Thermal Microcautery, a Form of Peripheral Nerve Field Stimulation for Treatment of Painful Knee Osteoarthritis: Non-Randomized Controlled Trial ()
1. Introduction
Chronic pain conditions are disabling to patients’ quality of life including the patients’ capacity to carry out day to day activities which require physical activity. Managing chronic pain poses difficulties and challenges, regardless of whether pharmacological or non-pharmacological methods are employed. Pharmacological treatments in pain management, however, can have multiple and varied side effects [1]. Painful knee osteoarthritis (PKO) is linked to severe morbidity [2], thus management of such conditions is important. The general recommended treatment for patients who suffer from osteoarthritis of the knee is firstly to use topical NSAIDs, followed by paracetamol as a form of rescue treatment if the patient still feels pain. Topical NSAID treatments are utilized so widely with a low risk:benefit ratio; however, the risks of their uses are yet to be elucidated [2] [3]. Nevertheless, NSAIDs as peroral medication have a variety of associated side effects including, gastric [4], and renal [5] side effects. Further medication treatment often leads to the use of opiates for chronic pain management, with little to no effect on the neuropathic element of pain [6]. Opioid related problems such as tolerance, resistance and opioid induced hyperalgesia and further risks when combined with anti-depressants or anticonvulsants can be problematic [6] [7].
The non-pharmacological modalities and interventions for PKO can be invasive with risk of complications and costs, thus a search for new modalities for managing chronic pain is still required. Total knee replacement (TKR) is offered to long term sufferers. The procedure is costly, often coincides with pharmacological treatment and can have serious adverse complications. Neuromuscular exercise programmes have been offered as one potential alternative [8] [9] [10], however the likelihood of noncompliance to a recommended physiotherapy to be sustained is common [11].
Agni-karma is a known technique in Ayurveda (an Indian system of Medicine) that employs thermal microcautery to the skin over painful areas for the treatment of severe chronic pain [12]. The microcautery is applied to the point of maximum pain through the angled and tapered tip (pin-point) of a metal rod after heating over an open flame until it is red. Quick touch application for about 0.3 - 0.5 seconds over the target skin point produces a second degree burn with an area of about 1 mm in diameter. A soothing cream is immediately applied, and healing is allowed over a period of two weeks.
Agnikarma, has been evaluated in several studies to treat some chronic pain conditions such as painful knee osteoarthritis [13] [14], sciatica [15] and tennis elbow [16] with a high clinical success rate in managing these chronic pain conditions.
Heat therapy [17] [18] and neuromodulation techniques such as Peripheral Nerve Field Stimulation (PNFS) by electricity [19] [20] [21] are known methods of pain management. Peripheral nerve field stimulation (PNFS) is the stimulation of unnamed small nerves in the vicinity of pain by superficial, subcutaneous lead placement. Explanatory theories for the mechanism of PNFS by thermal microcautery in treating pain include; firstly, resetting the descending inhibitory pathway (DIP) as burn induced inflammation stimulates DIP [22] [23] producing an immediate relief of pain; secondly, deeper burns invariably damage the nerve endings with possible prevention of transmission of any further painful stimuli originating from the original chronic pain source. As the nerves recover, the pain symptoms recur and hence the need for repeated microcauterization to jump the descending inhibitory pathway again. PNFS-TMC is a thermal microcautery that does not produce much burn (with regard to both surface area and depth of burn) so, maybe these proposed mechanisms are not valid to explain the beneficial effects of PNFS-TMC (Agnikarma) [13] [14] [15] [16] [24].
Other explanations for the mechanism of PNFS-TMC in treating chronic pain may include the Gate Theory of Pain [25], the role of the local capsaicin receptor TRVP1 [26], alterations in the signaling within the Dorsal Root Ganglion (DRG), which is now a target for focal neuromodulation [27] or, that chronic pain alters the brain maps of the affected dermatome area on the sensory cortex analogous to mechanisms proposed by Herta Flor [28] [29].
