Factors influencing self-efficacy in breastfeeding support among public health nurses in Japan ()
1. INTRODUCTION
1.1. Breastfeeding Trend
Breastfeeding has short term and long-term health benefits for both mothers and children [1-3] and is promoted in many countries. The WHO and UNICEF published the “Global Strategy for Infant and Young Child Feeding”, which recommended breastfeeding exclusively for the first 6 months after birth [4].
Despite the clear benefits of breastfeeding to mother and infant, breastfeeding rates remain low level in Japan. According to the Young Child Physical Development Survey conducted by Japan’s Ministry of Health, Labour and Welfare every 10 years since 1960, the breastfeeding rate of 1 - 2-month-old babies was 70.5% in 1960 but dropped to 31.7% in 1970 and has remained low since then [5].
Therefore, increasing the breastfeeding rate of 1- month-old babies was a goal in Healthy Family 21, the national campaign for maternal and child health (MCH) in Japan. And to share basic concepts with health workers and to support mothers who want to breastfeed, the Ministry of Health, Labour and Welfare published and promoted the Guide for Feeding and Weaning Infants and Young Children in 2007 [6].
Review of previous studies showed that professional supports had a positive influence on breastfeeding [7]. The Japan public health nurses (PHNs), who have been providing home visits and telephone counseling to support mothers and families, play an important role in supporting mothers on breastfeeding. To encourage breastfeeding, PHNs have launched initiatives such as group education for mothers, individual counseling, and peer support groups, and they coordinate meetings with pediatricians, obstetricians, and midwives. However, they may not be providing enough support to mothers.
1.2. Factors Associated with Self-Efficacy in Breastfeeding Support among PHNs
Bandura [8] suggested that human behavior is influenced by self-efficacy. Then previous studies used selfefficacy of breastfeeding support as an outcome indicator instead of measuring behaviors [9-11]. That is why we focused on self-efficacy and associated factors in this study. Previous studies have found that the following factors are possibly associated with the self-efficacy of breastfeeding support among PHNs.
1) Working area Previous research has suggested that working area influenced the self-efficacy of breastfeeding support among PHNs. Comparisons of municipality size and the practical abilities of PHNs showed that community assessments and competencies in personal support, policymaking, and data analysis of PHNs working for populations under 50,000 were lower than those of PHNs working for populations over 50,000 [12].
The Japanese Nursing Association (JNA) reported statistics on postgraduate education among PHNs by district in Japan in 2010 [13]. Kanto had the highest number of PHNs who attended trainings (50.5%) while Shikoku (36.5%) and Kyushu/Okinawa (37.6%) had the lowest. In addition, Kanto also had the highest number of PHNs who were supervised by preceptors (49.7%) while Shikoku (30.8%) and Kyushu/Okinawa (27.0%) had the lowest.
These results imply that self-efficacy in breastfeeding support among PHNs might be lower in small municipalities and in Shikoku and Kyushu/Okinawa. However, the reasons for these differences remain unknown.
2) Personal factors Personal factors such as education background, working experience and breastfeeding experience could influence the self-efficacy of breastfeeding support among PHNs. A change in the education trends of PHNs (from being trained in vocational schools to being trained in less specialized universities) might have resulted in current PHNs having lower practical abilities. In the last 20 years, PHN education has changed in Japan. PHN education has traditionally been provided by vocational schools for 1 year after graduating from 3 years of general nursing education. However, due to the increase in the number of universities from 1991 to 2007, many PHNs have university education. It has also been suggested that PHN education in universities consists of less lectures and practicums [14].
In addition, previous studies have found that nurses in the US who had more than 5 years of working experience had higher self-efficacy than nurses who had less than 5 years’ experience [15]. Furthermore, doctors in Australia [10] and the US [11] who had longer personal breastfeeding experience had higher self-efficacy.
It would thus be interesting to investigate whether PHNs in Japan with more working experience, breastfeeding experience, and who graduated from vocational schools would have higher self-efficacy in providing breastfeeding support.
3) Postgraduate and continuous education Kronborg [9] reported that nurses who attended prestudy training courses increased their self-efficacy about helping mothers with common breastfeeding problems. Another study showed that nurses had increased selfefficacy on breastfeeding support after attending training programs [16], implying that continuous education could improve the self-efficacies of PHNs on breastfeeding support.
The purpose of the present study was thus to determine the level of self-efficacy in providing breastfeeding support in PHNs working for MCH services in Japanese municipalities and its related factors, such as population, working area, education background, working experience, personal breastfeeding experience, postgraduate education, and continuous education.
