The Definition of Non-Urgent Visits to the Emergency Department and Validation of Criteria for Referrals ()
1. Background
The primary healthcare setting in Israel is constituted of four non-profit health funds, or Health Maintenance Organizations (HMOs): Clalit, Maccabi, Meuhedet and Leumit. The main goal of these HMOs is to provide curative treatments for the Israeli citizens to ensure their health and well-being [1] . In urgent conditions and cases when primary care is unable to provide the patient with appropriate treatment, the family physician can refer the patient to one of the emergency departments (EDs) [2] . In addition, Israel has a National Health Insurance Law, which allows each citizen to visit the ED of hospitals by themselves, based on one’s own decision. A visit to the ED without consultation with a physician or nurse results in a payment of 1049 NIS (approximately $300). In some cases, determined by the Ministry of Health or the HMO, the patient is eligible for partial or full reimbursement by the healthcare provider (i.e., the HMO).
In Israel, EDs are the connection between primary care and hospitals. In 2020, there were about 2.6 million visits to the ED; 2.2 million did not concern pregnant women. About 27% of these visits had ended with hospitalization [3] . In 2019, the average waiting time in the ED was 3.9 hours and the average occupancy rate was 80%. Understaffed emergency departments, high workload, burnout levels, and population ageing are additional factors leading to more complex medical conditions, resulting in ED overcrowding, thus making it difficult for medical staff to provide adequate treatment [4] [5] .
One of the main causes for ED overcrowding is non-urgent (NU) or inappropriate visits [6] . “Non-urgent Emergency Department” (NU-ED) visits have many definitions. Uscher-Pines et al. (2013) used the following definition: “visits for conditions for which a delay of several hours would not increase the likelihood of an adverse outcome” [7] . Similar definition was used in other work: “visits that can be treated in the community care in case they are available there” [8] . NU-ED visitors are defined as those who attend the ED due to a prolonged medical condition [9] or in cases which can be treated in the community setting [10] . NU-ED visitors are also those whose medical conditions do not require hospitalization [11] .
Non-urgent visits to the ED constitute a global phenomenon which is a direct cause for ED overcrowding. It is well known that ED overcrowding has great implications on health workers’ well-being, quality of care, patients’ satisfaction and the efficacy and economics of heath care system [6] [12] . In many countries, overcrowding management programs are installed to reduce the number of NU-ED visits. Defining these NU visits is the first step in many of these programs [13] [14] . Considering the above, the main goal of this qualitative research is to develop and validate an algorithm for defining urgent and non-urgent visits to the ED in Israel.
2. Methods
2.1. Study Design and Population
The present study is a qualitative study that was conducted via semi-structured, open-ended interviews. The interviews collected the experience of physicians and nurses working in ED and/or primary care senior physicians from different hospitals or HMOs in Israel. The study aims to formulate and validate criteria for unjustified referrals to the ED in Israel. Based on these criteria, it will be possible to classify the referrals to the ED as urgent or non-urgent visits.
Emphasis was placed on the creation of a heterogeneous research population, with the purpose of finding the largest number of possible reasons for non-urgent visits to ED. Participants’ number was determined based on the saturation idea [6] . Referral to the participants was done using emails, intended to these specific specialists. Senior physicians working in emergency medicine, internal medicine or pediatrics, and those working in the HMOs across Israel (family physician, pediatrician or intern) for more than 3 years were included in the study. In addition, senior physicians and nurses with more than 3 years experience in ED and who were employed as a manager or director for at least one year, were also included. Physicians and nurses who did not wish to participate in the study and those who have not worked in the ED or HMOs in the last 6 months, were excluded from the study.
2.2. Sampling Method and Data Collection
A qualitative study does not require a sample size calculation, but the idea is to reach saturation of the categories. The sample size was determined by theoretical and practical thematic saturation of the data [6] . Qualitative data collection took about 3 months. Following the approval of the health facilities in which subjects worked, participants were recruited through professional email listservs with information regarding the study goals. Subjects were invited to participate in 1 h semi-structured in-depth interviews including general and specific questions regarding the progress of non-urgent visits to ED. The participation in this study was done voluntarily. After 12 interviews, we achieved thematic saturation and a balanced sample based on practice settings. Purposive sampling was done—four senior doctors, four nursing managers in medical centers across the country and four doctors with managerial rank were selected—a total of 12 participants [6] .