Further mechanisms explain the beneficial effects of Agni-karma may relate to the connections of both peripheral and central mechanisms related to offset analgesia (OA) [30] where the application of a peripheral heat produces an analgesic effect through a temporal filtering of the supplied nociceptive information to the CNS. OA results in decreased activity in SI (primary somatosensory cortex), but is accompanied with higher activation in the inferior parietal lobule, intra-parietal sulcus, anterior insula and dorso-lateral prefrontal cortex [31].
The first and fourth authors of this paper have personal experience of working in India with an Indian based Agni-karma group. The authors were impressed with the immediate and long-term outcomes of using Agni-Karma in chronic pain conditions in India. The clinical studies on PNFS-TMC, however, are not numerous [13] [14] [15] [16], therefore more structured clinical studies are needed to assess and validate PNFS-TMC as a modality in the management of chronic pain.
The purpose of the current study is to assess the efficacy and the safety of using Peripheral Nerve Field Stimulation by Thermal Microcautery (PNFS-TMC) technique to manage cases with painful knee osteoarthritis.
2. Methods
The study was approved by the Research and Ethics Committee at Adelaide and Meath incorporating National Children’s Hospital-AMNCH (Tallaght University Hospital). REC reference: 2016-10 Chairman’s Action (3) (Appendix 1) and the trial was registered after recruitment of the targeted sample size (ClinicalTrials.gov Identifier: NCT03460717-Registration date: 9th of March 2018). The research was conducted in accordance with the regulations and guidelines of the European Network of Research Ethics Committees.
The study was designed as a non-randomized controlled trial. The technique of PNFS-TMC was introduced for the first time in Ireland and as a result, randomization was not possible. Patients with Painful Knee Osteoarthritis (PKO) who were waiting for TKR were offered PNS-TMC in addition to the standard analgesic care (Appendix 2).
All PKO patients with expected waiting time for TKR > 6 months were offered PNFS-TMC following full explanation of the technique including its benefits and risks including any possible complications. A website for the Global Agni-karma group (http://globalagnikarma.com) was supplied to the patients as an educational tool to educate patients about the technique. An additional information leaflet was provided (Appendix 3). Information was supplied to the patients through an initial phone call and then through a face to face meeting in the hospital following primary declaration of interest in the idea of PNFS-TMC.
All patients provided written informed consent for participation in the study (Appendix 4). Patients were allocated to one of two groups: 1) Intervention group; included patients who agreed to receive PNFS-TMC in addition to the standard WHO stepladder analgesics. 2) Control group; included patients who declined to have PNFS-TMC and decided to receive only the standard WHO stepladder analgesics.
Inclusion criteria:
Patients who agree to receive PNFS-TMC to be included in the intervention group.
Patients who declined to receive PNFS-TMC to be included in the control group.
History of painful knee osteoarthritis is >2 years diagnosed by the Orthopedic service.
Planned TKR to be >6 months after time of recruitment of the patient.
Intact healthy skin over and around the knee joint.
Exclusion criteria:
Patients who decline PNFS-TMC to be excluded from the intervention group.
History of painful knee osteoarthritis is <2 years or the presence of any other causes for painful knee in addition to the osteoarthritis.
Planned TKR to be <6 months after time of recruitment of the patient.
Inability to apply PNFS-TMC to the skin over and around the knee joint due to infection or inflammation.
A total of 46 patients from the list of TKR patients on an orthopedic waiting list were phoned and offered participation in the study. 16 patients declined PNFS-TMC and were subsequently included in the control group, 30 patients agreed to receive PNFS-TMC and were included in the intervention group. 14 patients out of 30 patients in the intervention group could not complete 4 sessions, these patients were excluded from the analysis. 16 intervention group patients were therefore subject to analysis (Figure 1).