Hypotheses 1) Self-efficacy in breastfeeding support would be higher among PHNs working in Kanto or in large/urban municipalities.
2) Self-efficacy in breastfeeding support would be higher among PHNs who had received 1 year of vocational training or who had more working and breastfeeding experience.
3) Self-efficacy in breastfeeding support would be higher among PHNs who have postgraduate education and who engage in continuous education.
2. METHOD
2.1. Participants
Participants were PHNs working at MCH services in Japanese municipalities. To control for potential confounders, only PHNs without midwife qualifications and those who had 5 to 15 years of working experience were included in the sample. If there was no PHN who met these conditions in a municipality, then PHNs with comparable working experience were recruited.
2.2. Data Collection
An anonymous self-report questionnaire, a letter explaining the study, instructions, and a return envelope were sent to directors of MCH divisions in all Japanese municipalities, who were requested to select one PHN to answer. The PHNs then returned the completed questionnaires to the researchers.
The data were collected from the end of October 2010 to the beginning of January 2011.
2.3. Ethical Approval
Ethical approval was obtained from the ethical review committee of the Faculty of Medicine, The University of Tokyo (Clearance No. 3035).
2.4. Questionnaire
The questionnaire was designed to collect data on working area, sociodemographic characteristics, postgraduate education/continuous education, and self-efficacy in breastfeeding support.
1) Independent variables a) Working area: municipalities were categorized into small (population < 20,000), middle-sized (population: between 20,000 and 100,000), and large/urban (population: > 100,000 or a city with a public health center). Prefectures were categorized into 8 districts (Hokkaido, Tohoku, Kanto, Chubu, Kinki, Chugoku, Shikoku, and Kyushu/Okinawa).
b) Sociodemographic characteristics: these included sex, age, working experience, educational background to be a PHN, breastfeeding experience (personal or helping their partners), and number of PHNs working for the MCH service in their municipality.
c) Postgraduate/continuous education: the question “have you ever attended trainings or seminars on breastfeeding support after graduation?” asked about postgraduate education while “have you read the Guide for Feeding and Weaning Infants and Young Children?” assessed continuous education. A 5-point Likert scale was used for the responses, ranging from 1 (not at all) to 5 (all of them).
2) Dependent variable a) Self-efficacy of breastfeeding support: the SelfEfficacy of Breastfeeding Support Scale (SBSS) was developed in a previous study [17] for nurses and midwives working in hospitals. We modified the SBSS in this study for PHNs working in municipalities (SBSS-R). The content validity of the SBSS-R was established through discussion with 2 other researchers, 1 of whom worked for family health nursing and the other had more than 10 years’ experience as a municipal PHN. Questions about support related to hospitalization in the original SBSS were excluded and questions about support in the community were added, resulting in a questionnaire with 14 questions with responses on a 5-point Likert scale, ranging from 1 (not confident) to 5 (very confident).
A pretest was conducted on 22 PHNs; results confirmed that the questionnaire was easy to understand and answer. Exploratory factor analysis (principal factor method, promax rotation) was conducted to confirm construct validity. Three factors were revealed: technical and individual support (Factor 1), infant care support (Factor 2), and emotional and group/community support (Factor 3; see Table 1). Factor contribution was 5.56 for Factor 1, 0.99 for Factor 2, and 0.75 for Factor 3, with the cumulative contribution ratio being 52.1%.
Hirano [18] reported that PHNs have 3 roles: individual care such as technical consultation and education, group support and networking, and system development such as quality assurance and providing new support. Factors 1 and 2 in this study measured individual and family support, with Factor 1 measuring support for mothers and families and Factor 2 measuring support for baby care while Factor 3 measured support for the group and providing new support. The ability of the SBSS-R to measure the 3 roles of PHNs indicates that it is a valid assessment. Although the SBSS-R has subscales, the total SBSS-R score was used for this analysis because this study examined comprehensive self-efficacy of breastfeeding support and its related factors. The Cronbach’s alpha obtained for the SBSS-R was 0.89, indicating high reliability.
2.5. Data Analysis
Frequency distributions were generated for working area and sociodemographic variables. Postgraduate/continuous education and SBSS-R were adjusted with the weights of PHN sampling and collection rates by prefecture and population size. The weights were calculated with the following equations (Figure 1).
