Intradialytic Hypertension: Prevalence and Associated Factors in Chronic Hemodialysis Patients in Senegal ()
1. Introduction
Usually, in most chronic hemodialysis patients, blood pressure (BP) decreases during the hemodialysis session due to ultrafiltration. However, in some patients, it increases and remains high during and after the dialysis session, hence the term paradoxical hypertension (HTN) [1] . Intradialytic hypertension (IDH), although discovered many years ago, is often neglected. Its definition remains imprecise and depends on the subjectivity of the authors working with it. It is most commonly defined as the elevation of BP greater than 10 mmHg in the post-dialysis period compared to the pre-dialysis one [1] . Several pathophysiological mechanisms have been proposed to explain the genesis of IDH. Among these mechanisms, hypervolemia certainly plays a central role [2] [3] [4] . Arterial stiffness [2] , the renin angiotensin aldosterone system [5] , and the elimination of antihypertensive drugs through dialysis [5] are other possible pathophysiological mechanisms associated with IDH. Finally, the electrolyte imbalance [6] [7] , sympathetic activity [5] , use of erythropoietin stimulating agents (ESA) [8] , and endothelial cell dysfunction [2] may play a role as well. IDH is commonly observed in hemodialysis patients. Recent work has focused on its clinical implications, with epidemiological evidence suggesting an association with increased morbidity and mortality [7] . Its frequency varies as per the definition used. Some data are available in the context of Africa.
To the best of our knowledge, no work has been performed evaluating IDH in a population of chronic hemodialysis in Senegal.
It is with this premise that the study was carried out, aiming to assess the prevalence of IDH in a population of chronic hemodialysis patients and to seek factors associated with it.
2. Patients and Methods
2.1. Design of Study
It was a cross-sectional and multicenter study of the descriptive and analytical type, which was conducted over a period of 3 weeks (from April 24, 2017 to May 12, 2017) in the hemodialysis units of Aristide Le Dantec Hospital in Dakar and Ziguinchor Regional Hospital Center. Patients with chronic hemodialysis carried out on a regular basis (2 or 3 sessions per week), at least 18 years old, and those agreeing to participate in the study were included. Patients who did not have 4 measurements (measured before and after 4 hemodialysis sessions) or decided to withdraw from the study were excluded.
2.2. Data Collection
Data was collected utilizing a systolic BP (SBP) and diastolic BP (DBP) record card, pre- and post-dialysis for 6 hemodialysis sessions as well as an epidemiological, anthropometric, clinical data collection card, para clinical and therapeutic from patient records. These data were considered as potential associated factors with IDH.
2.3. BP Measurement
The BP of patients before the hemodialysis session were measured in the supine position after five minutes of rest, right before connecting the patient, and those of the end-of-session BP was measured after the extracorporeal blood circuit was restored. The measurements were carried out by dialysis technicians or nurses, using an electronic BP machine of the OMRON® and SPENGLER®type. The heart rates (HR) and weights before and after the session were also recorded. We calculated the difference between pre-dialysis and post-dialysis SBP, mean pre- and post-dialysis Pulse Pressure (PP), mean pre- and post-dialysis HR, and IDWG.
2.4. Parameters Setting
IDH was restrained by an increase in SBP right after the hemodialysis session by 10 mmHg compared to that recorded before session [1] , with a repetition of this phenomenon for at least 4 hemodialysis sessions [9] .
2.5. Statistical Analyses
Data was captured utilizing the Sphinx software, version 5.1.0.2, and analyzed using SPSS (Statistical Package for Social Science), version 18. A descriptive study was performed with the calculation of frequencies and proportions for qualitative variables and calculation of the means and standard deviation for quantitative variables. An analytical study was done with crossed tables. To compare the frequencies, we applied Pearson’s chi-square test or Fisher’s exact two-sided test according to their applicability conditions. The comparison of averages was facilitated by the Student’s t-test. The threshold of significance was retained for p ≤ 0.05.
3. Results
During the study period, 112 out of the 114 chronic hemodialysis patients met the inclusion criteria, and 19 patients were later excluded. Thus, 93 patients were retained in the study, which represents 81.6% of the sample. The design of study is illustrated in Graphic 1.
