Extracranial Internal Carotid Artery (ICA) Aneurysm Repair and End to End Anastamosis of the Artery ()
1. Introduction
Extracranial carotid artery aneurysms are uncommon and occur in a broad range of patients due to many etiologies. True aneurysms involving all layers of the carotid arterial wall and false aneurysms both occur. Overall, extracranial carotid artery aneurysm accounts for less than 1 percent of all arterial aneurysms and approximately 4 percent of peripheral artery aneurysms [1] [2] [3] . Repair of extracranial carotid artery aneurysm represents 0.2 to 5 percent of carotid procedures depending upon the reporting institution [4] . We present a case of extracranial ICA aneurysm, successfully operated in our institution with resection and end to end anastomosis of the same artery.
2. Case Report
A 37-year-old male, presenting with a painful swelling on the right side of the neck, with the deviation of the tongue to the opposite side is presented. He had a Doppler test done elsewhere which showed aneurysmal mass at the level of right carotid bifurcation extending superiorly with displacement of neck vessels. Heterogeneous signal on Doppler, suggestive of aneurysm (with active flow) noted in the upper neck originating from the distal cervical ICA which is placed posteriorly in the carotid space compressing and displacing proximal ICA and its branches. CT angiogram confirmed the diagnosis (Photo A), showing the aneurysmal sac of the cervical ICA and the entry and exit vessels from it.
He underwent resection of right Internal Carotid Artery Aneurysm and end to end anastomosis of the internal carotid artery segments. The incision extended from the angle of the mandible to the sternal notch parallel to right sternocleidomastoid muscle. The swelling was 5 × 5 × 6 cm and the aneurysm was stretching both the external and internal carotid away from each other. Internal carotid artery was seen extending along the aneurysm and draining at the superior pole of the aneurysm (Photo B-1). This part had to be dissected from under the mandible to visualize the distal portion of the cervical segment of the internal carotid artery (Photo B-2). The common carotid artery was exposed. The external carotid was seen plastered and running medial to the aneurysm. The hypoglossal nerve was found stretched across the aneurysm. The exit limb of the internal carotid artery was found at the superior pole of the aneurysm. As the sump pressure of the distal end of ICA was less than 8 mm of Hg it was decided to insert a shunt into the internal carotid artery. The proximal limb of the shunt was inserted into the Internal Carotid and the distal end was inserted into the
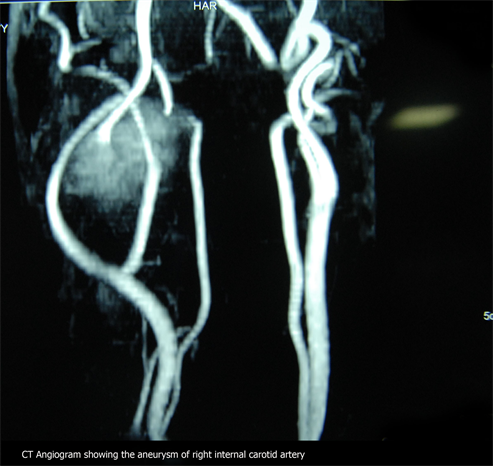
Photo A. CT angiogram showing the aneurysm of the left ICA.

Photo B. The surgical photographs showing each stage of the procedure as written under each photo.
distal part of the internal carotid after opening the aneurysm. The proximal limb of the internal carotid artery was disconnected from the aneurysm at its entry. This limb was then anastomosed to the area of distal internal carotid artery through which the shunt had been inserted distally (Photo B-3). The anastomosis was performed using 6.0 polypropylene suture (Photo B-4). The shunt removed. Hemostasis attained and wound sutured in layers with a drain.
The patient was shifted to ICU in a stable hemodynamic condition. He had an uneventful post-operative stay in ICU and was shifted to the room on the third postoperative day. He was later discharged in good health. He was reviewed after one year and was in perfect health.
3. Discussion
Carotid artery aneurysms have various aetiologies and represent a taxing pathology with limited expertise and familiarity. The most common cause of extra cranial carotid artery aneurysms is atherosclerosis. These aneurysms tend to be fusiform and are almost always associated with arterial hypertension. Extra cranial carotid aneurysm repair comprises 0.1% to 2% of all carotid procedures [5] [6] . The high incidence of cranial nerve compression and cerebrovascular events through embolization in untreated patients (68%) justifies invasive management for both symptomatic and asymptomatic carotid aneurysms [7] . Haemorrhage has also been seen as a complication of these aneurysms, although rupture remains uncommon. The surgical techniques applied to the management of extra cranial carotid aneurysms are ligation (or angiographic occlusion), endoaneurysmoraphy, resection with primary anastomosis, resection with graft replacement, or stent grafting. In the era of endovascular surgery, techniques used for occlusive disease are extrapolated as minimally invasive alternatives to conventional surgical treatment of extra cranial carotid artery aneurysms. The combined stroke and mortality rate of surgical reconstruction reported by the Texas Heart Institute was 9% [8] . They described a partial aneurysmectomy and patch closure of a large fusiform aneurysm involving the carotid bifurcation. This approach avoids extensive dissection of the posterior wall of the aneurysm, reducing the rate of cranial nerve dysfunction to 6%. McCann et al. [9] showed a stroke risk of 25% and a mortality rate of 20% in the follow-up of ICA ligation. A meta-analysis by Roset et al. [10] revealed a 1.2% mortality risk and a 6% stroke risk.
Long-term results for carotid aneurysm repair using stent grafts have not been established. Zhou et al. [8] reported a decrease in the 30-day stroke/death rate from 14% to 5% during a 19-year period with the introduction of endovascular techniques. Endovascular interventions reduce the risk of cranial nerve injury, can be done without general anaesthesia, are useful for distal lesions where surgical exposure is difficult, are associated with shorter hospital lengths of stay, and have lower morbidity and mortality rates.
4. Conclusion
Extracranial ICA aneurysm though is rare. We present the patient presented as a submandibular swelling with signs of inflammation. Luckily it was not incised by the local medical center as they suspected it to be an aneurysm, though it was not pulsatile. In fact on presentation, it was a tense painful swelling. Luckily we could come up with the diagnosis with Doppler and confirmed the anatomy by CT angiogram and proceed with surgery. Though resection and interposition graft were recommended, we could use the native ICA and reform the artery without any artificial graft.