Multiple linear regression was used to examine selfefficacy in breastfeeding support and its related factors with the adjusted weights. Model 1 included working area as the independent variable and the SBSS-R as the dependent variable. Sociodemographic variables were added as an independent variable in Model 2 and postgraduate/continuous education in Model 3. Dummy variables were used for district data due to the use of a nominal scale, with Kanto as a reference. To prevent multicollinearity, age and education were not entered into the analysis. Data from two male PHNs were included into the analysis after confirming that there were
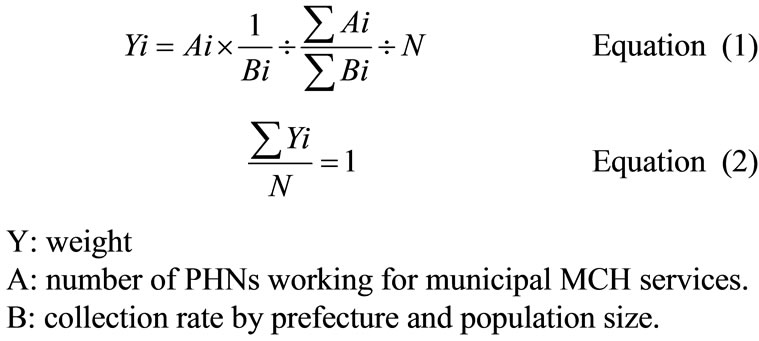
Figure 1. Weights of PHN sampling and collection rates by prefecture and population size.

Table 1. Exploratory factor analysis of the Self-efficacy in Breastfeeding Support Scale (14 questions): N = 729.
Principal factor method, promax rotation.
no effects of gender. The threshold for statistical significance was set at 0.01. SPSS 19.0 for Windows was used for analysis.
3. RESULTS
3.1. Sample
Of the 1750 questionnaires sent, 831 were returned (response rate: 47.5%); 102 were excluded from analysis because of missing data, making the valid response rate 41.7% (729).
Table 2 shows that more than 99% of the sample was female and that the average age was 35.6 years (SD = 6.2; range: 22 - 62). Average working experience was 10.7 years (SD = 5.5; range: 0 - 33). Educational background to be a PHN consisted of vocational school (63.6%), university (32.5%), and others (3.8%). The category “others” was absorbed into “vocational school” in the analysis because this comprised mainly a 1-year training in junior college, which is similar to that in vocational school.
Respondents with personal breastfeeding experience

Table 2. Sociodemographic characteristics of respondents: N = 729.
constituted 64.2% of the sample; this percentage included respondents who had partners who engaged in breastfeeding. The average number of PHNs working in MCH services in the community was 8.1 (SD = 14.1; range: 1 - 250).
3.2. Self-Efficacy of Breastfeeding Support
The average score obtained on the SBSS-R was 3.4 (SD = 0.5; see Table 3). The following statements had higher average scores than other statements: “I can explain the benefits of breastfeeding” (M = 4.0, SD = 0.6); “I can describe the development of a newborn” (M = 4.0, SD = 0.6); “I can explain the physiological functions in newborns” (M = 3.9, SD = 0.7); and “I can introduce mothers to facilities, home visit services, and medical centers that provide breast care” (M = 3.9, SD = 0.7). On the other hand, the statements “I can guide mothers on breast care in order to facilitate lactation” (M = 2.9, SD = 1.0) and “I can promote breastfeeding in the working environment and in public” (M = 2.8, SD = 0.9) had lower average scores than other statements.
3.3. Postgraduate/Continuous Education on Breastfeeding Support
The attendance rates of training programs or seminars on breastfeeding support after graduation was found to be 56.4%, and 87.9% reported to have read the Guide for Feeding and Weaning Infants and Young Children.
3.4. Relationships between SBSS-R and Working Area, Sociodemographic Characteristics, and Postgraduate/Continuous Education
Model 1 showed that SBSS-R scores were significantly higher for large/urban municipalities (β = 0.13, p < 0.01) and Kanto and lower for Chugoku (β = −0.14, p < 0.01), Shikoku (β = −0.11, p < 0.01) and Kyushu/ Okinawa (β = −0.14, p < 0.01) (see Table 4). The adjusted R2 was 0.05.
Model 2 revealed that SBSS was significantly associated with working experience (β = 0.13, p < 0.01) and breastfeeding experience (β = 0.22, p < 0.01), but not with education background. The adjusted R2 was 0.14 and was significantly higher than that of Model 1 (difference = 0.09, p < 0.01).
The results of Model 3 indicated that SBSS was significantly associated with postgraduate education (β = 0.14, p < 0.01) and continuous education (β = 0.12, p < 0.01). The adjusted R2 was 0.17 and significantly higher than that of Model 2 (difference = 0.03, p < 0.01).
4. DISCUSSION
This study showed self-efficacy in breastfeeding support among PHNs and its related factors, such as population, working area, working experience, personal breastfeeding experience, postgraduate education, and continuous education.
