Epidemiology of Gestational Choriocarcinoma: A Systematic Review ()

1. Introduction
Choriocarcinoma (CC) is a malignant neoplasm of trophoblastic tissue and is a type of gestational trophoblastic disease (GTD) [1] . These tumors are relatively rare and constitute less than 1% of all gynecological malignancies. Choriocarcinoma can occur in any form of pregnancy but is mostly preceded by a hydatidiform mole which is a benign form of GTD [2] . The incidence rates of gestational choriocarcinoma differ widely throughout the world with the highest incidence reported in Asia and the lowest in the Americas and Europe. In Asia, rates have been reported as high as 5 to 200 per 100,000 pregnancies whereas, in the Americas and Europe countries, the rates of 2 to 7 per 100,000 pregnancies have been noted [3] [4] [5] [6] [7] . These incidence rates may be based on the total number of pregnancies, deliveries, or live births [3] [8] . Comparisons of gestational trophoblastic disease incidence rates among different parts of the world are very difficult because of the methods used to determine rates [9] . The discrepancies between hospital-based and population-based data also contribute to the variation in worldwide incidence rates [8] [10] [11] .
Choriocarcinoma is more likely following a complete mole than a partial mole. In most cases, older women are at increased risk for CC. The malignant form of GTD, choriocarcinoma, can be more difficult to diagnose as the disease can develop months or many years after a prior pregnancy. A menstruation change is frequent, but it does not usually occur. Therefore, it is important to measure the hCG level in any woman of childbearing age who has unexplained metastatic disease. Biopsy of lesions without the ability to control bleeding is highly risky in this vascular disease and is not essential before commencing chemotherapy, however, where complete excision is possible, this can provide useful histological confirmation of the diagnosis and material for genetic analysis [12] .
This systematic review aims to identify and synthesize all available population-based and hospital-based data on gestational choriocarcinoma (CC) to arrive at conclusions on the epidemiology of CC and its risk factors. The worldwide incidence trend of this disease and the associated factors involved will also be determined. In this review, we emphasized reports using population-based and hospital-based approaches for evaluation rather than using case series studies. With respect to earlier literature reviews for gestational trophoblastic disease, the present study focused on recent updates and provides additional perspectives in describing the incidence and risk factors of this disease globally.
2. Methodology
2.1. Search Strategy
For a comprehensive search of medical science journals, we used MEDLINE, via EBSCO MEDLINE and EBSCO CINAHL. The databases were accessed from 1st December to 30th December 2015. The search strategy involves a combination (“AND”) of the following three sets of keywords 1) gestational OR pregnancy, 2) choriocarcinoma, 3) epidemiology OR incidence, and 4) risk factors. The references of all retrieved articles were reviewed for relevant citations.
2.2. Inclusion Criteria
The results were limited to studies that were published in the English language that included abstracts. The primary inclusion criteria were epidemiological studies of gestational trophoblastic disease, especially choriocarcinoma in women. Studies of all age groups are included. These included studies conducted in different regions of the world, such as Southeast Asia, Americas and Europe, and a global survey of choriocarcinoma. Only studies published within the last 20 years, from 1995 to 2015, were included in this review.
2.3. Exclusion Criteria
Case studies, case reports, animal studies, letters to the editor, news, and review articles were excluded. This review focused on the global incidence, risk factors, and other epidemiological data on gestational choriocarcinoma. Therefore, any studies related to molecular works, immunohistochemistry, or pathological studies were excluded. These selection criteria were used to achieve the objective of this systematic review in determining the epidemiology of gestational choriocarcinoma.
2.4. Screening of Articles for Eligibility
Retrieved articles were screened in three phases. In the first phase, articles that did not match the inclusion criteria based solely on titles were excluded. In the second phase, the abstracts of the remaining articles were screened thoroughly; any articles that did not meet our inclusion criteria were excluded. In the third or final phase, full texts of the remaining articles were read and assessed to exclude articles that did not meet the inclusion criteria or any articles that fulfilled the exclusion criteria. Duplicate articles were also removed. Systematic reviews and meta-analyses were excluded. All authors were involved in the selection and the data extraction phase. Differences in opinions were resolved by discussion between the authors. A flow chart that summarizes the article selection process is shown in Figure 1.