We developed and used a semi-structured interview guide consisting of open-ended questions organized in a progressive sequence to ensure topics were addressed systematically across participants. The research team developed questions based on our literature review on the topic and clinical experiences. Face-to-face and online interviews (using Zoom) were conducted individually with each participant. Place and time of the interviews were determined according to the convenience of the interviewees. Every interview lasted about one hour and was recorded following signing up informed consent. When necessary, another completion interview was arranged. Afterwards, these interviews were transcribed and analyzed to determine possible reasons for NU visits to ED. A list of possible criteria for NU-ED visits was constructed based on the words of the interviewees and while obtaining agreement between the interviewees.
In addition, during the interviews, theoretically representative clinical cases were presented with possible reasons for referrals to the ED. The cases were presented while classifying requests to the ED as justified and unjustified by the interviewees. In order to determine the urgency of contacting the ED, reference was made to laboratory tests, imaging tests, medical operations, treatments and diagnoses, which were conducted as part of the visit and documented in the discharge sheet from the ED. According to the criteria defined, it is possible to classify the referrals to the ED into urgent and non-urgent visits and characterize them at the population level. The following conditions were classified as urgent or non-urgent: MRI (magnetic resonance imaging), CT (computerized tomography) scan, CT angiography examination, doppler, electrocardiogram and echocardiogram, cardiac troponin, D-dimer test, ammonium laboratory tests, cut sewing, casting a limb after a fracture, administrating fluid infusions, diagnosis of a “femoral neck fracture”, removal of an ingrown toenail, tendon suture, enema, gastroscopy, bronchoscopy, chest or abdominal pain and treatment given under sedation.
2.3. Data Analysis
Qualitative data analysis was performed by a conventional content analysis [15] [16] . Briefly, participants’ answers were categorized into several categories and sub-categories, based on their content. According to this method, the content categories were extracted directly from the interview data. A list of the reasons for NU visits to ED, according to the interviewees, was compiled. This list was organized according to categories and subcategories, uniting similar categories on one hand, and splitting categories into several subcategories, on the other hand, as needed. This process led to the development of an algorithm for defining urgent and NU visits to the ED.
3. Results
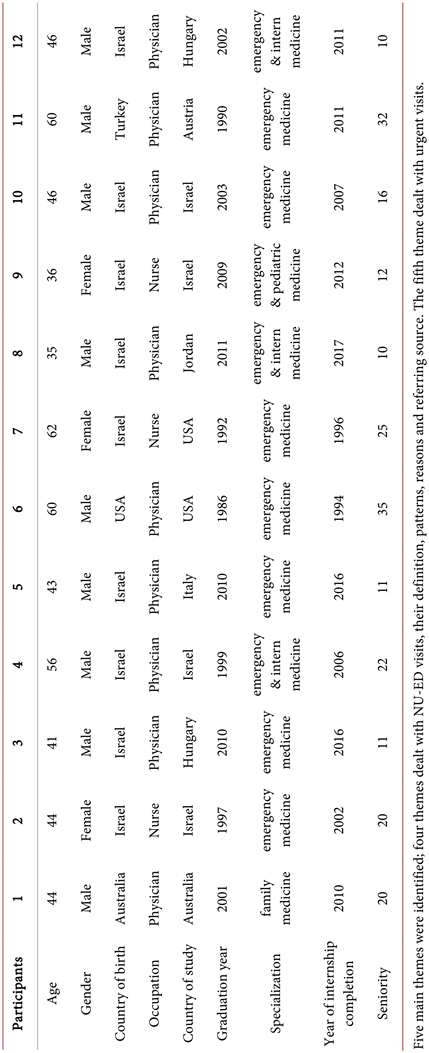
Twelve physicians and nurses participated in this study. Among the participants, three were females and nine were males. All females are nurses, and all males are physicians. Most of the participants were born in Israel and studied in other countries. Seniority ranged between 11 and 35 years. Most of the participants were specialized in emergency medicine (Table 1).
