growth (8.3%). Following by mechanical ventilator device, nine bacteria were isolated from nine
![]()
Figure 1. The isolated bacteria found in routine devices (indwelling urinary catheter, mechanical ventilation device and central venous catheter). CVC: central venous catheter. MDV: mechanical ventilation device. IUC: indwelling urinary catheter.
swabs (75%), one swab was non-significant count (16.7%), and tow swabs were no growth (8.3%). Finally, the least contamination device was the central venous catheter with only one swab with significant growth (8.3%).
Figure 2 shows that the “Klebsiella pneumonia” was most isolated bacteria on mechanical ventilation device (30%), followed by “Acinetobacter baumannii” (15%), “Staphylococcus epidermidis” (7.5%), “E. coli” (7.5%), “Serratia marcescens” (7.5%), “Photorhabdus luminscens” (7.5%).
Figure 3 shows that the Klebsiella pneumonia was most isolated bacteria (27.7%), followed by “Acinetobacter baumannii” (20.45%), “Staphylococcushaemolyticus” (13.64%), “Staphylococcus epidermidis” (6.80%), “E. coli” (6.80%), “Pseudomonas luteola” (6.80%).
Figure 4 shows that, most swabs taken from CVC (central venous catheter) was negative (no growth) (67%), and about 25% was gram positive non-significant count bacteria. Overall, one swab found to be significantly contaminated with “Kocurio kristinae” (8%).
Table 3 shows that the Enterobacteriaceae species resistance rate to Trimeth\sulfa, Ceftazidime, Ciprofloxacin were 90%, about 70% were resistant to Amp\sulbactam, Imipenem, Pip\tazo and 60% were resistant to Amikacin. On the other hand, Acinetobacter baumannii resistance rate to Ceftazidime, Ciprofloxacin, Imipenem, Pip\tazoand Amikacin was 100%, and about 80% to Trimethyl\sulfa.
5. Discussion
The incidence of hospital acquired infections varies according to the type of hospital and Intensive Care Unit (ICU), the patient population and surveillance techniques used to detect a hospital acquired infection [7]. In each hundred hospitalized patients seven of them inadvanced countries and ten of them in developing countries can acquire one of the health associated infections. Overall, most populations under the risk are patients in Intensive Care Units (ICUs), burn units, organ transplant unit and neonate’s unit [8].
![]()
Figure 2. The isolated bacteria found in mechanical ventilator device. MDV: mechanical ventilation device.
![]()
Figure 3. The isolated bacteria found in indwelling urinary catheter.
![]()
Figure 4. The isolated bacteria found in central venous catheter. CVC: Central Venous Catheter.
There are a large number of microorganisms are responsible for hospital acquired infections and any microbe may have the ability to causes infection in hospitalized patients. However, ninety percent of the HAI (Hospital Acquired Infection) is caused by bacteria, whereas viral, fungal, protozoal are less commonly involved [8] [9].
Depending on Extended Prevalence of Infection in Intensive Care (EPIC II) study, the proportion of infected patients within the intensive care unit (ICU) are often as high as 51%, and the most frequently reported sites for ICU acquired infections were the lungs (64%), abdominal (19%), and bloodstream (15%) [10].
![]()
Table 3. Resistance pattern of most isolated bacteria found in the routine devices against different type antibiotics.
The most common organisms cause ICU-acquired infections are “Enterobacteriaceae” (20%), “S. aureus (20%), “Pseudomonas spp.” (17%), “Enterococcus spp.” (10%) and “Acinetobacter spp.” (5%) [11].
Hospital acquired infections are becoming an increasing problem for hospitalized patients, especially in the ICU, particularly those acquired following the insertion of devices [12]. Anyway, according to the CDC’s National Nosocomial Infections Surveillance (NNIS) system criteria, the three common Device-associated infections are catheter-associated urinary tract infection (CA-UTI), IV catheter-related bloodstream infection (IV-CRBSI), and ventilator-associated pneumonia (VAP) [12].
In Alrass General Hospital, all nurses and staff followed Centers for Disease Control and Prevention (CDC) guideline for preventing a device-associated health-acquired infection. In ICU, cleaning and disinfection are run every morning. However, result of contamination devices in this study shows that, in a total of thirty-six swabs from the three devices, bacteria were grown on 19 plates (52.8%) and 6 were non-significant count (16.7%). The remaining swabs showed no bacterial growth (30.5%).
In our study the most organism founded was members of the “Enterobacteriaceae family”, such as “Escherichia coli”, “Klebsiella pneumoniae” and “Serratia marcescens”, followed by “Acinetobacter baumannii” and “Coagulase-negative staphylococci”. According to CDC these bacteria were reported as common bacteria that cause hospital-acquired infections [11].
Depending on the data of the infection control department in Alrass General Hospital, in the period from January to October (2019) there were 16 cases of hospital acquired infection in ICU. The most causative bacteria were “Klebsiella pneumoniae” in four cases (25%), “Acinetobacter baumannii” in three cases (18.75%), “Serratia marcescens” in three cases (18.75%), and one case of “Staphylococcus haemolyticus” (6.25%), “Staphylococcus aureaus” (6.25%), “Protous mirabilis” (6.25%), “Pseudomonas stutzeri” (6.25%), “Klebsiella oxytoca” (6.25%).