2.5. Data Extraction
The data were recorded as follows: 1) Author/s; 2) Age; 3) Region; 4) Gestational/ Non-Gestational; 5) Duration of study; 6) Study design; 7) Study population 8) Incidence and 9) Risk factors.
![]()
Figure 1. Flow chart of the selection process of articles in this review.
3. Results
3.1. Data Source and Selection
The searches conducted identified a total of 10 studies that met all the above inclusion criteria. In a total of 10 articles reviewed, nine were retrospective studies and one was a cohort study. All selected studies were based on several regions which are Asia (Korea, Japan, Türkiye, and China), Americas (USA, New Mexico, and Brazil), Europe (Finland, The Netherlands), and Africa (South Africa).
3.2. Incidence Rates of Gestational Choriocarcinoma
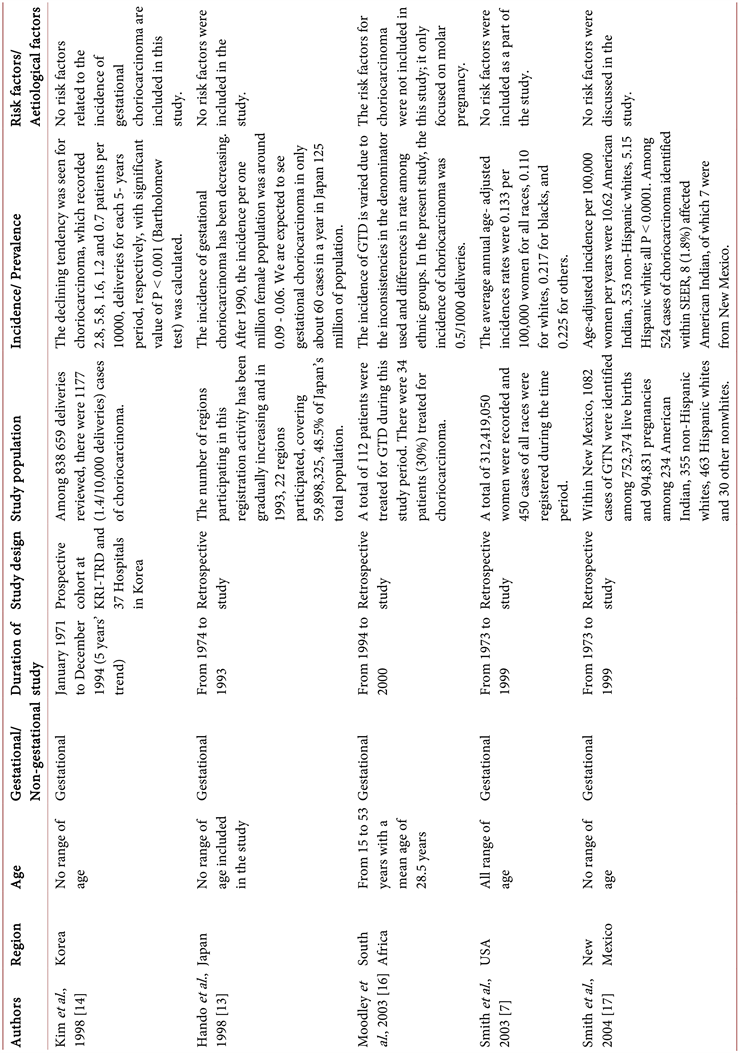
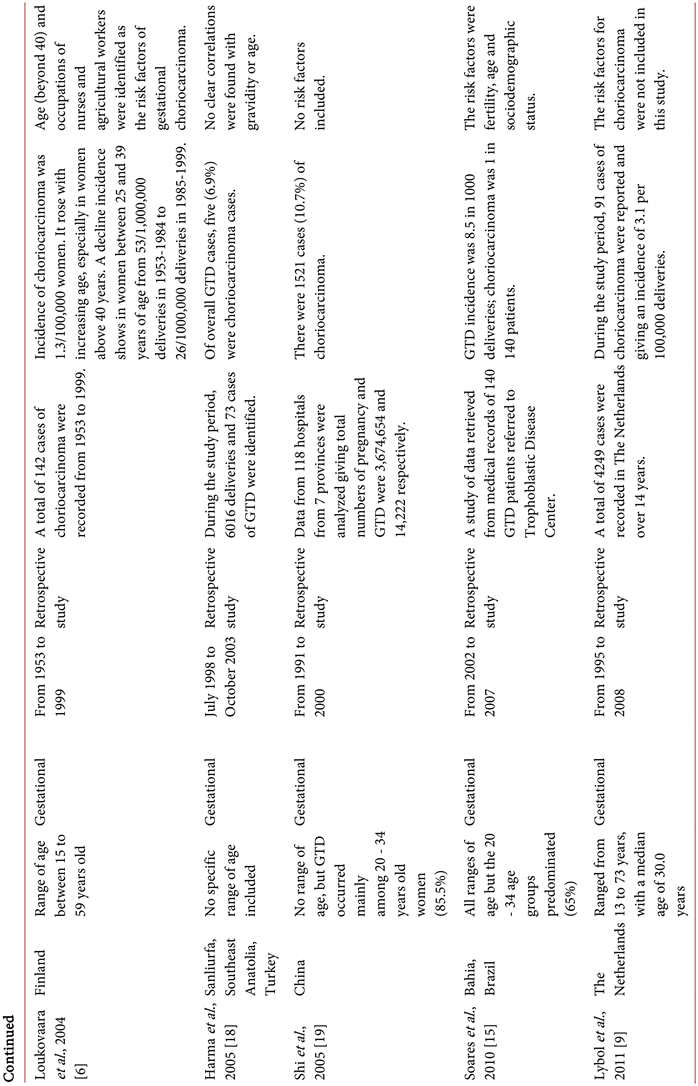
A total number of 4563 cases of choriocarcinoma were recorded from the selected articles from the year 1995 to 2015. Most studies (n = 8) stated the incidence rates of gestational choriocarcinoma during the time of their study period (Table 1). Only two (n = 2) studies clearly showed a decline in the tendency in the incidence rates of this disease [13] [14] . The distribution of studies by region according to the total number of gestational choriocarcinoma cases throughout the years was depicted in Figure 2. The data indicated the number of cases was seen higher in Asia countries as compared to other Western countries and Africa.
3.3. Association of Age with Incidence Rates
The age group involved in the studies ranged from 13 to 73 years old with a mean age of 28.5 to 30.0 years. Only five studies (n = 5) described the range of age involved, while the other five studies (n = 5) did not disclose. One study has investigated the incidence rates of choriocarcinoma in reference to age. The data indicated that the age group from 40 - 59 years showed an increase in the incidence rates as compared to others as illustrated in Figure 3.
