Misdiagnosis of Angina Pectoris Due to Severe Coronary Artery Disease: An Anecdotal Case ()
1. Introduction
Angina pectoris is the result of myocardial ischemia caused by an imbalance between myocardial blood supply and oxygen demand [1] .
Angina is a common complaint presenting typical symptoms (e.g., chest pain) among patients, including athletes, with coronary artery disease [2] .
A comprehensive approach to diagnosis and to medical management of angina pectoris is an integral part of the daily responsibilities of any health care professional, particularly cardiologists, general practitioners, and specialists in sports medicine [3] [4] .
The following should be taken into account during the physical examination:
• For most patients with stable angina, physical examination findings are normal.
• A positive Levine sign suggests angina pectoris.
• Signs of abnormal lipid metabolism or of diffuse atherosclerosis may be noted.
• Examination of patients during an angina attack may be more useful.
• Pain produced by chest wall pressure usually has a chest wall origin.
• Exercise ECG testing is mandatory in patients with chest pain during effort.
Exercise stress testing alone generally has somewhat lower sensitivity and specificity, however, it is cheaper and therefore a reasonable choice for patients with a low probability of disease [5] .
Exercise stress testing is definitely the better choice in detecting angina pectoris in patients with stable coronary artery disease [6] .
Physicians should strictly adhere to the American Heart Association’s recommendations in testing both symptomatic and asymptomatic athletes [7] .
2. Case Report
A 50-year-old male, master cycling athlete with a family history of cardiovascular disease and no other risk factors such as smoking, hypercholesterolemia, hypertension, et cetera, complained of retrosternal chest pain during physical exertion whilst pedalling uphill that forced him to slow down and interrupt exercising. The athlete described the pain during effort as a fist blow in his chest on the retrosternal side (typical Levine’s sign). Although the family physician consulted initially by the athlete reassured him that the most likely cause was a flu-like syndrome the athlete’s wife however decided to get a second opinion, from a consulting a cardiologist in a hospital center, who carried out a detailed clinical examination. In the athlete, with unremarkable physical examination, electrocardiogram (ECG) (see Figure 1) and echocardiography investigations were negative for diseases, therefore the cardiologist concluded for atypical chest pain in the absence of heart disease. Consequently “further tests were not required”.
This was the conclusion of the cardiologist. Fortunately, the athlete underwent a checkup a week later at our center of sports cardiology as part of his pre-participation screening. The pre-test probability for coronary artery disease based on age, sex and symptoms was high. Resting ECG was normal, while exercise ECG testing was interrupted for muscle weakness and showed abnormal ventricular repolarization (after only 5’ minutes work at 150 Watt) with marked ST-segment depression on leads V4 - V6 (see Figure 2) in coincidence to chest pain, typical for angina pectoris.
Recovery ECG confirmed the presence of subendocardial ischaemia due to the presence of ST-segment depression on leads V4 - V6 (see Figure 3).
Based on the results of that test, the athlete was sent for catheterization and the subsequent coronary angiogram showed (see Figure 4) a significant narrowing with 90% occlusion of the proximal left anterior descending artery (TIMI 1 flow) that required angioplasty with drug eluting stent (DES) placement. The athlete returned to his normal physical activity (cycling) routine within 3 months.
3. Conclusions
Investigating chest pain and its cause may delay or make an incorrect diagnosis because in some cases, chest pain may be vague and/or not severe enough for a person to seek medical care.
Chest pain, however, can be a sign of a serious condition and should be evaluated immediately. Chest pain is a symptom of many different conditions, so a thorough medical evaluation is needed to ensure an accurate diagnosis of the reason for chest pain [8] .
Misdiagnosis of angina pectoris is uncommon, but it does happen most frequently among general practitioners rather than among cardiologists [9] .
Misdiagnosis needs an unfeared outcome. There are various ways of preventing misdiagnosis such as seeking a second opinion or referring to a specialist.

Figure 1. Shows normal resting ECG tracing.

Figure 2. Shows abnormal exercise ECG testing with ST-segment depression on anterior precordial leads.

Figure 3. Shows persistent ST-segment depression on precordial anterior leads in ECG recovery tracing.
For this reason, an athlete who has symptoms, doubts and ambiguities regarding angina pectoris, must be reviewed and evaluated by a competent physician in sports cardiology, who is familiar with and has experience in exercise testing and ECG monitoring [10] .
For the athlete with symptoms, the nature of the symptoms outweighs any considerations of age or cardiac risk factors in the decision to perform exercise testing.
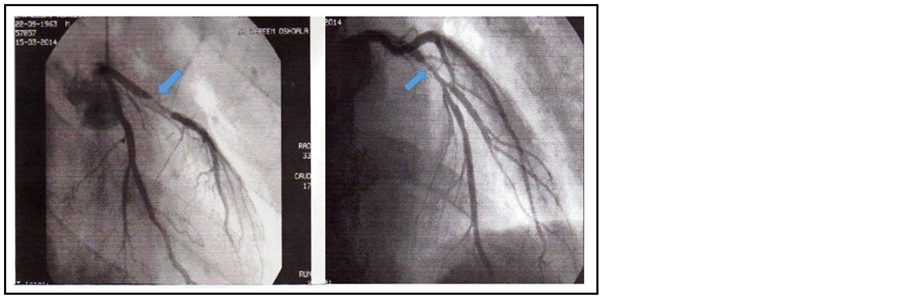
Figure 4. Shows critical stenosis of the proximal Left Anterior Descending artery on coronary angiogram (see blue arrows).
An athlete is considered symptomatic if he has any positive findings based on the AHA recommendations on history and physical examination [7] .
Symptomatic athletes older than 35 years are at a higher risk for CAD, which accounts for over 75% of the sudden deaths in this age group [11] .
For symptomatic athletes over 35, exercise testing (ET) has good sensitivity (70%) and specificity (80% - 90%) and should be used when appropriate in the case of any older athlete with eventual ischemia [6] .
In spite of this, diagnosis often eludes those doctors lacking the ability to recognize the disease, especially when it concerns athletes, i.e. subjects considered, a priori, healthy and thus hardly prone to this condition.
Fortunately, sports medicine and doctors skilled in uncovering cases of ischemic heart disease in athletes are increasingly able and trained to recognize ambiguous or doubtful cases during pre-competition screening, such as the subject in this case report.
Indeed, such an athlete suffering from a typical Second-wind Phenomenon, i.e., when the patient repeats the same activity after attack, may not feel the attack again the second time.
In fact, the symptom, also known as Walk-through Angina, is when the pain subsides as the patient continues his physical activity.
The purpose of this case report is therefore to induce physicians to pay more attention to the symptoms of angina and in case of doubt, perform a stress test that represents the best way in making a definitive diagnosis, or at least, in providing additional clinical elements for the patient’s safety.
In conclusion, the author considers the exercise ECG stress testing a key tool in risk stratification as it is vital in deciding on clinical management procedure.
NOTES
*Corresponding author.