
1. Introduction
Kodamaea ohmeri, previously known as Pichia ohmeri, is an ascomycetous yeast that belongs to Saccharomycetaceae family [1]. This yeast was widely used in the food industry for fruits, pickles and fermentation [2] [3]. Often misidentified as a Candida [4] [5], there have been reported cases involving predominantly immunocompromised patients with one or more predisposing factors [2] [6], suggesting that this yeast is now recognised as pathogenic for humans.
2. Case Report
An obese 60-year-old lady with diabetes, hypertension and bilateral obstructive uropathy secondary to bilateral ureteric calculi, presented with right loin pain, and one week after change of right ureteric stent. Clinically was stable and not in sepsis, with temperature of 36.9 degrees celsius, and clinical examination was unremarkable except for renal punch positive on right side.
Lab parameters were as follows: white cell count 32 (4.0 - 11.0 × 109/L), haemoglobin 11 (13.0 - 18.0 g/dL), platelet 267 (150 - 400 × 109/L), urea 36 (2.5 - 6.5 mmol/L), sodium 117 (135 - 145 mmol/L), potassium 5.5 (3.5 - 4.5 mmol/L), creatinine 532 (62 - 115 mmol/L), and C-reactive protein 10 (0.5 - 2.0 mg/L). urine for fine and microscopic examination unremarkable, blood gas not acidotic. Hepatitis B, Hepatitis C and HIV screening were non-reactive. Her glycated haemoglobin HbA1c was 6.8%.
Computed Tomography Urography (CTU) performed after the change of ureteric stent revealed right peritoneal collection, which was likely due to ruptured right upper ureter with malposition of right proximal ureteric stent. Ultrasound guided percutaneous drainage of right peritoneal performed yielded a sterile peritoneal fluid culture. Patient was treated with intravenous augmentin for three weeks. Subsequently she had carbapenem-resistant Acinetobacter baumannii (CRAB) central-related bloodstream infection (CRBSI) and was treated with intravenous meropenem for ten days.
Subsequent Computed Tomography (CT) scan of intravenous urography (IVU) showed fistulous communication between D2/D3 duodenum with the right peritoneal collection. To allow the bowels to rest, a peripherally inserted central catheter (PICC) was inserted for Total Parenteral Nutrition (TPN).
Shortly after, patient developed a new episode of sepsis and subsequent serial blood culture yielded Kodamaea ohmeri fungemia identified by MALDI-TOF MS.
She was started on IV amphotericin B deoxycholate while awaiting fungal sensitivity report. She had her PICC removed and her general wellbeing immediately improved. After 2 weeks, IV amphotericin B was withheld due to acute kidney injury complication. As the minimum inhibitory concentration (MIC) of the isolated Kodamaea ohmeri was anidulafungin 0.016 µ/mL, the antifungal agent was changed to IV anidulafungin. Subsequently, patient’s general condition markedly improved with anidulafungin without surgical intervention.
Transthoracic echocardiography (TTE) showed no vegetation and slit lamp examination revealed no evidence of endophthalmitis. There was persistent Kodamaea ohmeri fungaemia for over three weeks with persistent large amount of purulent discharge from peritoneal drain (Image 1). However, it eventually cleared one week after the patient was switched to IV anidulafungin.
Patient was discharged well with oral voriconazole with follow-up at clinic. Reassessment CT abdomen/pelvis two weeks later showed resolving right posterior para-renal collections.
Morphology of white creamy colonies of K. ohmeri after 24 - 48 hours incubation at 35˚C - 37˚C on chloramphenicol-added Sabouraud dextrose agar. (Images 2-4)
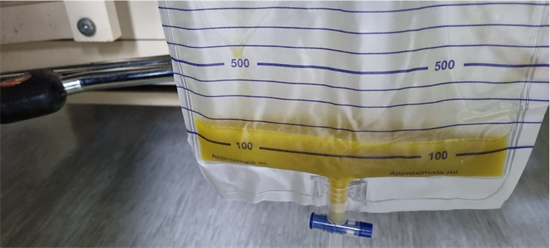
Image 1. Purulent discharge from peritoneal drain.

Image 2. Surface.