The mean-age of patients was 48.72 ± 14.06 years and a sex ratio (M/F) of 1.21. The mean duration of dialysis was 64.22 ± 45.63 months. Hypertensive nephropathy was more common, noted in 36 patients, which equals 38.7%, and nephropathy was indeterminate in 19 patients, which is 20.4%. The mean inter dialytic weight gain (IDWG) was 2.04 ± 1.06 kg, and the mean dry weight was 62.71 ± 13.69 kg. The mean hemoglobin level was 9.27 ± 1.91 g/dl, and the mean albumin level was 35.4 g/l ± 7.48. Hypoalbuminemia and anemia were noted in 50% and 68.7% of patients respectively. Out of the 93 patients, 19 (20%) were on ESA, 59 (63.4%) were on antihypertensive treatment. The characteristics of patients are presented in Table 1 and antihypertensive drug type used is given in Table 2.
The mean pre-dialysis BP was 144.48 ± 17.89/84.92 ± 13.99 mmHg, and the post-dialysis one was 146.38 ± 24.09/87.55 ± 15.17 mmHg. The mean pre-dialysis HR was 75.86 ± 10.9 pulsation per minute (ppm), and the post-dialysis HR was 77.06 ± 12.37 ppm. The mean pre-dialysis PP was 59.6 ± 16.20 mmHg, and that of the post-dialysis was 58.83 ± 17.89 mmHg.
During the study period, the SBP of 539 hemodialysis sessions were recorded at an average of 5.8 ± 0.5 sessions per patient. Among these 539 sessions, an increase of more than 10 mmHg of post-dialysis BP compared to that of pre-dialysis was observed in 179 sessions, which corresponds to 33.2 per 100 hemodialysis sessions. IDH was noted in 21 patients representing 22.6%. Factors that could influence the increase in SBP during the hemodialysis session were as follows: high post-dialysis PP, pre-dialysis systolic-diastolic HTN, pure pre-dialysis systolic HTN, and hypoalbuminemia. Associated factors with IDH are shown in Table 3.
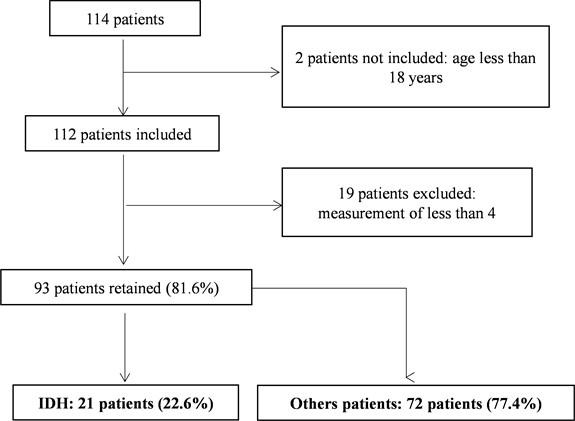
Graphic 1. Design of study.
![]()
Table 1. Characteristics of patients.
ECG: electrocardiogram; TTE: Transthoracic Echocardiography; LVH: Left Ventricular Hypertrophy.
![]()
Table 2. Types of antihypertensive drugs used.
ICE: Inhibitors of the Conversion Enzyme; AAR: Antagonist of Angiotensin II Receptors; ICC: Inhibitors of Calcium Channels.
![]()
Table 3. Associated factors of IDH.
4. Discussion
During the study period, 539 hemodialysis sessions were recorded. This result is lower than those of Sinomono [10] in Morocco and Attilio [11] in Italy, which respectively reported 828 and 51,504 hemodialysis sessions. This difference can be justified by the availability issues pertaining to the electronic BP machine in our services. We recorded an increase in post-dialysis SBP compared to pre-dialysis SBP in 179 hemodialysis sessions, which is 33.2 per 100 hemodialysis sessions. This prevalence was significantly higher than that reported by Van Buren in 2012, which was 21.3 per 100 hemodialysis sessions [12] .
