Examining Knowledge Decay in the Anesthesia Provider—An Integrative Review ()
1. Introduction
Knowledge decay, in general, can mean many different things regarding healthcare professionals. It can be referring to the lack of retention of knowledge from an academic institution, or it could be a lapse of knowledge or skills since starting clinical practice. Knowledge decay is a measure of the degradation of knowledge integrity [1] . For example, in an anesthesia provider, this could be a decay in knowledge integrity surrounding anesthetic medications, techniques, or crisis scenarios. Current strategies used to combat knowledge decay in the healthcare setting mostly centers around the requirement of continuing education hours to renew licenses to practice, such as with registered nurses. Although this is a requirement, there is no guidance on the kind of continuing education hours needed to be obtained, such as a simulation activity, online learning modules, or hospital-based training programs. For this reason, continuing education hours are vastly different in scope and knowledge obtained from individual to individual.
It is well-known that knowledge reinforcement can be helpful in retaining skills related to the job. Examining which reinforcement strategies is most influential in knowledge retention would be a beneficial way to find out how to prevent knowledge decay. One knowledge reinforcement theme is the use of a simulation activity. Simulation activities can be high-fidelity or low-fidelity, meaning they can take place in a highly technical simulation lab with scenario-based learning, or they can be a bedside skills test administered by a representative that is knowledgeable of the topic. Blanie et al. [2] constructed a high-fidelity simulation activity with both active participant and observer roles and saw promising results when knowledge decay was assessed later on. Another method in examining knowledge decay was a survey given to both residents and faculty members who had been redeployed to different areas of practice in order to help with the COVID-19 pandemic [3] .
While knowledge decay is well-recognized, there is a significant lack of research on how to prevent it in the anesthesia provider specifically—given that these individuals need to know how to manage a wide variety of clinical situations and crisis scenarios. Knowledge decay affects many healthcare providers globally; however, the following review will aim to examine knowledge decay in anesthesia providers in primarily the United States. One study was examined that took place in another country, as detailed below.
2. Methods
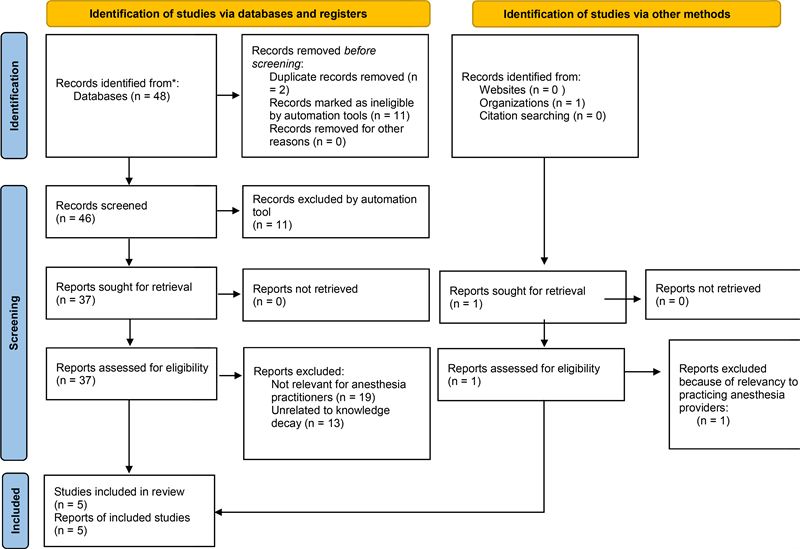
The search strategy was directed by the question, “How does knowledge decay affect the practice of an anesthesia provider?” A comprehensive search of literature was conducted in September 2022, using the databases of PubMed, the Cochrane Library, and Embase. These databases were utilized due to their availability of resources under the topic of knowledge decay regarding anesthesia providers. The detailed search strategy for databases used a combination of Medical Subject Heading (MeSH) keywords and associated terms (found in Table 1 below). MeSH keywords and associated terms were kept vague for several reasons, one being that the literature surrounding this topic is limited. Additionally, different tasks required of the nurse anesthetist sometimes parallel the physician anesthesiologist’s tasks, making knowledge decay a risk for both. Therefore, the search term “anesthesia” was used alongside a more extensive manual review to find relevant
topics. One article found on the American Association of Nurse Anesthesiology (AANA) website was excluded due to irrelevance.
Initially, 48 articles were attained and evaluated. Titles and abstracts were further evaluated for relevancy, applicability, and inclusion criteria. Inclusion criteria consisted of knowledge decay relating to anesthesia providers, preferably a trial or study evaluating the effects of simulation on knowledge decay. Exclusion criteria consisted of non-English language, non-provider studies, publications before 2012, and articles without abstracts or full-text availability. Exclusion criteria of publications before 2012 were implemented to keep all sources within ten years of the search date, while exclusions of articles without abstracts or full-text availability were implemented to ensure studies examined would not be lacking sufficient content to make adequate comparisons. After searching with these criteria, 37 articles were identified. Two were removed due to duplication. Abstract screening was performed by a single reviewer. After evaluating the remaining 35 articles, 30 were excluded after manual review due to lack of relevancy to the topic being researched. A breakdown of exclusions can be found in Appendix 1 below.
Five articles remained after all exclusion criteria had been implemented. These articles were both reviews and trials of knowledge decay for the anesthesia provider.
