Rapid Evolution of a Case of Choriocarcinoma Following Normal Delivery at Term Pregnancy ()
1. Introduction
Among the trophoblastic diseases, choriocarcinoma is the most faired. It often follows complete mole, abortion or ectopic pregnancy. It sometimes happens following normal pregnancy delivery. His signs could be observed as pelvic pains, asthenia, nausea, or vomiting. The most frequent signs are metrorrhagia, genital tractus discharge loco regional metastasis manifestations (pain, dysuria, hematuria etc. The diagnosis is by plasma beta chorionic gonadotopin hCG) quantitative assay showing a high level rate. Generally this trophoblastic pathology is cured by antimitotic drugs, we report a choriocarcinoma case diagnosed six months after full-term pregnancy delivery.
All ethics and deontological protocols rules are respected.
2. Clinical Case
We report a case of choriocarcinoma diagnosed ten months after childbirth.
This is a case of 32-year-old patient, gravida second and para second. She had a history of delivery by caesarian in 2015 of her first full-term pregnancy with a living child. At this second full-term monofetal pregnancy, she delivered well living newborn by caesarian section in January 2020, with normal immediat recovery. She did not breastfeed her son.
From March 2020, she used estrogen/progestogen mini-dose oral contraception for one month, then micro-progestative pill for 2 months and estrogen-progestogestative mini-dose pill for 5 months. She suffered of metrorragia from October 16, 2020 following the discontinuation of contraception. An emergency curettage was provided somewhere on November 10, 2020 (histological exam not done). Repeated βhCG assays were done on November 11, 2020 (4495 mIU/ml), November 12, 2020 (3967 mIU/ml) November 13, 2020 (1031.14 mIU/ml), November 20, 2020 (2561 mIU/ml) and November 23, 2020 12267.94 mI/ml.
We received the patient for the first time on November 27, 2020 for moderate metrorragia. The gynecological examination, showed at the anterior vaginal wall under the urethra a non-hemorrhagic friable and irregular tumor of 20 mm long/10mm wide. We did resection of the tumor for histologic exam. The ultrasound showed enlarged uterus full with heterogen content (the images can not be pinted because very dark), no lutein cyst seen. At general clinical exam we did observe any pathologic dysfunctional signs of the other organs. Hepatic ultrasound and chest radiography were normal. Other exploration like magnetic resonancy image (MRI) were not done. The histology of the biopsy concluded with a choriocarcinoma (Image 1 and Image 2). She was admitted in the Institute of Radiotherapy (National Cancer Center). The patient received a first treatment by antimitotic therapy according to the following protocol:
Anti-emetic (levosulpiride 25 mg) by slow intravenous injection before and after chemotherapy, Detamethasone 8 mg by slow intravenous injection and 400 mg and cimetidine by slow direct intravenous injection and Infusion of 100 ml of 0.9% saline solution for 15 minutes, then 50 mg of methotrexate in 500 ml of glucose serum 5% for 60 mins then 100 ml of 0% saline over 15 mins.
We received her again two months later, she presented with a second location
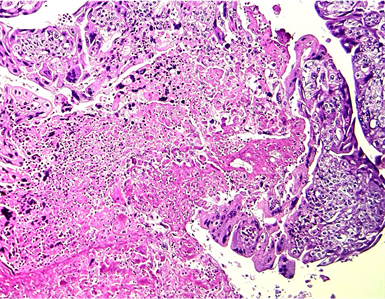
Image 1. The histological image shows a largely necrotic tumor made up of cytotrophoblacs (mononuclear cells) associted iwth synticiotrophoblasts (multinuclear cells) with atypia and mitoses (haematozylin—eosin × 100).
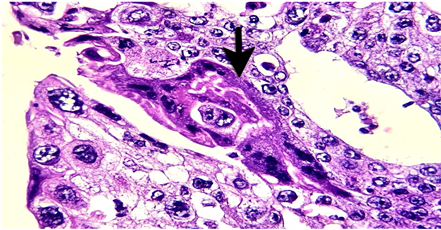
Image 2. High magnification, the cytotrophoblasts are equipped with an eosinophilic cytoplasm and oval nuclei with heterogeneous fine chromatin. Presence of a syncytiotrophoblastic giant cell (arrow) with several irregular nuclei (haematoxylin—eosin × 400).
of the tumor on the posterior vaginal wall. A second chemotherapy round of with other molecules durgs was proposed, but she decided to go somewhere hopping better care.She died May 2021.
3. Comment
This case of choriocarcinoma following a full-term pregnancy raises some questions. The patient had no pathological pregnancy history. The tumor happened after full term delivery pregnancy. Oral hormonal contraception was irregulary observed, changing drugs in short intervals time. Did hormonal contraception hurry the evolution of the tumor? A case of choriocarcinoma is reported in a patient who used the Mirena IUS intrauterine device with good prognosis [1]. For our case metrorrhagia episods were the first s manifestations requiring curettage (no anatomopathological exam provided of the removed products), despite this act the metrorrhagia continued. Postpartum choriocarcinoma has a propensity for early metastasis. The most frequently observed metastatic locations are lungs (80%), vagina wall (30%), the brain (10%), liver (10%) [2], if the time between childbirth and diagnosis is less than 4 months in 50/121 cases of choriocarnomas follow a full-term pregnancy [3]. An exceptional a case of both mother and the child was reported with favorable consequence [4].
The choriocarcinoma can have an intraplacental development. This event could de discovered on anatomical examination showing on section bicolor appearance of the parenchyma and some nodular whitish lesions [5] [6]. A pregnancy with difficult evolution (episode of metrorrhagia, fetal growth retardation, continuous or intermittent metrorrhagia, etc.) should attract attention for a systematic anatomopathological examination of the placenta. Unfortunately in Niger tradition, the placenta is systematically collected by the family and buried.
4. Conclusion
Sometimes choriocarcinoma develops following normal pregnancy. delivery. Then, partum metrorrhagia,must inqure skilled exploration of genital tructus and plasma beta chorionic gonadotopin quantitative assay.