Investigation on the Distribution of Common Thalassemias in Various Cities and Counties under the Jurisdiction of Chongzuo City, Guangxi ()
1. Background Introduction
Thalassemia is a relatively rare congenital anemia disease. Thalassemia is divided into four types: α, β, δβ and δ, among which α and β-thalassemia are more common [1] [2] [3] [4]. The disease is widely distributed in many parts of the world, and Southeast Asia is one of the high-incidence areas. It is more common in Guangdong, Guangxi, and Sichuan in my country; Sporadic cases are found in provinces south of the Yangtze River, and rare in the north [5] [6]. According to reports, the incidence in Guangxi: α-thalassemia 17.5%, β-thalassemia: 6.43% [7] [8] [9]. Chongzuo City currently has no relevant statistics. In patients with this symptom, the bead protein chain in the body will be insufficient or even lacking, which will directly cause the structure of human hemoglobin to change, which will affect the carrying capacity of the normal oxygen and cause functional impairment such as liver and spleen [10] [11] [12] [13]. At present, there is no medical method to treat the disease. Therefore, patients with severe thalassemia often die unfortunately in infants and young children, but this disease can still be effectively prevented [14] - [19]. Therefore, in terms of marriage, doctors provide medical advice to patients with positive family history; While, premarital examination and prenatal genetic diagnosis of the fetus, and prenatal diagnosis using genetic analysis can diagnose severe α and β-thalassaemia fetuses during pregnancy. The timely termination of pregnancy to avoid the occurrence of fetal oedema syndrome and the birth of patients with severe β-thalassemia is currently an effective method to prevent this disease [20] [21] [22]. Therefore, carrying out population census and genetic counseling are of great significance to the prevention of this disease. In order to understand the distribution of thalassemia in various cities and counties of Chongzuo City, this study selected samples from various cities and counties from May 2014 to December 2020 for genetic testing. The results are now reported as follows.
2. Materials and Methods
2.1. Research Subjects
This study intends to use the method of case-control analysis to conduct thalassemia gene analysis on 21,535 venous blood samples of patients suspected of thalassemia through routine blood screening collected from May 1, 2014 to December 31, 2020. All cases are signed and confirmed with the consent of the patient or guardian, and will be implemented after discussion and approval by the Medical Ethics Committee of this hospital.
2.2. Screening Method
The venous blood of the patient shall be screened according to the requirements of blood routine, blood type and hemoglobin electrophoresis. Any abnormality shall be tested for thalassaemia gene according to the doctor’s recommendation. If one party is diagnosed with thalassaemia, even if the screening result of the other party is normal, the genetic test of the same type of thalassaemia is required. If both parties are carriers of the same type of thalassemia gene, amniocentesis will be performed for genetic prenatal diagnosis from 16 to 24 weeks of gestation.
2.3. Gene Detection Method
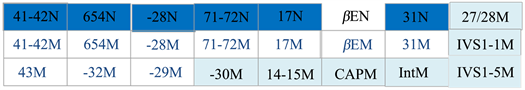
Genetic testing of deletion α-thalassemia was performed by GAP-PCR (--SEA, -α3.7, -α4.2 etc.). Mutations in the non-deletion α-thalassemia gene (αCS, αWS etc.) and β-thalassemia gene were tested by PCR-reverse point hybridization.
2.4. Interpretation of the Results of Thalassaemia Genetic Testing
2.4.1. Interpretation of Test Results for Deletion of α-Thalassaemia Gene
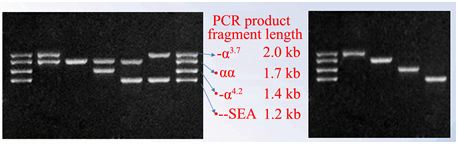
M DNA Markers Result judgment
1) αα/-α3.7 Heterozygote
2) αα/αα Normal
3) αα/-α4.2 Heterozygote
4) αα/--SEA Heterozygote
5) -α3.7/--SEA Double heterozygote
6) -α3.7/-α3.7 Homozygous
7) αα/αα Normal
8) -α4.2/-α4.2 Homozygous
9) --SEA/--SEA Homozygous
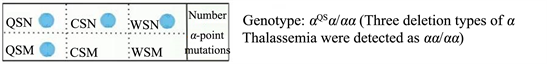
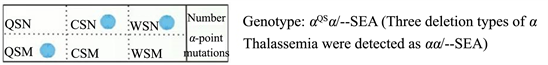
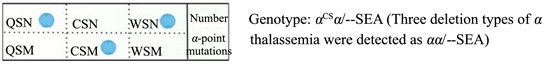
2.4.2. Interpretation of the Results of Non-Missing α-Thalassaemia
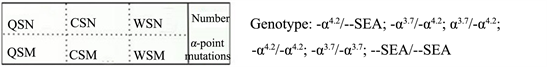
2.4.3. Interpretation of β-Thalassemia Gene Diagnosis Results

2.5. Instruments and Reagents
The nucleic acid extractor adopts the nucleic acid extractor Lab-Aid820 and Lab-Aid824s produced by Xiamen Zhishan; the thermal cycler adopts the T100 type produced by Bo Le; the electrophoresis instrument adopts the Bio-rad electrophoresis instrument produced by Bo Le; Hybridization instrument adopts YN-H96 automatic nucleic acid molecular hybridization instrument produced by Yaneng Biological Company. The reagents use the supporting reagents of the corresponding equipment. All reagents are used within the validity period; they participate in the quality evaluation activities of the National Clinical Laboratory Center every year, and all items are qualified.