3.1. Definition of NU-ED Visits from Nurses’ and Physicians’ Perspective
3.1.1. Definition of NU Visits to the ED
At the beginning of the interview, the participants were asked to define NU-ED visits. For some of them, there was a certain difficulty in defining the phenomenon, probably because of the issue of defining what is “urgent”. This can be understood from Z.’s words: “...This is a really very complex issue, very difficult to say...” There is a difficulty in determining the urgency of a referral before performing the tests, as can be seen in H.’s words: “...you treat people who should not necessarily have come to the emergency room and they want to go home quickly, and we want to help everyone. It is not possible to know at that moment who is justified and who is not until a medical team examines the patient. That is why it is not possible to know in advance...” Y. said that “all visits are urgent, but some of them can be treated in the community”. Most of the participants stated that the urgency level should be defined based on the triage scale (1 - 5). Thus, inquiries that rated on the triage scale 3, 4 or 5 (mainly 4 or 5) are usually not justified and in most cases can be treated outside the ED. Another definition was based on the urgency of the treatment, whether it can tolerate a delay and be given in a few hours or a few days. In addition, participants stated that NU-ED visits include cases where the patient is not hospitalized and do not need tests such as CT, ultrasound, MRI, treatment under sedation, special laboratory tests that do not exist in HMOs, and advanced treatments that must be performed in a hospital and are not available in the community.
3.1.2. Effect of NU-ED Visits on ED Overcrowding
Participants were asked to describe how the phenomenon of NU referrals manifests in ED and how it affects the load levels. All participants reported experiencing high burden and workload every day in their workplaces. In addition, it is evident that participants are aware of the impact of unjustified referrals on this burden. However, many of them thought that these NU visits were intentional. They described a phenomenon in which family physicians are often referring patients to the ED, in cases when the availability of a specific test in the HMOs is much lower than in the ED. For example, participant A. stated that in his area of work, emergency medical services in HMOs are not available and therefore there are many NU-ED visits: “…in Israel we do not have enough community services to respond to all patients at all hours of the day...”.
3.2. Manifestation of NU-ED Visits Phenomenon
3.2.1. Patterns of NU-ED Visits
According to the participants, most NU-ED visits occurred outside the working
Table 1. Socio-demographic and professional characteristics of study participants.
hours of HMOs, during nights and weekends. G. stated “...the phenomenon manifests itself at selected times of the day, for example when medical centers near to my hospital are closed (11:00-00:00)...”.
In addition, many patients were referred by their family physicians to ED for further investigations or to carry out certain tests or to receive an answer from a more specialized expert in the ED, when in fact the answer can also be given within HMOs. G. stated “...many inquiries are in need of a completion of the medical investigation that started in the community and can certainly continue in the community as well, but for some reasons they are referred to the hospital. Some inquiries might require medical advice only by a professional doctor such as an ophthalmologist, neurologist, urologist (testicles) solely due to a lack of service in the community. Moreover, there is a lack of communication between doctors in the community and doctors in ED, and there are no doctors specialized in emergency medicine who are present in medical centers and can provide an answer...” Moreover, D. stated “...we see a lot of shortage of appointments for imaging, as well as minor medical cases with unclear referral reasons to ED. Around 15% of referrals are unnecessary...”.
3.2.2. Numbers of NU-ED Visits
The participants were asked to roughly estimate the percentage of NU-ED visits. It is important to note that at this stage, most of them mentioned referrals given by a qualified person such as a family doctor, a professional doctor or a nurse. A large variation was found in the estimation of NU-ED visits: between 10% - 80% (depending on the time of day and day of the week). This wide range is explained by the type of ED (adults vs. pediatric, lying vs. mobile etc.) and its geographical location. This can be understood from H. who stated that there is a difference between mobile and lying ED: “...This is an answer that depends on the wing I am working in. We have a walking wing and a lying wing. There are patients who come to the ED lying down; at least 1 - 2 patients could be treated in ambulatory setting. These are patients who are less mobile and may need more medical help. At the community, about 70% of arriving patients could be treated within the HMOs…”.
3.3. Main Reasons for NU-ED Visits
Several questions dealt with the reasons for unjustified referrals to the ED.