2.1. Intervention: PNFS-TMC
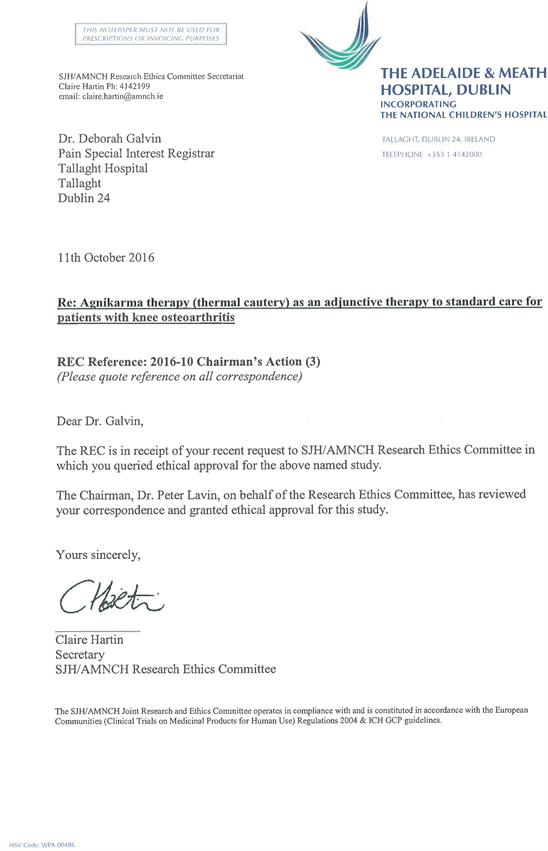
The intervention group patients were scheduled to have 4 sessions, 2 weeks apart, over a period of 8 weeks. During each session, the most painful points over the knee joint on palpation were determined, marked and recorded and treated as “points of tenderness”. Skin sterilization was not utilized before the procedure as temperature used (371˚C - 649˚C) was sufficient to destroy even prions which will denature at 135˚C [32]. The pin pointed tip of the metal rod (Shalaka), which is composed of Brass (a metal alloy of copper and zinc) was heated over an open naked flame for 5 minutes, until the tip became red in color (Figure 2). The temperature of the heated rod lies within in the range of 371˚C - 649˚C. Each marked skin point was touched with the pin point tip of the hot metal rod for 0.3 to 0.5 second. The aim was to produce a micro second-degree burn, with an area of about 1 mm in diameter and a depth of less than 1 mm. Immediately following removal of the hot metal rod away from the skin, the burned point was covered by a soothing herbal cream to alleviate any pain caused by the treatment. The cream was herbal based [Burncool cream—license number (India) GA/1555—Pistacia lentiscus 0.2%, Shorea robusta 9%, Sesamum indicum 15%, coconut oil 15%, bees’ wax 2% and water QS (Quantum Satis)]. Patients reported that the cream immediately cools the burned area and therefore makes the treatment acceptable for the patient (Video 1).
![]()
Figure 2. Upper left; the metal rod or Shalaka made of Brass, alloy of copper and zinc. Upper right; the pointed tip of the metal rod used to apply PNFS-TMC. Lower right; the metal rod is suspended with its tip in open flame. Lower left; the tip heated until it is red.
Video 1. Each marked skin point was touched with the pin point tip of the hot metal rod for 0.3 to 0.5 second. The aim was to produce a micro second-degree burn, with an area of about 1 mm in diameter and a depth of less than 1 mm. Immediately following removal of the hot metal rod away from the skin, the burned point was covered by a soothing herbal cream to alleviate any pain caused by the treatment. The cream was herbal based [Burncool cream—license number (India) GA/1555—Pistacia lentiscus 0.2%, Shorea robusta 9%, Sesamum indicum 15%, coconut oil 15%, bees’ wax 2% and water QS (Quantum Satis)]. Patients reported that the cream immediately cools the burned area and therefore makes the treatment acceptable for the patient.
The procedure was repeated for other marked painful points. The central line for the future standard surgical incision for TKR was totally avoided. These painful points could vary between sessions both in nature and location. They are defined as points of maximum tenderness within an area of allodynia. The boundaries of the area of allodynia were defined first by palpation and then within that demarcated area the precise pain points were agreed upon by the patient.