During this period central line-associated blood stream infections (CLABSI) was most common device-associated infections, following by ventilator-associated pneumonia (VAP) then catheter-associated urinary tract infections (CAUTI), these results differ from Al-Tawfiq et al. study, which was the catheter-associated urinary tract infections the most common [13].
In our study the most bacteria isolated were “Klebsiella pneumoniae” followed by “Acinetobacter”. These results are correlated with most causative organisms reported by infection control department in Alrass General Hospital.
Tao L et al. found that the most organism isolated from a patient with devices associated infections were “Acinetobacter baumannii” (19.1%), followed by “Pseudomonas aeruginosa” (17.2%) and “Klebsiella pneumoniae” (11.9%), these results slightly resemble to our finding [14].
Our finding is consistent with a result of a study performed on Brazilian hospitals to measure the device-associated infection, the “Enterobacteriaceae” were the most isolated bacteria and “Acinetobacter spp.” and “Coagulase-negative staphylococci” (8.4%) were also significant [15]. Weinstein, R et al. reported that the gram-negative bacilli were associated with 23.8% of blood stream infections (BSIs), 65.2% of pneumonia episodes, 33.8% of surgical site infections (SSIs), and 71.1% of urinary tract infections (UTIs) [16].
In our study the indwelling urinary catheters were the most contamination device, they were significantly contaminated with “Klebsiella pneumonia” (27.27%), which slightly resemble the result of Nicolle, L [17].
Mechanical ventilator devices were the second most contamination device, the most microorganisms found are gram-negative bacilli (67.5%), followed by coagulase-negative staphylococci (7.5%), the result looks like to most bacteria isolated from ventilator-associated pneumonia patients in Weinstein R et al. study which found gram-negative bacilli 58% [15].
The resistance patterns of organisms isolated in the present study are compared with those reported by Cuellar L. et al. and Afhami S. et al. studies, in our study the Enterobacteriaceae resistance to Ceftazidime and Pip\tazoaremore than that in Cuellar L. et al. study and Acinetobacter strains resistance to ceftazidime and Amp\sulbactam are more than that in Afhami S. et al. study [9] [18].
5.1. Prevention and Control of Hospital Acquired Infections
Hospital acquired infections can be controlled by practicing infection control programs, keep a check on antimicrobial use and its resistance and adopting antibiotic control policy. An efficient surveillance system guided by the World Health Organization (WHO) can help healthcare institutes to devise infection control programs [8]. All health workers are responsible, they must work together to reduce the risk of infection for patients and staff. However, Infection control programs are cost-effective, but their application is often hindered by an absence of support from administrators and poor compliance by doctors, nurses, and other health workers [19].
5.2. Central Line-Associated Blood Stream Infections Prevention
Center for Disease Control and Prevention (CDC) identified Strategies for prevention of ClBSI which includes the following:
1) Educating and training health care providers who insert and maintain catheters.
2) Using maximal sterile barrier precautions during CVC insertion.
3) Using a 2% chlorhexidine preparation for skin antisepsis.
4) Avoiding routine replacement of CVCs as a strategy to prevent infection.
5) Using antiseptic/antibiotic-impregnated short-term CVCs if the rate of infection is high despite adherence to other strategies [20].
5.3. Catheter-Associated Urinary Tract Infection
The strategies for the prevention of CAUTI are divided into basic practices of insertion, maintenance, and removal. In insertion, the medical staff assess for medical necessity and appropriateness of device, use aseptic insertion technique and sterile supplies and apply securement device to prevent movement and traction. The next step is maintenance which includes the hands preserve sterile, continuous closed system and regularly empty drain bag by using a patient-dedicated collection container. Finally, remove it when no longer medically necessary [21].
5.4. Ventilator-Associated Pneumonia (VAP) Prevention
CDC recommendation practices for prevention of VAP including the following:
1) No routine changing of humidified ventilator circuits.
2) Periodically draining and discarding condensate collecting in the ventilator tubing.
3) Changing the heat-and-moisture exchangers when they malfunction mechanically become visibly soiled [22].
6. Conclusion
This study detects a high contamination of routine devices and resistant organisms and appropriate interventions are necessary to reduce these rates. Indwelling urinary catheters were the most contaminated devices followed by mechanical ventilator devices; the less one was central venous catheters. The most organisms isolated resemble those reported by the infection control in Alrass General Hospital as the most curative organism of HAI. Depending on these results we suggest that the routine devices used in intensive care unit in Alrass General Hospital may consider as a source of transmitting of HAI.
Recommendations
1) Effective infection control practices and effective strategies to control antibiotic-resistant bacteria should be applied.
2) Recommend more surveillance system guided by WHO in KSA hospitals。
3) Recommended more researches on HAI in the Middle East.
Acknowledgements
I would like to thank the staff and management of Alrass General Hospital, especially the infection control department and staff of the Microbiology Laboratory for space and their help to undertake this study. I would also like to extend my appreciation to the ICU nurses and to Dr. Amal Sulaiman and Dr. Sara Aliin Qassim University—Microbiology Department.