3.3.1. Complaints for Which Patients Turned to ED
Most NU-ED visitors complained about high fever, small burns and wounds, chronic conditions or asked to perform tests which are barely available in HMOs. Most of the participants stated that in many cases NU visitors’ complaints could be solved in the HMOs. Several participants emphasized that when seeking treatment for chronic conditions, the problem cannot be solved immediately at ED. Most problems of this type will require adjustment of treatment and follow-up in the community, so it can be assumed that it is unnecessary to go to ED in these cases, as H. said: “...for example, a patient who has been suffering from back pain repeatedly for several months goes to the emergency room because he has not found an appropriate solution through a family doctor or in the community. In the event that he goes with the intention of solving the problem altogether, we have no way to help him, since ED intend treatments for acute cases. It will be possible to alleviate his pain at the moment, but to balance chronic pain he needs a pain clinic or a follow-up with a spine specialist...”.
Often people turn to ED out of a need for treatment or attention, as Z. emphasizes in his story the wrong way in which ED is perceived by patients and the health services working outside the hospitals: “...one day a guy came to me, it was quarter past eleven at night. He looked perfectly fine, and he came for a toothache. Then he said to me: “Just so you know, I’m under house arrest and I just wanted to get out of the house for a bit to get some fresh air, so I ordered an ambulance. And I have to call to let them know I’m in the hospital, I don’t care, how many hours it takes, I’m fine, I’ll be fine. He just wanted time off”.
3.3.2. Logistic and Personal Reasons for NU-ED Visits
Since most of the clinics in the community are open at specific hours and not during the afternoon, evenings, nights or weekends, many patients cannot get the treatment in this setting. Attending urgent care centers, available in some cities with longer working hours, can be a solution, although many patients still choose to attend the Eds.
In terms of appointments’ availability, many patients have to wait weeks or even months for the appointments they need in order to find out their medical condition, monitor it and adjust treatment. Patients often apply independently or are referred by a care provider in cases where it is necessary to perform a procedure or test, for which the queue in the community is very long. As G. reported: “...most of the reasons are logistical or administrative and do not arise from the patient’s true level of urgency and the need for treatment. The reasons can be related to completing a medical investigation by means of diagnosis that is not available at the time in the community. A significant part of NU inquiries is intended for a medical advice by an expert in some field and is sent to ED to shorten the waiting times for that doctor in the community...”.
Moreover, for many people, everyday life does not allow access to the necessary inquiries during daytime hours. Therefore, these people turn to ED even in chronic cases out of convenience. B. pointed: “...over the years, working in shifts, there are many inquiries from people during non-hours, because it is convenient for them, because they think that they will receive the full services of the hospital as part of a visit, instead of making appointments and running around in the hospital. There is a widespread opinion among the public that there are specialist doctors in ED in every field at every hour of the day, but we know that reality is not like that...”.
3.3.3. Unique Patterns
There are unique contact patterns for some ED, such as the case of pediatric ED in Israel where the capacity of visits is maximum for 24/7. The second case concerns non-Israeli citizens who cannot get medical treatment in the HMOs if they do not have a suitable medical insurance. In these cases, they attend the ED and get the required treatment regardless of the urgency of medical condition.
3.4. Referral for NU Cases
The referring source was one of the most frequently reoccurring factor in the interviews. The participants chose to repeatedly mention the fact that many patients come to ED in unjustified cases as a result of referrals made by family physicians, specialists’ physicians, medical home services at various centers and different medical call services.
3.4.1. Referrals by Family and Expert Physicians
According to the interviews, the family physician is the main referring source for NU reasons. The main reason for these NU referrals is a lack of understanding and knowledge of the role of ED, as A. stated: “there is a phenomenon of patients being referred by professional doctors who are too lazy to perform operations in the community despite that they are expected to do so. Some of the inquiries are done because of a lack of knowledge about the services available in community medicine…” The second reason is the inability to treat the patient properly with the given resources or system constrains (long waiting lists for medical inquiries, treatments, meeting with specialist physicians etc.).
3.4.2. Referrals by Nurses from the Call Center
Referrals by nurses from call centers are another main referral source. As stated in the interviews, since these nurses are not meeting the patients in person, they must provide the appropriate treatment that will ensure the patient’s well-being. This might explain why their referral rate is rather high. Furthermore, many patients choose to refer themselves to the ED, without medical advice, contributing to ED overcrowding. Y. stated: “...in the centers, and certainly if it’s just a phone call and not a video, nurses work according to protocols. If the patient mentions some code word, the protocol indicates that the nurse should refer him to ED...”.