4.1. Self-Efficacy in Breastfeeding Support
Each statement on the SBSS-R obtained different rat-
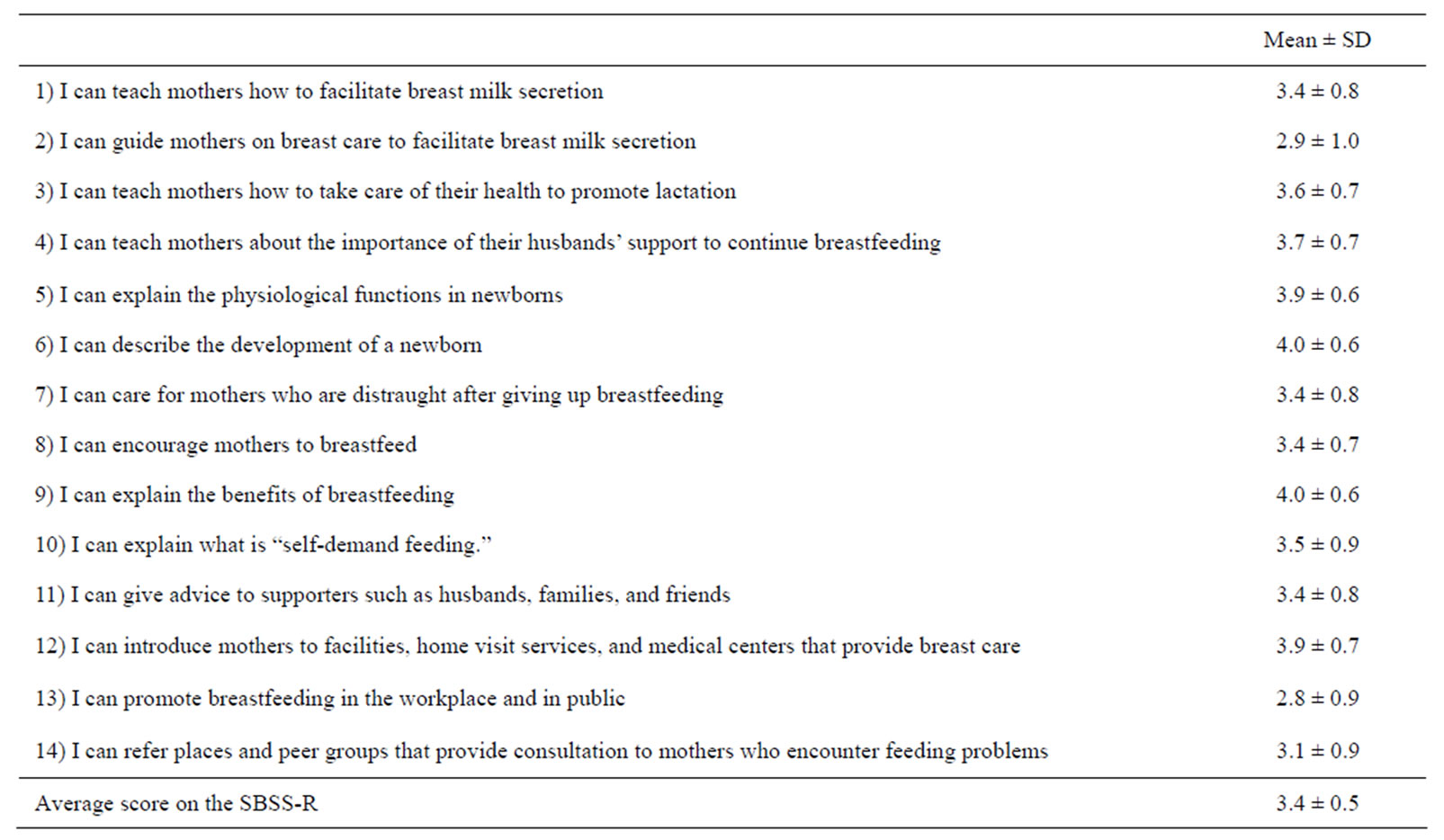
Table 3. Self-efficacy in breastfeeding support among PHNs working for MSC services: N = 729.
Questions were responded to on a 5-point Likert scale ranging from 1 (not confident) to 5 (very confident). Adjusted with weights of PHN sampling rate and collection rate by prefecture and population size.

Table 4. Relationships between SBSS and working area, sociodemographic variables, and postgraduate/continuous education among PHNs working for MCH services; multiple linear regression analysis†, N = 729.