In cases where the patient had two affected knees the procedure was applied to the worst affected knee before the second to mimic the order of treatment that would be given during knee replacement.
The thermal micro-cautery was applied by author one in all cases (previous training in the procedure had taken place at the Global Agni-karma Centre).The same instrument was used for all patients. All fire safety precautions were taken.
All patients were advised to continue their normal therapy and to use this intervention as an adjunctive therapy. In a similar fashion, control patients were advised to continue their normal therapy.
2.2. Data Collection
Data was collected from patients in both groups. The primary outcome was change in VAS pain score which was recorded twice. Initially a baseline VAS was recorded at the time of recruitment (before any intervention), and then again after 8 weeks (i.e. after 4 sessions in the intervention group and 2 weeks after the last session).
VAS pain score was obtained verbally by a phone call in the control group, after explaining the score to the patients. Secondary outcomes were recorded subjectively. Changes in daily activity (improved, worsened or no change), changes in sleep quality (improved, worsened, no change) and changes in analgesics usage (increased, decreased, no change). Data was collected both over the phone and during the sessions.
2.3. Sample Size Calculation
We hypothesized a 50% reduction in VAS pain scores for patients with PKO who received PNFS-TMC (Agni-karma) as a primary outcome [13] [14]. Allowance was made for a type one alpha error of 0.05, power 0.9 with a smallest effect size of 40%, standard deviation 10. Based on this data, a power of 32 patients was established with 16 patients in each group. Sample size calculation was estimated by using G*Power software version 3.1.9.2 (Institute of Experimental Psychology, Heinrich Heine University, Dusseldorf, Germany).
2.4. Statistical Analysis
Data of patients’ characteristics were compared by independent t-test. Other categorical variables were evaluated by chi-square test or Fisher’s exact test when appropriate. All values expressed as mean ± standard deviation, median (interquartile range), or number of participants (percent) as appropriate. A P < 0.05 was considered statistically significant. Statistical analysis was performed using MedCalc Statistical Software version 17.7.2 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2017).
3. Results
The trial was carried out in the period from December 2016 to August 2017. A total of 46 patients with PKO and expected waiting time for TKR > 6 months were offered to receive PNFS-TMC in addition to routine care. 16 patients declined PNFS-TMC and were assigned to the control group with one patient lost to follow up during the 8 weeks follow up. 30 patients agreed to have PNFS-TMC. 17 patients completed all 4 sessions. One patient was lost to follow up after the fourth session. Data from 16 patients in the intervention group and 15 patients in the control group were analysed (Figure 1).
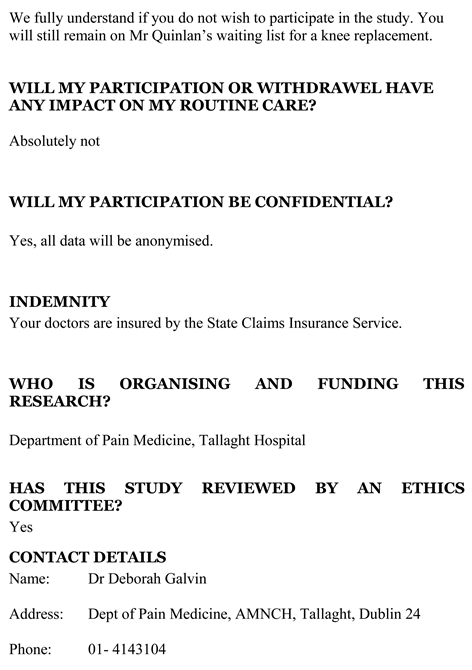
16 (14 female) patients completed 4 sessions of PNFS-TMC—Mean age 64.76 (SD 9.98). 15 (13 female) patients were followed in the waiting list control—Mean age 71.56 (SD 9.82) with no significant difference between the groups in age nor gender distribution (Table 1).
The baseline VAS score was significantly higher in the PNFS-TMC group than in the Control group [9 ± 1.23 (95% CI 8.38 to 9.61) versus 5.93 ± 2.11 (CI 95% 4.81 to 7.06) respectively with P < 0.0001] (Table 1).