3. Findings
Five articles published between 2018 and 2022 met the inclusion criteria and were included in the final analysis. The articles were categorized according to evidence level and quality. The Johns Hopkins Nursing Evidence-Based Practice Evidence Rating Scale was used to evaluate the level and quality of the evidence as specified in Table 2 [4] . Four studies took place in the United States, while one took place in France. The sample size varied from 10 - 281 participants. Simulation activities for each study took place in a single simulation center. One article was an online survey and examined knowledge decay over time due to the COVID-19 pandemic. Two articles were level I evidence, two were level II, and
one was level IV. All four articles were quality B evidence. Main themes have emerged that suggest simulation activities, whether used alone or coupled with didactic learning, improve immediate learning outcomes as well as long-term retention of knowledge on the situations being simulated. Another theme emerged suggesting that knowledge decay is abundantly present when examining providers who moved to different specialty areas to help with the COVID-19 pandemic [3] .
Improved Learning Outcomes
Four studies reported increased learning outcomes when using simulation-based learning activities [3] [5] [6] [7] . Blanie et al. [2] measured learning outcomes by using a multiple-choice questionnaire. Kumar et al. [6] implemented an assessment tool to measure learning outcomes. Gisriel et al. [5] used a test that was administered immediately after the simulation activity and one month after the simulation activity had been completed. Miller et al. [7] reported that the use of simulation-based learning activities would help with immediate learning outcomes of anesthesia residents in crisis situations. While the definition of “learning outcomes” may vary between these studies, it is generally assumed that this refers to higher academic performance that can therefore lead to knowledge retention. The most promising learning activity, as examined by the various learning tools, would be simulation-based learning activities.
Augmented Long-Term Knowledge Retention
Three of the studies involving simulation-based learning examined whether the participants had retained knowledge from the learning activities [6] [5] . Kumar et al. [6] focused on how repeated simulation activities would help anesthesia residents more fully retain the knowledge from the activities for long-term use. Gisriel et al. [5] conducted a follow-up assessment one month after the initial simulation activity to see if knowledge decay was present. Gisriel et al. [5] found that students who had completed the simulation-based learning activity had better knowledge retention when compared to those who had learned in the traditional didactic setting by examining the test scores one month after learning had ended. Miller et al. [7] reported that long-term knowledge retention was seen as much as a decade after simulation activities involving anesthesia residents.
Knowledge Decay in Unfamiliar Environments
One study examined the perceived knowledge decay of residents and faculty members who had been redeployed due to the COVID-19 pandemic [3] . Nofi et al. [3] found that the redeployment of residents and faculty members due to the COVID-19 pandemic often led to unfamiliar environments as well as unfamiliar crisis situations. This was examined through an online, multiple-choice survey [3] . The data showed that knowledge decay was present in these redeployment situations, especially in individuals who were in their residency and were redeployed to a different specialty than one they were accustomed to [3] .
4. Discussion
This integrated review examined knowledge decay in the anesthesia provider by looking at a variety of studies with the key findings being the retention of knowledge when simulation activities were implemented. Notably, several studies involved more of how to prevent knowledge decay from happening in the first place by involving healthcare providers with simulation-based learning activities [2] [5] [6] [7] . There was also one study that examined knowledge decay involving the COVID-19 pandemic and how it may have put healthcare providers in unfamiliar or completely new situations [3] . The literature described in this review also represents the limited available evidence on knowledge decay specifically the anesthesia provider.
This review gives insight into which learning activities may be best for combating knowledge decay in general. Several studies showed strong, long-term retention of knowledge with simulation activities specifically [2] [5] [6] [7] . It is important to note that not all learning activities are equal in terms of outcomes, test results, or participant engagement. For instance, didactic learning activities involved in the classroom setting will have different outcomes than activities involved in hands-on learning. This review provides evidence-based practice guidelines for the prevention of knowledge decay in the anesthesia provider.
Evidence-Based Practice Recommendations/Synthesis
Several recommendations are identified for how to combat knowledge decay in the anesthesia provider. Anesthesia providers, particularly those early in training, should be involved in simulation-based learning scenarios that enable them to experience less likely events related to the care of patients undergoing anesthesia [2] [5] [6] [7] . Moreover, anesthesia providers should work in situations and surgeries that they are familiar with, if possible [3] . Knowledge decay is seen mostly in an unfamiliar environment and when simulation-based scenarios have not been utilized along with didactic learning [2] [5] [6] [7] . Anesthesia providers must be adequately and continuously educated on unfamiliar situations they may encounter in the operating room, such as malignant hyperthermia.
Gaps in Literature
Although knowledge decay literature for healthcare providers, in general, has an abundance of literature, knowledge decay in the anesthesia provider specifically does not have as much in-depth examination. One could argue that knowledge decay in the healthcare provider is directly correlated with knowledge decay in the anesthesia provider. However, a specific focus was put on the anesthesia provider due to the unique nature of these individuals in the operating room. Research that would examine more closely the causes and effects of knowledge decay in the anesthesia provider would deliver evidence-based practice on how to combat knowledge decay in the first place.
5. Limitations
This review had several limitations. Notably, there were only five articles obtained that were of relevance to this topic after reviewing several databases. This was due to the search for knowledge decay in the anesthesia provider and not all healthcare professionals. This methodology in obtaining relevant articles severely limited the number of relevant studies. Several of the studies were measured using self-evaluation tools, which is open to bias. One article was also open to recall bias since the survey was sent well after the events had occurred [3] . There was also a small sample size in one study [5] . Additionally, several studies administered the same test to the same students, the only difference being the time from the first administration to the second. This method was open to bias.
6. Conclusion
The aim of this integrative review was to examine research involving knowledge decay in the anesthesia provider and provide evidence-based strategies for how to combat this decay. The findings of this review indicate that knowledge decay occurs when anesthesia providers are in unfamiliar situations, and simulation-based learning activities help combat knowledge decay over time. Future research is needed to expand on these conclusions, such as examining different learning activities or studying knowledge decay over an extended period of time. Healthcare workers can examine these recommendations in order to promote learning and prevent knowledge decay.
Appendix 1. PRISMA flow diagram