Description of the Factors Associated with Trigger Finger in Patients Treated at Petroleos Mexicanos “Pemex” ()
1. Introduction
The trigger finger (TF), also known as stenosing tenosynovitis of the flexor tendon, is a common cause of hand disability. The prevalence of this pathology ranges from 1% to 3%, with an incidence of 2% to 3%. It has two peaks of presentation throughout life: the first is in patients younger than eight years of age, and the second is between the fifth and sixth decades of life [1] . The presence of TF can result in significant limitations in certain daily living activities, such as the holding of objects, counting coins, or buttoning of buttons [2] .
TF has a female predilection and is two to six times more common in women than in men. It occurs most frequently in the middle and ring fingers of the dominant hand, followed by the index and little fingers in that order [1] [3] .
Although the etiology is unknown, some theories have been described, and some predisposing factors are known [3] . Risk factors for this entity include genetic predisposition, systemic diseases (diabetes mellitus, systemic arterial hypertension, and dyslipidemia), and repetitive gripping activities causing mechanical irritation of the first pulley tendon (A1). Several hand diseases, such as Quervain’s tenosynovitis, Dupuytren’s contracture, and carpal tunnel syndrome, have a higher incidence of TF [3] . However, systemic diseases such as hypothyroidism, rheumatoid arthritis, mucopolysaccharidosis, carpal tunnel syndrome, and diabetes mellitus are associated with a higher incidence and severity of TF. The prevalence of TF in patients with type 2 diabetes mellitus ranges from 5 to 20%, and the incidence of TF is 10%. Glycosylated hemoglobin levels greater than 7 have been positively correlated with the development and severity of TF [1] .
The clinical manifestations of TF are varied, ranging from moderate pain to contractures of the fingers involved, as a result of the narrowing and widening of the tendon sheath [3] . A diagnosis is established through a thorough examination of the patient’s medical history and physical examination. The patient may experience pain at the metacarpophalangeal level, functional limitation, flexion locking, locking sensation, or entrapment with active range of motion of the finger (Figure 1 and Figure 2).
It is possible to treat this condition with conservative or surgical methods. The initial treatment regimen consists of local administration of corticosteroids, oral administration of non-steroidal anti-inflammatory drugs, and immobilization of the affected phalanges. Diabetic patients are required to maintain glucose levels within normal ranges [4] . One study compared splinting of the metacarpophalangeal joint with splinting of the proximal interphalangeal joint. Both were effective in reducing pain and disability and improving symptoms. However, splinting the proximal interphalangeal joint was more effective, suggesting that
![]()
Figure 1. Finger with flexion locking due to flexor tendon swelling.
![]()
Figure 2. Nodule in flexor tendon showing locking with A1 pulley. “Created with BioRender.com”.
immobilization of the affected finger is a viable treatment [2] [5] .
Howard first described corticosteroid injection into the flexor tendon sheath in 1953, with variable success rates in subsequent literature. The majority of authors agree that acceptable success rates can be achieved with a minimum of three injections. Seigerman et al. reported that pain relief occurs three weeks after the injection [6] .
Surgery is indicated when conservative treatment is unsuccessful. The open surgical approach employs direct visualization and division or release of the A1 pulley, with success rate exceeding 95%. The most common complications include are persistent pain, swelling, and persistent or recurrent triggering [3] (Figure 3). The percutaneous surgical technique (Figure 4), described in 1958
![]()
Figure 3. Image A with an open surgical approach to release the A1 pulley by making an incision approximately 2 cm above the A1 pulley. Image B shows the incision of the A1 pulley to release the flexor tendon. “Created with BioRender.com”.
![]()
Figure 4. Image A showing the A1 pulley and flexor tendon. Image B showing the release of the A1 pulley with needle via percutaneous needle without incision. “Created with BioRender.com”.
by Lorthioir with 94% effectiveness, has the advantages of minimally invasive surgery (less postoperative pain, less trauma, among others) and a lower cost [3] .
The final treatment decision depends on the preference of the patient and the surgeon’s individual assessment of the severity of each case. Even observation may be an option. The spontaneous resolution of TF has been seen within one year, which is probably attributed to remodeling of the pulley and decreased inflammation due to lifestyle changes [3] [7] .
The aim of the present work is to review the prevalence and epidemiological characteristics of patients diagnosed with TF in our hospital.
2. Methodology
This is a retrospective, observational, cross-sectional and descriptive study. The source population consisted of all patients with a diagnosis of trigger finger who had been treated in the department of plastic and reconstructive surgery of our institution between 2020 and 2023. The inclusion criteria were as follows: patients with a diagnosis of trigger finger between 2020 and 2023, who underwent immediate postoperative clinical follow-up, and who had a complete clinical record.
The only exclusion criterion used was not having a complete clinical record. In 2020 and 2023, a total of 239 patients were obtained, through a non-probabilistic convenience sampling, who had been treated for trigger finger in our institution. Two patients were excluded from the study because they did not receive post-surgical follow-up. The study enrolled a total of 237 participants.
The primary objective of this study is to determine the prevalence and characterize the clinical and surgical characteristics of the population affected by trigger finger in our hospital.
For nominal variables, a frequency analysis was performed. Kolmogorov-Smirnov normality tests were applied, and then mean and deviation were used to describe normally distributed numerical variables and median and range to describe non-normally distributed numerical variables.