The VAS score after 8 weeks (i.e. 4 sessions), was significantly lower in the PNFS-TMC group than in the Control group [4.64 ± 2.08 (95% CI 3.57 to 5.72)
![]()
Table 1. VAS score in intervention and control groups.
VAS: Visual Analogue Score. P value < 0.05 is considered statistically significant.
versus 6.73 ± 2.01 (95% CI 5.61 to 7.85) respectively with P = 0.0058] (Table 1).
In the PNFS-TMC group, VAS score decreased significantly from 9 ± 1.23 (95% CI 8.38 to 9.61) at baseline to 4.64 ± 2.08 (95% CI 3.57 to 5.72) after 4 sessions (P < 0.0001). While in the control group, VAS score showed a non-significant increase in VAS score from 5.93 ± 2.11 (CI 95% 4.81 to 7.06) to 6.73 ± 2.01 (95% CI 5.61 to 7.85) after 8 weeks (P = 0.2844) (Table 1).
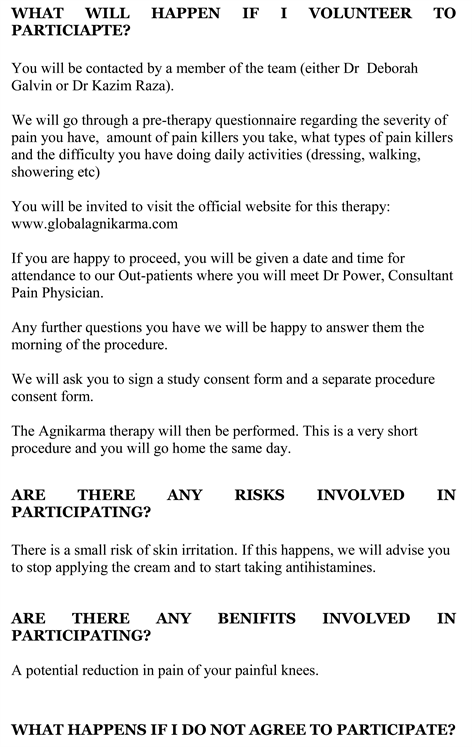
The majority of Patients in the PNFS-TMC group experienced improved daily activity, compared to none of the patients in the control group (11 patients (68.7%) versus 0% respectively, P < 0.0001). None of the PNFS-TMC patients reported worsening of daily activity versus 5 patients (33.3%) in the control group, P < 0.0001. The majority of patients [10 patients (66.7%)] in the control group had no change in daily activity versus 5 patients (31.2%) in the PNS-TMC group, P = 0.0418 (Table 2).
The majority of patients in both groups showed no change in sleep quality [62.5% in PNFS-TMC group versus 80% in control group, P = 0.3018], 6 patients (37.5%) in PNFS-TMC group had improved sleep versus none in the control group (P < 0.0001). 3 patients (20%) had worsening of sleep quality versus none in the PNFS-TMC group (P < 0.0001).
About the analgesic requirements, most patients in both groups experienced no change in analgesic needs (15 patients (93.7%) in PNFS-TMC group versus 13 patients (86.7%) in the control group, P = 0.5171) (Table 2).
In the PNFS-TMC group: 6 patients (40%) were interested in having more sessions, while 9 patients (60%) were not interested in having more sessions. However out of these 9 patients, 4 patients (26.66%) were not interested because satisfaction of the level of pain relief. 2 patients (12.5%), out of the 16 patients in the Intervention group cancelled their TKR as pain level decreased to a satisfactory level (Table 3).
Regression analysis showed a significant correlation between best pain score after 4 sessions and activity after 4 sessions in PNFS-TMC group (R2 = 0.006, P = 0.0285).
![]()
Table 2. Secondary outcomes in intervention and control groups.
*: P value < 0.05 is considered statistically significant.
![]()
Table 3. Outcomes in the intervention group.