†Adjusted for PHN sampling rate and collection rate by prefecture and size of population. aReference: Kanto district; b1 = small municipality, 2 = middle-sized municipality, 3 = large/urban municipality; c1 = vocational school/junior college, 2 = University; d1 = yes, 0 = no; e5-point Likert scale; 1 = not at all, 2 = some of them, 3 = half of them, 4 = most of them, 5 = all of them.
ings, with confidence in guiding mothers on breast care to promote lactation and in the promotion of breastfeeding-friendly environment receiving lower scores than other statements.
A possible explanation is that PHNs have theoretical knowledge of breastfeeding but not practical knowledge on breast care. Thus, it would be helpful for PHNs to have practical training on breast care. Another area that our sample lacked confidence in is the promotion of a breastfeeding-friendly environment, which requires policy planning, resource mobilization, and intersectional collaboration.
By focusing on areas where PHNs are less confident in for training programs, overall self-efficacy on breastfeeding support could be increased in PHNs.
4.2. Related Factors of Self-Efficacy on Breastfeeding Support among PHNs Working at Municipal MCH Services
Self-efficacy on breastfeeding support was significantly associated with working area, sociodemographic characteristics, and postgraduate/continuous education among PHNs working for MCH services.
1) Self-efficacy of breastfeeding support and working area Self-efficacy of breastfeeding support is higher among PHNs working in large and/or urban municipalities, which supports Hypothesis 1. This is true even after adjusting for related factors, such as breastfeeding experience, working experience, PHN education, and postgraduate/continuous education. Our finding corroborates that of a previous study [12], which found that competence in support, policy-making, data analysis, and community diagnosis is lower among PHNs working for small municipalities. A possible reason for this low competence could be that PHNs working in small municipalities have insufficient training opportunities and limited access to information.
Self-efficacy in breastfeeding support was lower among PHNs working in Chugoku, Shikoku, and Kyushu/Okinawa and higher in Kanto. This result supports that of a previous study [13], which examined training opportunities for PHNs by district, suggesting that selfefficacy in breastfeeding support is influenced by the availability of opportunities for training/education in districts.
2) Personal experiences of PHNs There was no association between the educational backgrounds of PHNs and self-efficacy in breastfeeding support even after adjusting for related factors. Thus, Hypothesis 2 was not supported. Our result might correspond with that of Tsumura [19], who reported that the practical abilities of PHNs who had university education are highly individual. The conflicting results might be due to the difference in breastfeeding education in PHN education; the curriculum also varies according to schools. Therefore, future studies should clarify the relationship between breastfeeding education and self-efficacy in breastfeeding support in PHNs.
However, we found that PHNs with more working and personal breastfeeding experience had higher self-efficacy in breastfeeding support than those who did not, even after adjusting for other related factors. This finding partially supports Hypothesis 2.
3) Postgraduate/continuous education PHNs who received postgraduate training or who engaged in continuous education had higher self-efficacies in breastfeeding support even after adjusting for related factors—a finding that supports Hypothesis 3.
This result suggested that self-efficacy in breastfeeding support in PHNs could be increased through attending trainings and self-enrichment. It is therefore necessary to create training opportunities for PHNs and to provide new and important information to them, especially those who work in remote and/or small municipalities.
5. LIMITATIONS OF THIS STUDY
This study covers all municipalities in Japan; however, the sampling rate differed between municipalities. The response rate was 47.5% and varied by district and population size, which was why we adjusted for these factors. However, the PHNs who responded may have been more interested in breastfeeding support than those who did not answer this questionnaire; respondents were not randomly selected from the municipalities.
The SBSS-R was used because its content validity, construct validity, and reliability have been established. However, its criterion-related validity and stability have not been examined. This instrument is thus expected to be further refined in future studies.
Finally, this study revealed the relationship between self-efficacy in breastfeeding support and its related factors but could not draw a causal conclusion due to its cross-sectional design. Therefore, future studies should use a longitudinal design to determine causal relationships.
6. CONCLUSION
This study identified the areas in breastfeeding support where PHNs lacked self-efficacy, such as breast care and promoting breastfeeding-friendly environments. We also found that self-efficacy in breastfeeding support was higher in PHNs with postgraduate/continuous education, suggesting that this self-efficacy could be increased through self-enrichment. It is thus necessary to increase training opportunities for PHNs and to disseminate new and important information to PHNs, especially those working in remote and/or small municipalities, to increase their self-efficacy in breastfeeding support.
7. ACKNOWLEDGEMENTS
We are grateful to the PHNs who took the time to answer the questionnaire. We would like to express our gratitude to Professor Norito Kawakami for his contribution and thank the faculty and members of the Department of Family Nursing, Graduate School of Medicine/ Faculty of Medicine, School of Health Science & Nursing in the University of Tokyo.