Early Clinical Improvement of the Axial Pain after Sagittal Curve Restoration in Patients Who Underwent a Multiple Level Microdiscectomy with Fusion of the Cervical Spine Using Zero Profile Cages ()
1. Introduction
The ACDF is a highly popular procedure that is commonly performed in individuals who have cervical disc prolapse or a degenerative cervical spine.
Despite the fact that the majority of patients have excellent outcomes [1] [2] , some of them are concerned about postoperative pain [3] .
The bulk of this pain is axial, which necessitates immediate physical and pharmacological treatment.
This axial pain has been linked to a poor lordotic alignment.
The lordotic alignment influences the cervical spine’s flexion extension dynamic [4] [5] and may cause pain by putting a different stress on the neck muscles and cervical vertebrae.
We anticipate that correcting the alignment will result in an early reduction in axial pain.
The purpose of this study is to look at the relationship between restoring normal cervical spine lordosis and the persistence of axial pain in the early post-operative period in patients who had a degenerative cervical spine and underwent a multiple microdiscectomy with fixation fusion using a 0 profile cage fusion.
2. Methods
18 patients received multiple ACDFs with 0 profile cages, bone grafts, and screws fixation for a multiple level degenerative cervical spine.
Prior to surgery, all of the patients had an aberrant cervical curve.
Before and after the surgery, the sagittal lordosis was measured.
Visual analog scale (VAS) and neck disability index were used to assess pain (NDI).
Depending on the sagittal curve restoration, we divided the patients into two groups:
Patients in Group I have an aberrant cervical spine curve, either a straight or kyphotic neck. Neither could be fixed with surgery.
After surgery, participants in Group II had a normal restored lordosis.
All patients had their axial and radicular pain evaluated preoperatively and again 2 - 4 weeks following surgery.
3. Results
Eighteen patients with cervical degenerative spine disease had a multilevel ACDF procedure that included microdiscectomy, osteophytes removal, and fusion with zero profile cages and bone transplant.
The participants’ ages ranged from 36 to 64 years old.
The pain was assessed before surgery and shortly after surgery, with a time period of 2 to 4 weeks to adapt the early care. VAS was used to assess the pain in the neck and upper limbs.
The neck disability index was also assessed both before and after surgery.
In total, there was a considerable improvement in pain following surgery, with 12 patients experiencing immediate relief from radicular pain (the p-value is 0.00729). This finding is statistically significant (p 0.05). After surgery, 11 of the 18 patients were free of axial discomfort (the p-value was 0.0032). At p 0.05, this finding is substantial.
In 11 individuals, the cervical lordosis was restored to a 20 - 40 degree angle. In the immediate post-operative time, five of them were pain-free, whereas the other six had varying degrees of pain (the p-value is 0.473812). This finding is not statistically significant (p 0.05). In the case of radicular pain, 7 patients were pain-free following surgery (the p-value was 0.73244). This finding is not statistically significant (p 0.05).
If we consider that the pain is negligible at level 0-1-2, here results become very significant in term of the relationship between the restoration of the cervical lordosis and clinical improvement of pain, the p-value is 0.026494. With a p value of 0.5, this result is significant.
NDI improves in all patients in a deferent rate.
4. Discussion
Cervical degenerative disease is frequently associated with cervical and/or radicular pain. Although radicular pain improves dramatically very quickly after surgical decompression [6] [7] , axial cervical pain may persist. This early axial pain necessitates prompt medical and physical management.
The visual analog scale (VAS) is commonly used to assess pain, whereas the neck disability index (NDI) is used to assess the impact of pain on personal activity [8] .
In our study, we chose 18 patients between the ages of 36 and 64 who all had multiple levels of degeneration in their cervical spine, resulting in cervical canal stenosis and both radicular and axial pain. These patients had an abnormal cervical lordosis prior to surgery and underwent surgical decompression and fusion of two, three, or four levels using zero profile cages by anterior approach.
Regardless of the restoration of cervical lordosis, we achieved a significant improvement in both radicular and axial pain in our selected patients during the early follow-up period (Table 1, Table 2). Similar results as good pain relief had
![]()
Table 1. Improvement of radicular pain after surgery.
The chi-square statistic is 8.6897. The p-value is 0.0032. This result is significant at p < 0.05.
![]()
Table 2. Improvement of axial pain after surgery.
The chi-square statistic is 7.2. The p-value is 0.00729. This result is significant at p < 0.05.
previously been reported in the literature, but only over a long period of time and at a different level of surgery [9] [10] .
Normal cervical lordosis is related to the overall balance of the spine [11] , and it is measured between C2 and C7 and is estimated to be around 34 degrees [11] , the mechanisms that keep this balance in place have been linked to the C7 and T1 slopes. The C7 slope, which connects the occipitocervical and thoracolumbar spines, is a useful marker of overall sagittal alignment [12] .
After a cervical fusion, radiological and clinical outcomes revealed that a kyphosis of 20 degrees or a decrease in sagittal lordosis after surgery are significantly related to cervical pain complaints [13] [14] .
Many techniques for decompressing and aligning the spine were described, including the use of cages or wedged interbody grafts [15] . The anterior approach to cervical fixation was described for the first time by Robison and Smith, as well as Clowards. [16] [17] , this method can correct 11 - 32 degrees of kyphosis [18] . According to some authors, the anterior approach results in less cervical lordosis correction than the posterior approach [19] . However, posterior instrumentation alone is ineffective in restoring cervical lordosis; it only serves to reduce the degree of kyphosis [20] .