4. Discussion
The current trial shows that Peripheral Nerve Field Stimulation by Thermal Microcautery (PNFS-TMC), otherwise known as Agni-Karma in Ayurvedic medicine, is potentially effective when used as an adjunct to standard WHO stepladder analgesics in managing chronic pain due to knee osteoarthritis. PNFS-TMC significantly reduced VAS by about 50% (P < 0.0001) after 4 sessions as compared to control patients who experienced mild non-significant increase in VAS (P = 0.2844) after the same period. Interestingly, although PNFS-TMC group had a significantly higher baseline VAS than the control group [9 ± 1.23 (95% CI 8.38 to 9.61) versus 5.93 ± 2.11 (CI 95% 4.81 to 7.06), P < 0.0001], PNFS-TMC patients achieved a significantly lower VAS than the control group after 8 weeks [4.64 ± 2.08 (95% CI 3.57 to 5.72) versus 6.73 ± 2.01 (95% CI 5.61 to 7.85) respectively with P = 0.0058].
PNFS-TMC resulted in improved daily activity in a majority of patients (68.7%) which did not happen with any patient in the control group (P < 0.0001). PNFS-TMC was associated with improved sleep in 6 patients (37.5%) which did not happen with any patient in the control group (P < 0.0001). None of the patients who received PNFS-TMC experienced deterioration in sleep nor daily activity. Both groups declared comparable analgesic consumption.
The current study presents evidence of the clinical effect of PNFS-TMC (Agnikarma) for the relief of pain in patients with knee osteoarthritis who are on a waiting list for TKR. We document a 50% reduction in pain score after 4 sessions of therapy delivered over an 8-week period. Of note, the interventional group had a higher initial VAS score, this might be due to more osteoarthritis and more pain or it might be due to poor response of these patients to medications. The higher baseline VAS of the intervention group patients may be their reason to accept participation in the study. PNFS-TMC significantly reduced this high VAS score when compared to the control patients which suggests the efficacy of PNFS-TMC. The analgesia induced by PNFS-TMC was associated with improved activity and sleep. Two patients cancelled their TKR due to satisfaction with the level of pain relief and improved activity. This was an unexpected outcome but hints at the potential pain relief capacity of the technique for some.
It is a standard teaching in Pain Medicine that improvements in pain scores which are subjective need to be linked with improvements in function. An example of this would be, the support for a prescription of opioids in chronic pain would follow documentation of a 50% improvement in pain associated with better function in the activities of daily living in an initial trial of therapy. This philosophy permeates into acute post-operative medicine also, where fast track rehabilitation strategies post-operatively attempt to combine the improved pain scores and thus improved the pain management of recovery. Improved function, sleep and stable medication in the interventional group were also recorded. These findings support the primary outcome’s finding of a pain score reduction after 4 sessions by framing it with meaningful improvements in quality of life as measured by improvement in daily activities and some with better sleep quality. These results are in stark contrast to the status quo of knee pain sufferers, including when compared to the deterioration expressed by the control group. It is interesting to note that the comparative waiting list control group deteriorated during their period of waiting. There was no meaningful difference in the use of medication, however, patients were not asked to alter their medication as such an instruction might be unethical without having enough valid evidence for analgesia through Agnikarma. A future design with PRN medication use option might explore this issue further.
The objective of studying Agni-karma is both to document benefits worthy of further investigation and to stimulate a conversation about possible mechanisms of action so that a further hypothesis can be generated. Indeed, the possibility of a better understanding of mechanism might offer a pathway to new treatments.
The pre-requisites for Thermal Microcautery to work seem to be; 1) Presence of maximal pain points or focal points of tenderness. 2) Acute second degree burn to the area. 3) Treatment probably repeated at 1 - 2-week intervals, most effective when completed over several sessions. 4) An early treatment effect which could start within hours of the initial burn.
Heat treatment has evidently managed chronic pain in other instances [13] [14] [15] [16] [24]. A possible explanation of the mechanism by which PNFS-TMC produces such analgesic effects includes peripheral nerve field stimulation by heat [30].