3.5. Reasons for Urgent ED Visits
At the end of the interview, the participants were asked to give several examples of justified reasons for ED visits.
3.5.1. Relevant Laboratory Tests
Most of the participants listed a number of laboratory tests that require attendance to the ED, such as cardiac troponin and D-dimer. Although, most of these tests are also available in the urgent care centers. Nevertheless, the results of these examinations can require immediate treatment that can be supplied in hospitals only. Some laboratory analyses, such as ammonium test or metabolic spectrum, are only done in hospitals and not in community.
3.5.2. Relevant Imaging Tests
Participants indicated some imaging tests as urgent, such as MRI, CT scans, ultrasound, Doppler and echocardiography. Participants emphasized that these tests should be performed in the ED only when they are not available in the community and there is an urgency to perform them. H. said “...imaging tests such as CT and ultrasound, which are most commonly used in ED, can also be performed within the community depending on patient’s diagnosis. In the case of a patient with a known history of kidney stones and complaining of back pain, there is no medical need to perform an ultrasound for the urinary tract stones as this is not a solvable condition in the ER. The patient will need follow-up and pain relief treatment that can be given in the community...”.
3.5.3. Relevant Treatments
A number of treatments that are carried out in urgent cases in ED are also available in the community, but their availability is low. To mention few, chest or abdomen drains, shoulder replacement, decompression of the digestive system, removal of foreign bodies from the pharynx or eye that mostly requires use of optical fibers or microscope. T. stated that treatments given in trauma or shock rooms are exclusively performed in ED.
In pediatric cases, any treatment that requires sedation, incisions, sutures, lumbar puncture, as well as reduction of fractures, must be performed in ED.
3.5.4. Relevant Diagnosis
Chest pain and abdominal pain are two relevant reasons for referring to ED. In these cases, other health parameters of the patient should be considered, justification can be based on various reasons and not necessarily on life-threatening situations. Participants mentioned a series of specific relevant diagnoses: multi trauma, head injuries in people treated with anticoagulants, renal colic with fever, severe COPD (Chronic Obstructive Pulmonary Disease), epistaxis under anticoagulants and more.
3.5.5. ED Referrals during COVID-19 Outbreak
The interviews took place at the end of 2020 to the middle of 2021, a period in which a high incidence of COVID-19 was observed. Thus, the topic of the corona epidemic came up a lot in the interviews and received similar interpretations from the seniors in emergency medicine. Several phenomena were very common in EDs during this period. Since COVID-19 tests were not available in the HMOs, many patients arrived to the ED in order to perform the test. Additionally, during lockdowns, a decrease in the general number of ED visits was observed, most people preferred to postpone a visit to a hospital in order not to be exposed to the virus and thus may have postponed treatment of medical problems, which needed attention without delay at that time. The ED became the place where positive COVID-19 patients got medical treatments, since they were not allowed to arrive to HMOs, as stated by T. “a corona patient with a bruised finger or rubbing of the knee or back pain or any other complaint was referred via a phone call only to the emergency room—by default for the purpose of receiving medical treatment for corona patients. There were no other settings in the community for corona patients and only now there is a glimmer of the possibility of treating them at home by protected teams...”.
4. Discussion
The main goal of this work was to define criteria for NU visits to the ED. NU-ED visits are very common worldwide and their negative effect on ED overcrowding, patient’s satisfaction, healthcare worker’s burnout and treatments’ effectiveness is great [7] . As a matter of fact, NU-ED visits affect all the health system. To understand the way senior physicians and nurses working in the EDs or HMOs perceive NU-ED visits, we first asked them to define this phenomenon. Most of them stated that NU or urgent visits should be distinguished based on the answers for the following questions: 1) Does the medical condition require an immediate treatment? 2) Is ED the only place that can provide the required treatment at the certain timepoint? Similar definitions were given previously by other researchers [7] .