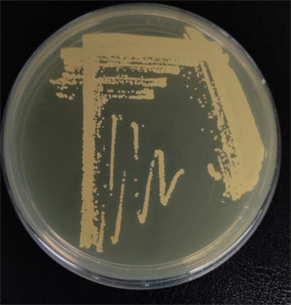
Image 3. Reverse.
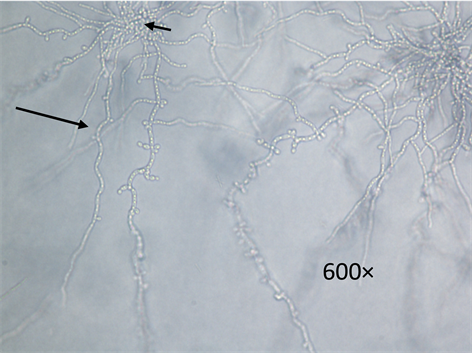
Image 4. Wet mount prepared from a 24 - 48 hour-old culture of K. ohmeri grown on Cornmeal agar. The yeast cells were ovoid to cylindrical with pseudohyphae (long arrow) and blastoconidia (short arrow) seen under light microscope.
3. Discussion
Kodamaea ohmeri is an emerging rare yeast infection and potentially life-threatening especially in immunocompromised patients [1] [2] [7]. Potential risk factors for Kodamaea fungal infection include intubated and ventilated patients with prolonged hospital stay, prolonged intravenous antibiotics, indwelling catheters, fluid infusion, implants, diabetics, and underlying malignancies [8].
This patient, an elderly with diabetes mellitus had an invasive urology procedure with complications. She also had a prolonged course of broad-spectrum antibiotic prior to the diagnosis of the fungal infection, plus an indwelling catheter in an immunosuppressed patient further facilitated the fungal infection.
The patient had a recent invasive urothelial procedure that was complicated by an intra-abdominal injury, which further created a persistent fistulous communication between duodenum and peritoneum. There was also prolonged course of a large peritoneal drain (Image 1). The fungal blood stream infection can be associated with patient’s malnutrition status and mucosal breach [8]. Although there is no growth obtained from peritoneal culture, we deduce this might be due to inadequate sampling or early infection with low fungal yield. Despite central line catheter removal, the blood culture yielded persistent Kodamea ohmeri which raised suspicion of peritoneal in origin. In addition, longer duration of clearance of the fungaemia, in this case, suggests a higher volume distribution due to her obese stature [9].
The fungal identification was performed via blood culture sampling and incubated using BACTECTM Plus Aerobic/F Culture Vials and anaerobic/F Culture Vials. Both aerobic and anaerobic bottle yielded yeast-like organism after 48 hours incubation at 35˚C. It is detected through wet mount preparation (Image 4).
![]()
Table 1. Antifungal susceptibility testing test report.
The cultivation of yeasts done on chloramphenicol-added Sabouraud dextrose agar for 24 - 48 hours of incubation at 35˚C - 37˚C in an aerobic condition. It appeared as candida-like colonies on solid medium. Over 48 hours of incubation, the yeast Kodamaea ohmeri grew as white creamy colonies that can be seen on surface and reverse of plate (Image 2 and Image 3).
Matrix-assisted laser desorption ionization time of flight (MALDI-TOF) mass spectrophotometry further confirmed the identification. Susceptibility of antifungals was made by E-test. The minimal inhibitory concentration (MIC) of the antifungal agents is in Table 1.
4. Conclusions
Early diagnosis of fungal infection such as Kodamaea ohmeri is crucial, with immediate removal of indwelling catheters to ensure adequate source control and optimum treatment with appropriate antifungal therapy. There should be a high index of suspicion for early recognition for this pathogen to initiate prompt appropriate antifungal therapy. In this context, molecular identification method using MALDI-TOF proved reliable to identify K. ohmeri with 99.9% confidence. MALDI-TOF MS is fast and accurate in identification of fungal and bacterial species with the sensitivity and accuracy being comparable to PCR.
In addition, antifungal sensitivity testing has variations in susceptibility that poses challenges in management. More publications are needed to establish optimal antifungal regimens.
Funding
This article receives support from the “Persatuan Pendidikan Perubatan PASCA Ijazah” Selayang Hospital Funds.