![]()
Figure 2. The total number of choriocarcinoma cases reported globally from the year 1994-2015. [6] [9] [13] - [19]
![]()
Figure 3. The age-incidence rates of choriocarcinoma in Finland from 1953-1999. [6]
3.4. Risk Factors of Gestational Choriocarcinoma
Among all studies that have been reviewed, only two studies (n = 2) investigated the risk factors of choriocarcinoma (Table 1). Loukovaraa et al. described that ages above 40 years and occupations such as nurses and agricultural workers were the association factors for choriocarcinoma [6] . While Soares et al. reported that fertility age and sociodemographic status were also identified as risk factors [15] . Maternal age is the most consistent risk factor for choriocarcinoma. The median age for women with CC is generally somewhat higher than a normal pregnancy. There also seems to be an increased risk of choriocarcinoma in women with long-term oral contraceptive use and blood group A. Nutritional and socio-economic factors are also the most important risk factor of GTD in some populations.
4. Discussion
The epidemiological data for gestational choriocarcinoma disease was limited. Most of the epidemiological data were mainly focused on gestational trophoblastic diseases such as hydatidiform mole or molar pregnancy. This study has provided a mixture of findings. Kim et al. reported that the incidence of GTD significantly declined from 1971 to 1995 [14] . This corresponds well to the economic and medico-social advances in the country during this period of study. There was also a change in age distribution with a significant decrease in over 40 years’ age group as well as a decrease in high gravidity. The statistical significance is less reliable because the denominators of this study were based on hospital delivery statistic. No aetiological factors were reported in this paper. The difference in epidemiology between molar pregnancy and choriocarcinoma tends toward older age women without any regional difference.
