Appropriateness of a Physiotherapic Treatment Protocol for the Axillary Web Syndrome, Applied in a Territorial Rehabilitation Service: Description of a Clinical Case ()
1. Introduction
Breast neoplasm is the most common form of cancer among women. Currently in Italy over 37,000 new cases are diagnosed per year [1] [2] 25% of which women below 50 years of age [3].
Axillary surgical procedures have reported, along with post-operative morbidity of bleeding, infections, presence of lymphedema and shoulder pain, also the axillary fibrous banding syndrome, better known as axillary web syndrome (AWS).
AWS normally appears between the first and the fifth week after surgery [4] [5] [6] diagnosed on 28.86% of women [7] [8].
The manifestation AWS is mainly at the level of axillary region at surgical dissection, but it can also extend towards the elbow and most serious cases, up to the column of the thumb [9] [10] with upper limb functional deficits [11].
L’AWS presents as a single cord or multiple thin cords in the subcutaneous tissues of the axilla. The cords frequently result in abduction shoulder pain and limited range of motion.
It presents as a tight subcutaneous cord in the axilla.
It can be associated with later lymphedema in a minority of patients.
L’AWS most frequently becomes symptomatic between 2 and 8 weeks postoperatively but can also develop and recur months to years after surgery.
Physical therapy and exercise can reduce pain and increase range of motion.
Education about and awareness of AWS should be promoted for both patients and providers, and regular assessments for AWS should be initiated by health care providers [12].
2. Case Report
The patient is a 69-year-old woman, retired ex-employee, with surgical outcome of right quadrant and right axillary lymphadenectomy because of sentinel lymph node’s positivity.
The anamnesis furthermore presents a picture of a pharmacologically controlled hypertension, digestive disorders and a clinical history following a surgery done 20 years ago for cholecystectomy.
The patient is address to the territorial rehabilitation service because of her right shoulder pain, specifically in axillary area and the scapula, limiting most of the normal activities of daily life with the presence of lymphatic vessels’ fibrosis at the brachial level, further confirmed from the STAWS questionnaire v.2.1 [13].
During the objective examination, the patient has a functional limitation with an active movement preserved up to 80˚ of abduction and 130˚ of elevation with the presence of pain in the last degrees of the movement.
The cervical spine has been evaluate and excluded as a factor contributing scapula pain.
Cervical mobility was painless and normal on all its planes of movement as well as the cervical radiculopathy identified through upper quadrant tests [14] was absent, the movement and the strength of the right elbow were normally preserved and pain free.
Hypo mobility from the fourth vertebra (D4) to the seventh vertebra (D7) was present at the anterior-posterior vertebral dorsal segmental test of mobility [15].
The description of this clinical case is to create an appropriate physiotherapy protocol to deal with patients having AWS in a rehabilitation service, through an active and passive manual therapy of the upper limb and dorsal cervical junction (MAP) together with self-mobilization exercises to do at home (EA), both established the MAP+EA protocol (MAPEA).
The patient was aware about her clinical condition, as well as had clarifications about her case study.
After agreeing to the publication, she signed a free and informed consent form.
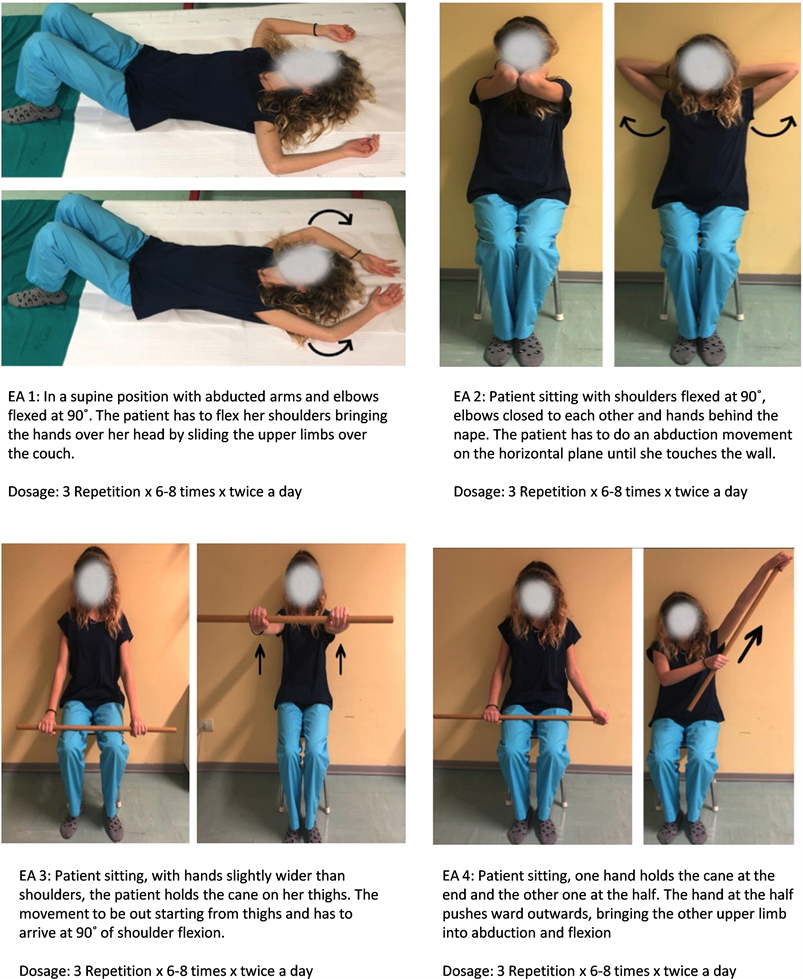