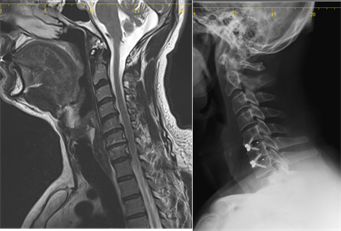
In our group of patients, the initial X-ray revealed that all patients had abnormal cervical lordosis (inclusive criteria), with either a straight neck or cervical kyphosis (Table 3). After surgery, the sagittal alignment was corrected in 11 patients, and these abnormality ratios improved in 61 percent of patients (Table 4). Hu et al. reported a successful cervical curve correction in 41% of deformed patients [21] .
To maintain normal balance and minimize demand on the posterior cervical muscles, the normal weight bearing axis is located posteriorly to the cervical vertebral body [22] .
In the normal population, flexion begins at C6C7 and extension begins at the lower cervical spine (C4C7) [22] . Any changes may result in a different load on the vertebrae, resulting in pain. It appears that having lordotic alignment affects the cervical spine’s flexion extension dynamic [4] [5] . In patients with a straight curve or a kyphotic spine [23] , the gravity center shifts anteriorly, causing axial pain. This axial pain could be due to more than just poor alignment and kyphosis, but also to an associated myelopathy, adjacent segment degeneration, and pseudo arthrosis [24] [25] .
![]()
Table 4. The alignment after surgery.
To maintain normal balance and minimize demand on the posterior cervical muscles, the normal weight bearing axis is posterior to the cervical vertebral body [22] .
In the normal population, flexion begins at C6C7, while extension begins at the lower cervical spine (C4C7) [1] . Any changes may result in a different load on the vertebrae, causing pain. It appears that having lordotic alignment affects the flexion extension dynamic of the cervical spine [4] [5] . In patients with a straight curve or a kyphotic spine, the gravity center shifts anteriorly, causing axial pain. This axial pain could be caused not only by poor alignment and kyphosis, but also by an associated myelopathy, adjacent segment degeneration, and pseudo arthrosis [24] [25] .
Despite the fact that some authors demonstrated that post-operative cervical alignment does not correlate with patients’ clinical and neurological improvement.
Kawakami et al. discovered that correcting the sagittal balance could result in a significant clinical improvement in patients with myelopathy and degenerative cervical spine [4] . Furthermore, Hu et al. and Moustafa et al. [21] [26] discover that correcting the alignment after one or two levels of fixation can improve the outcome of axial pain.
Both radicular and axial pain have been reported to be significantly improved following multilevel cervical spine surgery.
After a tree level fixation, Papadopoulos and all [18] reported an excellent improvement of 83 percent. Hu and all reported a significant hight level of long term improvement of the axial pain after the alignment was restored [21] .
From these evidences we conclude that the surgical correction of the cervical curve may also lead to an early improvement of the common post-operative complain of axial pain.
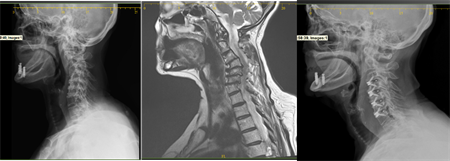
restored cervical spine.

restored cervical spine.
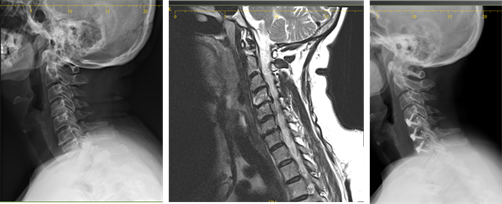
unrestored cervical spine.
unrestored cervical spine.
All of the patients in our group had ACDF for 2, 3, or 4 levels.
To minimize dysphagia, cages equipped with screws (zero profile) were used to ensure stability. Cages were chosen after the neck was positioned in normal lordosis and the endplates were adapted to receive these cages using the height speed burr.
We re-estimated axial and radicular pain in both groups of patients, restored and non-restored, after surgery.
Although the majority of patients experienced pain relief (Table 1, Table 2), we were unable to identify any significant relationship between the restoration of the cervical spine curve and pain relief in the early postoperative period, which lasted between 1 and 3 weeks (Table 5, Table 6).
When the pain at level 0-1-2 is accepted as negligible, here the relationship between pain improvement and restoration of the cervical curve becomes significant (Table 7).
![]()
Table 5. Surgical restoration and axial pain.
The p-value is 0.473812. This result is not significant at p < 0.05.
![]()
Table 6. Surgical restoration and radicular pain.
The p-value is 0.73244. This result is not significant at p < 0.05.
![]()
Table 7. Surgical restoration and negligible axial pain.
The p-value is 0.026494. This result is significant at p < 0.05.
Hu et al. [21] demonstrated that NDI improved after surgery. In our study, all patients improved their cervical activity after surgery, particularly in the restored group, but without statistically significant rates.
5. Conclusions
Even though restoring normal cervical lordosis has been recommended to prevent or minimize long-term axial pain in patients with cervical degenerative disc disease who underwent decompression with ACDF for one or two levels, it appears that this axial pain may not be improved in the immediate or early postoperative period when it is performed in multiple levels degenerative cervical spine.
This results in more involved medical and local management of the anticipated pain, as well as the patient’s assurance of a better prognosis in the coming months.