Based on a study reported by Hando et al. (1998), antecedent pregnancies of 60 cases of gestational choriocarcinoma include clinical choriocarcinoma and histologically diagnosed choriocarcinoma in 1992 and 1993 were 25% of molar pregnancy, 20% of abortion and 45% of term delivery [13] . The main previous pregnancy history to choriocarcinoma is term delivery, in which molar pregnancy is less in percentage. This is probably due to the decrease in the incidence of molar pregnancy and the spread of established post-molar management systems using high sensitivity hCG measurement throughout Japan country. In contrary, countries such as Europe, America, and Asia, the incidence of GTD was much lower [16] . This could be due to underestimation as the studies were hospital based and most of the uncomplicated cases may occur in referring centers. And the risk factors were only focused on molar pregnancy cases such as maternal age, races and geographic regions.
In a population-based data by Smith et al. recorded over a span of 27 years (Surveillance, Epidemiology, and End Results, 1973-1999), the age-adjusted incidence rate for gestational choriocarcinoma per 100,000 woman-years for all races was 0.133 [7] . There was significant decrease (49.7%) over years, with an
Table 1. The incidence rates and risk factors of gestational choriocarcinoma.
annual percentage decrease of 2.8% per year. Age adjusted incidence rates were also higher among blacks and other non-whites as compared to whites but for survival rates, only blacks were significantly poorer [5] [7] . When comparing the age-incidence rate among different races such as American Indian, non-Hispanic Whites, Hispanic Whites and other nonwhites in New Mexico, among all, the American Indian women show highest incidence with 10.62 per 100,000 women per year [17] .
Furthermore, a study by Loukovaara et al. (2004) showed that the incidence rate for choriocarcinoma was 40 per million deliveries from 1953 to 1999 [6] . There was a decline in the incidence of choriocarcinoma in Finland after the year 1985. Overall, the decline was apparent only in women between 25 and 39 years of age. These could be due to the increased number of abortions and the good efficacy of chemotherapy in persistent trophoblastic disease cases in the country over the years. Variation in the age of women at delivery is not likely to explain the findings of this study. In a study reported by Harma et al. (2005), less than 10% of choriocarcinoma cases were recorded during the study period. Gravidity or age did not show any clear correlation [18] . There were few differences from the study reported by Shi et al. (2005), with 10.7% of choriocarcinoma cases recorded [19] . Soares et al. (2010) reported that out of 40 GTD cases from 2002 to 2007, there was only one case of choriocarcinoma [15] . Decrease in fertility rate and more widespread use of contraceptive use compared to previous decades can be the possible causes of decreased incidence of choriocarcinoma. Micronutrient such as vitamin E supplementation may have harmful effects in those cancerous tissues, however it must be taken with the guidance of medical practitioner [20] .
Other than that, Lybol and colleagues (2011) reported an incidence of 3.1 per 100,000 deliveries for choriocarcinoma cases [9] . This is in accordance with data obtained from other population-based studies conducted in Western countries such as Sweden, Denmark, New Mexico, and Finland. The incidence recorded was between 2.4 and 4.0 per 100,000 deliveries. The main finding of this study was on epidemiological data of hydatidiform mole; there was only a little information regarding choriocarcinoma. The overall incidence of GTD in The Netherlands was low but significantly increased over the last fourteen years. Rates found in HM and choriocarcinoma are consistent with rates seen in previous population-based studies in Western countries.
5. Conclusion
There is limited information on the epidemiological aspects of gestational choriocarcinoma. Most of the studies found concentrate on the bigger scope of gestational trophoblastic disease (GTD). GTD comprises hydatidiform mole (molar pregnancy), invasive mole, choriocarcinoma, epitheliod trophoblastic tumor (ETT) and placental site trophoblastic tumor (PSTT). Over the countries, about 20% of the studies show a decline in the incidence of choriocarcinoma while the other 80% show an inconsistencies rate. These may depend on the denominator used and differences in races and ethnic groups. In addition, the information regarding the association of age, fertility age, occupations and sociodemographic status remains to be seen. This is because out of ten studied articles, only two studies include the risk factors for gestational choriocarcinoma.
Acknowledgements
This work was supported by the Malaysia Ministry of Education Research Grant Scheme 600-RMI/FRGS 5/3 (108/2013).