NU-ED visits occur mostly during the afternoon, evening, night and weekends, when medical treatments are not available in the HMOs. These visits also occur due to a low availability of diagnostic tests and treatments in the HMOs. Similar trends were found in other researchers’ works that dealt with NU-ED visits worldwide [17] . According to the twelve participants’ answers, 10% to 80% of the ED visits are NU. In other works that are mostly based on different relevant databases, observations reported a very different range of 20% - 40% [7] [18] . Very often in these works, the definition of NU-ED visits is not clear [7] [18] .
As reported by the participants, the main reasons for NU-ED visits include minor injuries, chronic conditions, fever, abdominal or chest pain. Some of them noted that these reasons might sometimes turn out to be urgent, but in most of the cases, they are not. One of the main reasons for NU-ED visits is referral by physicians who percept a given medical condition as more urgent than it really is [19] [20] . Another reason for NU-ED visits is the availability of ED in terms of hours or geographical location. The possibility of attending the ED in any time is a central factor affecting patients’ decision even in NU cases. Moreover, many patients perceive the medical staff in the ED as more professional than in the community. These patterns are in accordance with other studies [21] .
The main source for NU-ED visits is referral from a family physician or nurse from the call center. Both family physicians and call center nurses are considered to have the required skills and knowledge to differentiate between urgent and NU medical conditions. Indeed, for the same reason, there are low chances that a patient would visit the ED without a referral from the family doctor [22] . Often in the community, there is a lack of awareness and knowledge about the roles of ED and the available options in HMOs. In addition, appropriate treatment can not always be provided in the community. Finally, participants stated that some procedures and conditions are urgent enough to attend the ED, such as cardiac troponin, D-dimer, blood gases, ammonium laboratory test; MRI, CT, doppler and echocardiogram; treatment given under sedation and complains of chest and abdominal pain.
COVID-19 outbreak in its different stages also had great influence on NU-ED visits. Surprisingly, during the first outbreaks and lockdowns, people were afraid to leave their houses without a worthy reason. A decrease in the general number of ED visits was observed, most people preferred to postpone a visit to the hospital in order not to be exposed to the virus.
A great tool to reduce NU-ED visits is the usage of the triage scales that help to ensure patients are getting treated based on the clinical urgency of their case. Using this scale, it only takes few minutes to determine the urgency level. These scales mostly range between: (1) life risk situation that requires immediate diagnosis and treatment to (5) chronic condition that can be treated in the HMOs. According to the participants in this study, medical cases that scores above 3 in the triage scale, can be treated in the HMOs and can be defined as NU-ED visits. Therefore, implementation of these scales in the community and their use in the decision making of ED referrals by family physicians and call center nurses, might greatly reduce NU-ED visits.
5. Conclusions
The main goal of this work was to define NU-ED visits and to determine and validate criteria for urgent and NU-ED visits. According to the participants, an appropriate reason for urgent ED visits is when a given medical situation must be treated immediately and there are no treatment options in the HMOs. It was found that most NU-ED visits occur in times when the HMOs services are not available, mainly due to convenience and availability considerations. These visits had negative effect on health services. Most participants repeatedly mentioned that many family physicians and nurses from call centers refer patients to the ED instead of providing them with the adequate treatment in HMOs or urgent medical centers. Low awareness of the role of ED, low availability of certain tests in the HMOs, and inability to provide the appropriate treatment in the community clinics are reasons behind these referrals. Finally, the participants noted reasons for appropriate ED visits, such as several laboratory tests, imaging and specific treatments, although these options are also available in the HMOs. It is important to note, that in Israel, the Ministry of Health is obligated to maintain a triage process in emergency medical departments in general hospitals 24 hours a day by qualified staff members, while maintaining structured work processes and quality control.
Specifically, the following triage methods are implemented in Israel:
1) Canadian triage and Acuity scale (CTAS)
2) Australian triage scale (ATS)
3) Emergency Severity Index (ESI)
The implementation of the triage scales in the community might greatly reduce NU-ED visits.
We believe that the Ministry of Health in collaboration with HMOs should implement communication programs to educate the public about the role of an emergency department and the necessity of referring a patient to a family physician before going to ED. At the same time, it is important to publish addresses of clinics and urgent medical centers, where primary medical care can see patients in cases that do not require an ED.
In addition, consideration should be given to implementing educational programs in higher educational institutions and workplaces regarding the importance of early treatment in the community and the avoidance of last-minute ED visits, while at the same time empowering and staffing initial health services in the community.