Pain itself has two features, temporal and spatial [33]. The analgesic effect of CPM (Conditioned Pain Modulation) has been linked to filtering of the spatial feature while the OA (Offset Analgesia) has been linked to filtering through temporal features [30] [31] [34]. One explanation proposed has been that heat effects CPM [35]. This mechanism may not be applicable to PNFS-TMC as CPM does not happen if the time of stimulation is shorter than 20 seconds [36] while the time of PNFS-TMC is 0.3 - 0.5 s. To further add to this; the nature of the burn produced by PNFS-TMC (a micro second degree burn) favors the concept of offset analgesia (OA) [30] [31] [34] as a possible explanation for the effectiveness of PNFS-TMC in managing pain conditions.
OA depends on applying two different temperatures peripherally which is applicable to PNFS-TMC as there are two different temperatures, an initial high temperature (371˚C - 649˚C) followed by a lower temperature induced by application of cold soothing cream (room temperature 20˚C). Although, OA is mainly connected to filtering the temporal component of pain [23], recent studies [30] [33] [34] suggested that OA has a spatial component in addition to the temporal component. OA can be applied on the findings in our study, where the spatial component can be due to superficial stimulation (burn by PNFS-TMC) coupled with deep stimulation by signals from deeper inflamed tissues. The temporal component arises due to the time difference between the two temperatures applied during PNFS-TMC (371˚C - 649˚C followed by 20˚C).
The finding of a greater improvement from the high VAS intervention group was interesting. It is possible that people with a higher pain perception may have a higher sensitivity to peripheral nerve field stimulation, regardless of the mechanism through which pain alleviation operates.
The VAS score showed a non-significant increase in the control group. A possible explanation is the progressive deterioration in knee osteoarthritis with the patients’ daily activity or natural variability in a chronic condition for which analgesia is not consistently efficacious.
OA has been proved to be non-dependent on either ketamine [36] [37] nor opioids [37]. A functional MRI study [31] showed that OA produces a significant reduction in pain intensity associated with decreased activity in SI (primary somatosensory cortex), but is accompanied with higher activation in the inferior parietal lobule, intraparietal sulcus, anterior insula and dorso-lateral prefrontal cortex [38] [39].
Our preferred modern descriptive term is “Peripheral Nerve Field Stimulation by Thermal Microcautery”. This captures the necessity to find peripheral maximal pain points within the painful area which do not relate to an anatomical area and seem to represent a field of painful activity. Such an area has a neural and perhaps ultimately, a brain link. The repetitive nature of the intervention categorizes it as stimulation—karma in the original title translates as action. Cautery is descriptive for the intervention and loyal to the traditional name of the procedure (Agni translates as fire). Together the total descriptive term fits with the modern concept of peripheral nerve field stimulation which attempts to modulate the peripheral nerve field by electric means as opposed to our traditional stimulation by thermal microcautery.
We took the view that 4 sessions were a reasonable number, however, patient populations that do not normally attend a Pain Clinic showed a trend in lack of completion. A significant number of patients failed to stay in the study to complete 4 sessions of therapy. We looked at their reasons for withdrawal as documented in the results section which included 2 who received no improvement after two sessions. Other patient withdrawals occurred despite documented improvements. Some patients were lost to follow up after one session. Our primary objective was to calculate VAS after 4 completed sessions. We therefore only considered those results to test the hypothesis that 4 sessions of Agni-karma would demonstrate a positive trend in pain relief.
Our results agree with the few clinical studies published on the use of Agni-karma in different conditions of pain as PKO [14], sciatica [15] and tennis elbow [16]. The Agni-karma for the PKO studies [14] was delivered in a traditional manner for knee pain using two different temperatures. One technique applied the heat to the brass instrument for 5 minutes pre-application. The other time period of heating the instrument was longer, heating for 15 minutes pre-application. Interestingly, they revealed a greater effect of Agnikarma with higher temperature (longer heating). Our set up is was akin to the lower temperature, we waited approximately 5 minutes pre-application. The precise temperature of the probe was not the focus of this study however the tip of metal rod was red in colour before application to the skin. They also used a 4-session model and studied two groups of 28. In their overall assessment they recorded that over 50% of their patients had improved pain scores.