IDH is generally perceived as a rare phenomenon in hemodialysis [13] [14] . In several studies applying the same criteria, its prevalence was less than 15% [15] . In our study, we have reported a relatively significant prevalence of IDH at 22.6%. This prevalence was comparable to that reported by Attilio [11] in Italy, which was 23.1%. However, it was lower than that of Sinomono [10] in Morocco, Sebastian [16] in South Africa and Mackanga [17] in Gabon, which reported prevalence rates of 29.17%, 28.4%, and 28.99% respectively. It was higher than that of the CLIMB study [18] as well asthe WAVE 2 study [19] , which reported respective prevalence rates of 13.2% and 12%. The noted prevalence of IDH in our study was alarming, as it is currently considered a risk factor for cardiovascular mortality [11] . Inrig et al. [20] noted an increased risk of hospitalization and death at 6 months in patients who had an increase in BP by 10 mmHg during the hemodialysis session as compared to the patients whose BP decreased during the hemodialysis session. Post-dialysis SBP was also more significantly correlated with the ambulatory inter dialytic BP than pre-dialysis [21] . Its management is necessary and can be facilitated through the adequate management of the blood volume with the estimate of an ideal weight, individualization of hemodialysis parameters, and use of modules for retro control of ultrafiltration. It is also necessary to identify such associated factors to support them optimally.
In our study, factors that could influence the increase in SBP during the hemodialysis session were as follows: high post-dialysis PP, pre-dialysis systolic-diastolic HTN, pure pre-dialysis systolic hypertension, and hypoalbuminemia (p = 0.049).
High PP was a predictor of IDH (70.25 ± 15.99 vs 55.49 ± 17.11), with a p-value at 0.0008. This association is alarming. Several studies have shown that PP is a cardiovascular risk factor that is independent of the average arterial pressure. This risk factor primarily plays a role in the prediction of a myocardial infarction and, to a lesser degree, in the prediction of cerebrovascular accidents, where the average arterial pressure plays a greater role than pulse pressure [22] . In the Attilio study, IDH was associated with PP pre-dialysis rather than post-dialysis [11] .
Pre-dialysis systolic-diastolic HTN was also an associated factor for IDH (p = 0.004), whereas patients with pure systolic HTN pre-dialysis performed less better IDH (protective factor) (p = 0.01). In the Sinomono study [10] , HTN at beginning of session was considered a risk factor (p < 0.001).
In our study, patients in the IDH group were older (IDH vs control, 49.14 ± 13.21 vs 48.6 ± 14.39) and presented lower mean IDWG (1.86 ± 1.22 vs 2.09 ± 1.01), lower average dry weight (59.19 ± 11.26 vs 63.73 ± 14.23 kg) as well as a lower BMI (20 ± 3.73 vs 21.72 ± 4.34) than those in the control group, without recording a statistically significant difference.
We noted regression in the prevalence of IDH with dialysis duration and no statistically significant difference (p = 0.32): from 1 to 59 months = 54.8%; 60 to 199 months = 32.3%; 120 to 179 months = 9.7%; and 180 months and over = 3.2%; moreover, it was noted with the increase in IDWG: less than 2 kg = 32.1% (9); from 2 to 3 kg = 20% (9); and 3 kg and more = 15% (3).
5. Conclusion
IDH remains a frequent phenomenon in chronic hemodialysis patients and is often neglected. In our study, it was observed in 21 patients, which represents 22.6% of our sample. It is associated with mortality and increased morbidity, especially in terms of cardiovascular issues. High post-dialysis PP, pre-dialysis systolic-diastolic HTN, pure pre-dialysis systolic hypertension, and hypoalbuminemia were significantly associated with IDH. This must be sought and supported primarily through the adequate management of the volume and secondarily through the mastery of vasoconstriction by the individualization of dialysis and antihypertensive drugs.
Limitation of the Study
It is a cross-sectional study with para clinical data collected retrospectively. Analytically, the small number of patients does not make it possible to affirm the associations found. Other multicenter and prospective studies are needed to confirm these associations.
Conflicts of Interest
The authors declare not to have any conflict of interest in relation to this article.