Treatment timeline Taking charge of MAPEA treatment in the territorial rehabilitation service lasted two months, where the patient underwent the MAP protocol. The protocol provided two biweekly sessions lasting 45 minutes, with the addition of EA protocol to execute out twice a day for the duration of 20 minutes for the entire duration of MAP. The follow up was does at 3 months after the last treatment session. Therapeutic interventions The MAP treatment consisted into passive and active mobilization the shoulder joint in supine position until reaching the pain limit in all its planes. The stretching passive muscular chains of the upper limb combined with breathing and mobilization of the scapula in lateral decubitus. The transversal mobilization of soft tissues, around the scar along the direction of the minor mobility without both of pain, burning and itching. Once carried out the work at upper limb level, II and III degree Maitland mobilization [16] of the dorsal cervical junction was realize. The EA protocol provided for a four exercises of self-mobilization to practise at home (Appendix), after the patient had been trained by the physiotherapist at the end of the first session of the first MAP treatment.
3. Discussion
The patient collaborated for the entire duration of the work protocol both in time dedicated to evaluation and MAPEA treatment.
The scales considered is Constant-Murley (C.M.S.) [17] [18] [19]; numerical rating scale (N.R.S.); and EuroqoL (EQ-5D), tool that allows measuring the interviewees health status and their quality of life, because of which it is possible to evaluate the health care provided [20].
The outcome assessment tools were administer before the start of treatment (T0), at the end of the last treatment session (T1) and at follow-up.
The collected data they were analysed and reported in Table 1: in the particular case, there was between T0 and T1 improvement in percentage of 43%, N.R.S. scale of 59%, C.M.S. scale and 81% in EQ-5D questionnaire, while in follow-up phase of 75% on the N.R.S scale, of 27% on C.M.S. and of 23% on EQ-5D (Figure 1).
Key: N.R.S.: Numerical Rating Scale, EQ-5D: Euroqol.
![]() Key: T0: Beginning of treatment, T1: End of treatment, Var.: Variation.
Key: T0: Beginning of treatment, T1: End of treatment, Var.: Variation.
Figure 1. Graphic representation of the score of outcomes, with the percentage change (%) of improvement between T0 and T1 and T1 and follow-up.
The descriptive analysis has highlighted as the improvement variation at follow-up was did not so high at C.M.S and especially at EQ-5D compared to the outcomes obtained during T1. This result could derive from the fact that the patient was not being treat with MAPEA protocol during the time elapsed between T1 to follow-up, but she carried out just the EA protocol.
This is a noteworthy aspect and it should be take into account, given that it is widely acknowledged to all rehabilitation health professionals that it is essential having a high level of life’s quality in order to keep good levels of rehabilitation assistance.
The Axillary web syndrome (AWS) is became increasingly recognised as consequence of breast cancer treatment. There are currently no formal guidelines on which to base therapy interventions.
The Physiotherapy intervention for these patients may prove beneficial in limiting subsequent shoulder dysfunction.
This case provides evidence that early physiotherapy intervention may lead to a quicker resolution of symptoms and pain shoulder with improvement quality of life.
The Physiotherapy intervention for these patients may prove beneficial in limiting subsequent shoulder dysfunction. Further research is needed to develop a standardised treatment approach for AWS.
4. Conclusion
In literature, there are few works focus attention on the rehabilitation management of the AWS and the clinical case here described could be consider as a tangible model of reference to represent a strategy to further increase works with efficacy tests and range of greater recommendations. The purpose is to device appropriate programs of rehabilitation care in line with what right now appears to be the assistance model for people affected by oncological disease, based increasingly on patient’s attention and involvement aimed at improving the quality of life [21].
Acknowledgements
The authors would like to thank Dr. Ilenia Bardelli for her assistance in giving professional enrichment notions concerning cancer related Lymphedema.
Appendix: Self-Treatment Exercises Protocol, “EA”