None of our patients reported any complications related to the thermal microcautery applied to the skin with almost complete healing of the induced second degree burn. This may be due to the brief contact with the skin (0.3 - 0.5 second) and the very small area of burn (about 1 mm).
There is certainly an art in the degree of pressure to apply which is shown in the video (Video 1) which demonstrates the procedure. We did not instruct the patients to reduce the analgesia doses that they were regularly taking for PKO because we did not have certainty about the effect of PNFS-TMC. Future studies may include such instructions and measurement of the analgesic requirements.
5. Conclusion
PNFS-TMC may offer a simple, safe, cheap and effective method to manage chronic painful knee osteoarthritis. The effects of PNFS-TMC were reflected by significant improvements in pain score, activity and sleep with none of the patients experiencing any complications. Further studies including larger sample size with different pain conditions are required. Future studies may include functional MRI to further investigate the possible mechanisms of PNFS-TMC.
Limitations and Future Studies
One of the limitations of the current study is that it is a non-randomized trial which could undermine the validity and generalizability of our results. Due to the novel nature of the intervention, and it being used in clinical practice for the first time in Europe, we had to offer PNFS-TMC to our patients and allocate patients who agreed to the intervention group and patients who refused to the control arm. This is partially compensated by having a control arm to which the intervention has been compared.
Another limitation was the use of a probe heated for a period of 5 minutes only for PNFS-TMC. Additionally, our trial did not analyze precisely the analgesia consumption by the patients.
Another limitation of our trial is that it is a single center trial and recruited a relatively small sample size for a limited number of sessions. Our sample size is comparable to Jethava, N.G. et al. [10] who examined Agni-karma on 28 patients with PKO, however a more comprehensive study would be required to derive reproducible conclusions.
Data derived from this trial will be used to plan for another trial which will assess the use of PNFS-TMC in different localized pain conditions such as back pain, shoulder pain and knee pain.
Acknowledgements
The authors acknowledge; Vaidya Asvin Barot (UK) for research rediscovery and development of concept. Also, Global Agnikarma Centre, Ahmedabad, Gujarat, India—Vaidyas Hitesh Chauhan, Hardik Darji, Krishna Patel, Hetal Chauhan, staff and patients for clinical access, training and the educational website. Finally, Consultant Orthopedic Surgeons at Tallaght University Hospital, Dublin, Ireland. Mr. John Quinlan and Mr. Tom McCarthy—for allowing the authors to access their waiting lists of patients for TKR.
Data Availability
Data will be available upon reasonable request.
Institutional Attribution of the Work
Department of Pain Medicine, Tallaght University Hospital, Trinity College, University of Dublin, Ireland.
Authors Contributions
1) Camillus K. Power:
Study design, clinical application of the technique, supervision of the research, writing the primary manuscript, revision and approval of the final manuscript.
2) Deborah Galvin:
Application for Ethical Committee approval, data collection, revision and approval of the final manuscript.
3) Tagarisa Foto:
Patients recruitment and follow-up, data collection, revision and approval of the final manuscript.
4) Ahmed Abdelaal Ahmed Mahmoud:
Data analysis, participated in study design, revision and approval of the final manuscript.
5) Nikolaos G. Kostopoulos:
Revision and approval of the final manuscript.
Research and Ethics Committee Approval
The study was approved by REC at Tallaght University Hospital (Adelaide and Meath incorporating National Children’s Hospital) on the 11th of October 2016. REC Reference: 2016-10 Chairman’s Act (3).
Trial Registration
ClinicalTrials.gov Identifier: NCT03460717; Date of clinical trial registration: 9th of March 2018.
Appendix 1. Ethical Committee Approval
Appendix 2. WHO 3-Step Analgesic Step Ladder

Appendix 3. Patient Leaflet Template
Appendix 4. Consent Form