2.6. Statistical Analysis
The SPSS22.0 statistical software was used for statistical analysis; the statistics of counting units used the chi-square test; the statistics of measurement units used the t test, and P < 0.05 was considered statistically significant.
3. Results
Venous blood samples collected from outpatients and inpatients in our hospital from 2014 to 2020 and sent from counties and districts to test for thalassemia genes, a total of 21,535 cases, including 6148 cases in Jiangzhou District (including our hospital), and there are 2318 cases of alpha-thalassemia gene positive, accounting for 37.70% of the people screened, 896 cases were positive for β-thalassaemia gene, accounting for 14.57% of the people screened, 464 cases were positive for αβ double gene, accounting for 7.55% of the people screened. 2470 cases were negative, accounting for 40.18% of the screened population; 2852 cases in Daxin County, and 1337 cases were positive for α-thalassaemia gene, accounting for 46.88% of the screened population, and 457 cases were positive for β-thalassaemia gene, accounting for screened 16.02% of the people checked; 175 cases were positive for both α and β; accounted for 6.14% of the screened persons, and 883 were negative, accounting for 30.96% of the screened persons.3291 cases in Fusui County, 1372 cases were positive for α-thalassaemia gene , and accounting for 41.69% of the screened population; 456 cases were positive for β-thalassaemia gene, and accounting for 13.86% of the screened population, 125 cases were positive for αβ; accounting for 3.79% of the screened population, and 1338 cases were negative, accounting for 40.66% of the people examined. 2354 cases in Tiandeng County; 1144 cases were positive for the α-thalassaemia gene, and accounting for 48.60% of the screened people; 430 cases were positive for the β-thalassaemia gene, and accounting for 18.27% of the screened people; 109 cases were positive for both α and β-thalassaemia which accounted for 4.63% of the screened population; 671 were negative, and accounted for 28.50% of the screened population. There were 3249 cases in Longzhou County, and 1465 cases were positive for α-thalassaemia gene, accounting for 45.09% of the screened population; 512 cases were positive for β-thalassaemia gene, accounting for 15.76% of the screened population; α and β were positive for all cases. 187 cases, accounting for 5.75% of the screened population, 1085 cases were negative, accounting for 33.40% of the screened population. There are 2507 cases in Ningming County, 1234 cases were positive for α-thalassaemia gene, accounting for 49.22% of the screened population; 491 cases were positive for β-thalassaemia gene, accounting for 19.59% of the screened population, and 157 cases were positive for α and β, accounting for 6.26% of the screened population, and 625 negative cases, accounting for 24.93% of the screened population. There were 1134 cases in Pingxiang City, 585 cases were positive for α-thalassaemia gene, accounting for 51.59% of the screened persons, 222 cases were positive for β-thalassaemia gene, accounting for 19.58% of the screened persons, and 79 were positive for α and β which accounting for 6.96% of the screened population, 248 negative cases, and accounting for 21.87% of the screened population. According to the chi-square test of multiple rate or composition ratio, the comparison of the distribution of the thalassaemia gene test results in each city and county, χ2 P = 0.0000, the difference is statistically significant. See Table 1 below for details.
4. Discussion
Thalassemia is a relatively rare congenital anemia disease. In terms of the
![]()
Table 1. Distribution of the results of thalassaemia gene testing in each district of Chongzuo City.
Note: According to the comparison of multiple rate or composition ratio, χ2 = 472.6917, P = 0.0000.
prevalence in my country, it is more common in the south. In patients with this symptom, the globin chain in the body will be insufficient or even lacking, which will directly cause the structure of human hemoglobin to change, which will affect the normal oxygen carrying capacity and cause damage to functions such as liver and spleen [23] [24] [25] [26]. Generally speaking, if two thalassemia patients with the same type married, there is a chance of giving birth to severe anemia patients. To effectively prevent the disease, blood is required for genetic analysis. If it is confirmed that they belong to type β, the children will have a fourth chance of being completely normal, a second chance of becoming mild anemia, and a fourth chance of becoming medium or severe anemia [27] [28].