Statistical analysis and normality tests were obtained with the jamovi program version 2.3.18. The article was written based on the STROBE guidelines for observational reports. A search for articles was carried out in PubMed, Cochrane Library, Google Scholar, and a synthesis of current knowledge.
In accordance with the ethical norms of the Declaration of Helsinki and article 17 of the Regulations of the General Law of Health on Health Research, the participation of patients in this study involves one type of risk: No Risk.
The protocol was approved by ethic and bioethics commit at Pemex. The information collected will be stored in a database and the identity of the research subject will be protected by entering a consecutive number. This database will only have access to the researchers and will remain under password in the computer of the head of the plastic and reconstructive surgery service, with the data obtained this study will be carried out, and it is planned to save this information for future studies, so it will not be discarded and will be completed with future research subjects. It does not require informed consent because it is a descriptive cross-sectional study where the data will be taken from the electronic clinical record.
3. Results
The total population was 237 patients, of which 165 were women (70%) and 72 men (30%). The minimum age was 26 years and maximum 104 years, with a mean of 62 years (Table 1 and Table 2).
The most affected hand was the right hand with a total of 158 patients (67%), while the left hand was affected in 79 patients (33%). In the right hand the middle finger was the most affected (45%), followed by the thumb (24%), ring finger (19%), index finger (8%) and little finger (4%). In the left hand, the thumb had the greatest involvement (34%), followed by the middle finger (32%), ring finger (24%), index finger (6%) and little finger (4%) (Graphic 1).
Of the 237 patients, 80 of them had obesity (34%), 86 had type 2 diabetes mellitus (36%), 95 had systemic arterial hypertension (40%), 43 had a positive history of smoking (18%) and 24 of them for alcohol consumption (10%) (Graphic 2).
![]()
Table 1. Sex distribution of patients with trigger finger.
![]()
Table 2. Age distribution of patients with trigger finger.
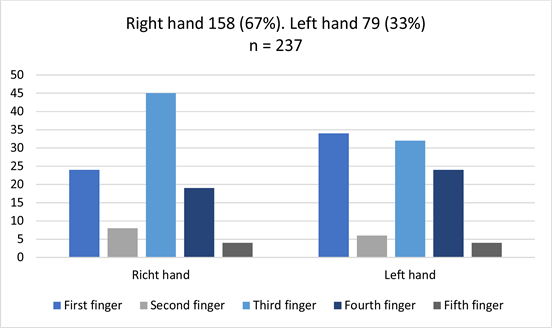
Graphic 1. Frequency of hand and finger involvement in patients with trigger finger.
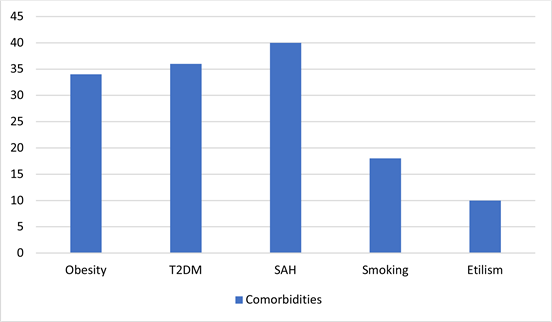
T2DM: type 2 diabetes mellitus, SAH: systemic arterial hypertension.
Graphic 2. Frequency of trigger finger associated with comorbidities.
![]()
Table 3. Frequency of surgical techniques performed for the treatment of trigger finger.
NSAID: nonsteroidal anti-inflammatory drugs.
Thirty-three percent of patients (n = 78) received corticosteroid infiltration and 58% (n = 138) were given oral nonsteroidal anti-inflammatory drugs prior to surgical treatment. Open technique was performed in 190 (80%) patients, while percutaneous technique was performed in 47 (20%) of them (Table 3).
4. Discussion
In our case series there was a higher prevalence in women and the involvement of the right hand (dominant hand in most of the population) coincides with those described in the literature. Blough et al. described a 2 - 6 times greater involvement in the female population [3] , however, Neto et al. observed that it is only twice as great in women, which is consistent with what was found in our population [8] . Another finding that was found in our population is the greater frequency of involvement of the middle finger and thumb, while in the literature the most affected fingers are the middle and ring fingers, as Lunsford et al. [2] . Gil et al., also describe the middle and ring finger as the most affected [1] . However, Blough et al. report greater involvement of the ring finger followed by the middle finger [3] .
In our study, a non-negligible percentage suffered from systemic diseases such as diabetes mellitus, arterial hypertension and obesity, a finding that coincides with those described in the literature. Blough et al. emphasize that diseases involving metabolic syndrome, especially diabetes mellitus and hypertension, are known risk factors [3] . Neto et al., in their retrospective study state that 68% of the patients had systemic arterial hypertension and 36% had type 2 diabetes mellitus, the latter finding is identical to that found in our population [3] [8] .
Most patients received medical treatment with nonsteroidal anti-inflammatory drugs and corticosteroid infiltration prior to surgical treatment. The percutaneous technique was performed in 19.8% of the patients and the open technique in 80.2% of them.
As our study is descriptive and observational, it is limited by the fact that it is not possible to conduct a random sample, which could lead to biases. However, new lines of research can be opened with randomized samples.
5. Conclusion
In our case series there are similarities with respect to the epidemiology reported in the literature, however there are remarkable differences in the frequency of involvement. The female sex was twice as frequent and the middle finger and thumb were the most affected. Most of the patients received surgical treatment with open approach and percutaneous approach in 20% of them.