In view of the lack of radical cure for the disease and poor clinical manifestations of moderate and severe prognosis, doctors should make medical advice to patients with positive family history or marriage, and conduct premarital examination and prenatal genetic diagnosis during early pregnancy, to avoid the occurrence of the next generation of children.
Medthalassaemia is completely preventable, and the key is early screening for genetic carriers. According to reports, one out of every nine people in Guangdong carries the thalassaemia gene. Some Cantonese people have a long-term bad complexion, which may be the cause of mild thalassaemia. They have almost no symptoms and can be regarded as normal people and do not need treatment. However, if both husband and wife are carriers of the thalassaemia gene, they may give birth to severe thalassaemia children [29] [30] [31] [32] [33]. Therefore, it is very important to screen for thalassaemia before pregnancy. The easiest thing is to do a routine blood test during the premarital examination or pregnancy examination. If the wife’s average hemoglobin volume (MCV) is lower than the normal value, she may be a carrier of the thalassemia gene, and the husband should also go to the hospital for examination as soon as possible. Those who have thalassemia in the family, have had a stillbirth, and both spouses have low MVC are all high-risk groups of thalassemia. In addition to routine blood tests, hemoglobin electrophoresis screening and genetic diagnosis should also be done. Even if there is no premarital examination and pregnancy check, and the pregnant woman is found to be a carrier of the thalassaemia gene during the prenatal screening, it can still prevent the crisis from happening. The spouse of a pregnant woman should go to the hospital for examination as soon as possible. If both parties are found to be carriers of the same type of thalassaemia gene, the fetus has a 1/4 chance of being normal, and a 1/2 chance of being a gene carrier (that is, thalassaemia mild). There is a 1/4 chance of being severe thalassaemia. Next, the prenatal genetic diagnosis can be performed for the fetus in the pregnant woman’s abdomen by drawing amniotic fluid or umbilical cord blood. If the genetic diagnosis finds that the fetus is normal or thalassaemia mild, the pregnancy can be continued. If the fetus is found to have thalassaemia intermediate or severe, the doctor will advise the pregnant woman to terminate the pregnancy [34] [35] [36].
In accordance with the principle of “check everything”, this study provides citizens with thalassemia genetic testing to reduce the birth of children with severe thalassemia in Chongzuo City; Block new cases to reduce the burden of treatment, and prevent poverty caused by illness. Grasp the incidence and distribution of the α and β thalassemia in this city. Form evaluation conclusions and put forward medical guidance opinions. To provide to the health authorities for better prevention and control of thalassemia in their jurisdiction.
Results of this study showed that among 21,535 suspected thalassemia samples collected, 9455 α gene deletion or point mutation were screened by genetic diagnosis, accounting for 43.91% of the total screened. 3464 cases were point mutations in the β gene, accounting for 16.09% of the total screening; 1296 cases with positive αβ genes, accounting for 6.02%; 7320 negative cases, accounting for 33.99%; the total number of positive cases was 14, 215 , accounting for 66.01% of the total screening population. From this result, it can be seen that the incidence of thalassemia is still relatively high in all cities and counties under the jurisdiction of Chongzuo City, which should arouse the attention of relevant departments. In addition, the incidence of thalassemia varies from city to county in Chongzuo City. According to the comparison of multi-rate or composition ratio, the incidence of thalassemia in each city and county has a significant difference, P < 0.001. This requires that we must pay attention to supervision, and guide relevant departments to prevent and treat diseases based on key inspections in key areas to reduce the incidence of thalassemia as much as possible, and give the next generation a healthy body.
5. Conclusion
The results of this study showed that the incidence of thalassemia in the gene detection results of suspected thalassemia samples in Chongzuo city was high, up to 66.01%, which should be paid close attention by relevant departments. In addition, the incidence of thalassemia was unbalanced among cities, counties and districts of Chongzuo city, and the comparison of multiple rates or constituent ratios was P < 0.001, which required the relevant health authorities to have targeted supervision to achieve the purpose of disease prevention and treatment. Thalassemia major is a tragedy for a family, requiring a lot of money to prolong life, and ultimately failing to change the situation. It is suggested to timely screening, timely diagnosis and medical consultation in married childless families and early pregnancy to reduce the birth of children with severe thalassaemia and avoid the occurrence of tragedy.
6. Limitations of the Study
The source of the cases in this study is only in Chongzuo City, Guangxi. The results of the study only represent the situation in Chongzuo area, and cannot represent the situation in other regions or the whole country, which has certain limitations.
Acknowledgements
In the research process of this subject, we have received strong support and help from many departments and individuals, as well as other researchers who did not participate in this subject. Here, all the members participating in this research express their deepest gratitude and wish them good health and all the best.
Fund Project
Scientific Research and Technology Development Project of Chongzuo City, Guangxi (NO. Chongke Attack 17122603).
NOTES
*Co-First author.
#Corresponding author.